
It’s 10:47 p.m. You just left the library after a 12‑hour USMLE grind. Your group chat is dead, your family is two time zones away (and frankly doesn’t really “get” what you’re going through), and you walk back to your apartment knowing this: if you completely fall apart tonight, there is no one in this city who really has your back.
That’s the situation this is for.
You’re in medical school. Stress is baked into your life: blocks, OSCEs, Step, shelf exams, clinical rotations. But you don’t have a built‑in support system where you are. Maybe you:
- Moved states or countries and know nobody.
- Have family who are unsafe, invalidating, or just unavailable.
- Are estranged from home completely.
- Have “friends” around but nobody you trust with the real stuff.
And yet, you still have to show up to anatomy lab. Or pre‑round on patients. Or sit in a freezing exam room and remember the coag cascade.
So here’s the point: you cannot wait for a perfect support system to magically appear. You need a local mental safety net. Something that holds when you’re not okay at 2 a.m. on a Tuesday.
I’m going to walk through exactly how to build that, step by step, like you’d build a treatment plan.
Step 1: Accept Your Actual Situation (Not the Fantasy Version)
You can’t fix what you keep pretending isn’t a problem.
If your inner narrative is: “I should be able to do this alone” or “Once this exam is over I’ll be fine,” you’ll keep white‑knuckling until you burn out. I’ve seen too many students hit that wall in M2 and then just keep crashing through rotations.
Be blunt with yourself:
- “I do not have reliable emotional support where I live.”
- “If I had a crisis tonight, I don’t know who I’d call.”
- “My family is not a safe place to land right now.”
That’s not self‑pity. That’s assessment. Like noting vitals before you decide what to do next.
Once you name it, you can treat “lack of support” as a real risk factor—just like poor sleep, financial stress, or chronic illness. Not a moral failing. A risk factor. And risk factors get management plans.
Step 2: Build an Immediate Crisis Plan (Bare Minimum Safety Net)
Before we talk about community and friendships and all the nice stuff, you need a floor. This is your plan for the 1–5% of the time when things are genuinely bad: panic attack, self‑harm thoughts, can’t stop crying, can’t function.
Write this down in one place. Not in theory. Actually written.
Your crisis card should have:
Emergency contacts (non‑negotiable)
- Local emergency number (911 in the U.S. or your country’s equivalent).
- Campus security / campus emergency line.
- National or regional crisis line (suicide hotline, text line, etc.).
- Hospital ED closest to you (name + address).
Institutional mental health resources
- Student counseling center number.
- “After‑hours” counseling or crisis line if your school contracts one.
- Your school’s wellness office contact.
- Deans you could email if you needed academic flexibility (name + email).
Personal “safe” options
- A classmate you could text “Hey, are you awake? Not okay” without needing a full explanation.
- A place on or near campus where you can go and not be alone (24‑hour study space, hospital cafeteria, chapel, etc.).
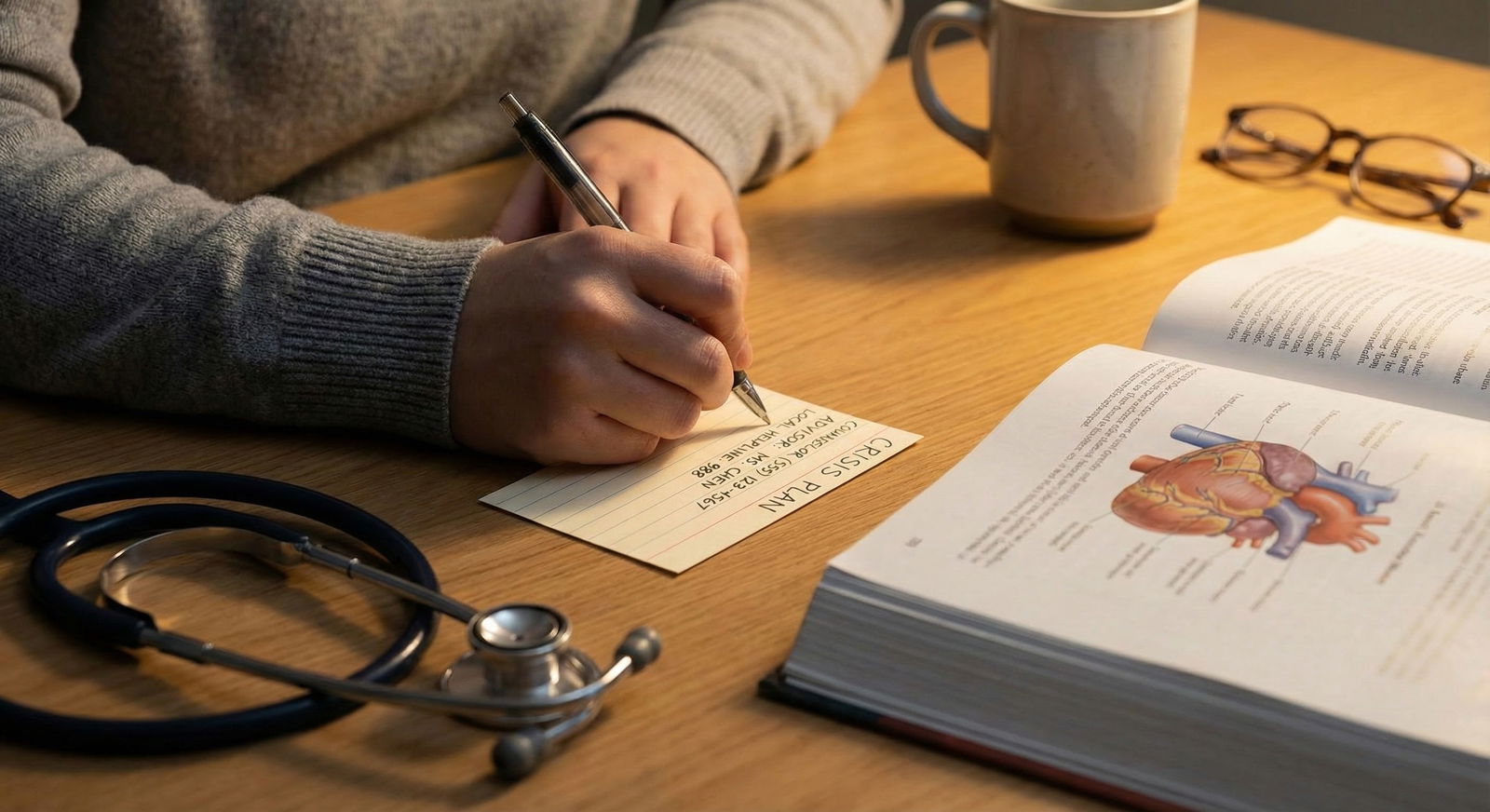
Lock this note on your phone home screen or print it and tape it inside your notebook. In crisis, your executive function is garbage. You want zero decision‑making.
If you’re thinking, “I’m not that bad, I don’t need this,” that’s like saying “my patient isn’t that hypotensive, they don’t need IV access.” You set it up before the crash.
Step 3: Audit What You Already Have (Even If It Feels Small)
People in your situation often say, “I have no support here.” That’s sometimes true. More often, what you actually have is fragmented, underused, or not‑yet‑safe support.
Do a quick inventory:
- Classmates you’ve had even one real conversation with.
- Residents/attendings who have said, “Email if you ever want to talk about this specialty or life stuff.”
- Peer mentors, big‑little pairs, learning community faculty.
- Student orgs you went to once and never back.
- Non‑med stuff: gym class teacher, barista you see daily, spiritual community, neighbor you small‑talk with.
Make a list, literally. Then label each:
- A: Could be emotional support (with some time).
- B: Could be practical support only (study help, logistics).
- C: Not for support (toxic, unsafe, too boundary‑crossing).
You’re not judging people. You’re sorting resources. Like triage.
Step 4: Create a “Layered” Local Support System
Think in layers, not “best friend who fixes everything.” You want redundancy. If one thing fails (friend is on call, therapy is booked, exam week chaos), something else can hold.
Here’s a simple mental model:
| Layer Type | Main Role | Example Resources |
|---|---|---|
| Professional | High-risk, ongoing | Therapist, psychiatrist |
| Institutional | School-specific issues | Counseling center, dean |
| Peer – Deep | Emotional support | 1–3 trusted classmates |
| Peer – Light | Daily connection | Group chats, study buddies |
| Community/Activity | Baseline well-being | Gym, clubs, faith groups |
Let’s break these into actual moves.
4A. Professional Support: Lock This In Early
If you have ANY history of:
- Depression, anxiety, self‑harm, trauma.
- Eating disorders, substance use, chronic insomnia.
- Or even just “I’ve been crying in the bathroom weekly…”
You should not be waiting until Step 1 to find a therapist.
Actions:
Use your student health coverage on purpose.
Ask directly: “Which providers are familiar with medical students / trainees?” Some cities around big med schools have therapists who practically specialize in you.Book recurring, not one‑off.
First intake, then push for a regular slot: every other week is fine. The goal is: when you hit a hard patch, you already have someone who knows your baseline.If the school counseling center sucks (many do):
- Use them for a letter/referral to external providers.
- Ask them specifically: “Who do med students often see in the community?”
- Use short‑term there while you search for long‑term elsewhere.
And yes, I know booking therapy during M2 or clerkships feels impossible. Book it like you’d book a mandatory lab. You move things around it, not the other way.
4B. Institutional Support: Know the People With Power
Your school isn’t your friend, but there are usually people inside it who can be allies.
Find out:
- Who is the assistant/associate dean of student affairs or wellness?
- Who handles leaves of absence or exam accommodations?
- Who runs the learning community / college system?
Then do something most students never do: meet them before you’re desperate.
Email: “I’m trying to be proactive about wellness during school. Could I set up a brief meeting to understand what kind of support exists if I hit a rough patch?”
You’re not trauma‑dumping. You’re doing reconnaissance.
Why this matters: when life blows up (breakup, health crisis, mental crash) you’ll already know:
- Who to email for an exam delay.
- How to ask for a lighter rotation.
- What language to use to not screw yourself with the promotions committee.
Step 5: Turn Classmates into Real Support (Without Oversharing)
You don’t need 20 close friends. You need maybe 2–4 humans locally who know you beyond “what did you get on UWorld today?”
You build that intentionally.
Actions you can start this week:
Upgrade one acquaintance by 10%.
Instead of “How are you?” / “Tired lol,” try:
“Honestly, I got wrecked by this block. Are you surviving or also falling apart?”
Slight vulnerability. Not your whole trauma file. Enough to see if they meet you there.Use predictable contact points.
- Weekly coffee after small group.
- Walk to parking together after lab.
- “Can we study together for this exam and at least complain to each other?”
Name the mental health reality out loud.
“Everyone keeps pretending this is fine. It’s not fine for me. How’s it really feeling on your side?”
People are waiting for someone to stop performing. You might be that person.Be the kind of support you want back—within limits.
Text after a hard exam: “Today sucked. I’m ordering takeout and rewatching something dumb. If you want to half‑brain this with me, you’re welcome.”
Low pressure. Clear door‑open.
You’re testing: who responds, who disappears, who consistently minimizes you (“we’re all stressed, you’ll be fine”)—those folks belong in your “not for emotional support” category.
Step 6: Use Non‑Med People Strategically
Here’s the trap: med friends understand the content but can also amplify the stress. Normal people often can’t fully understand, but they can calm you down and help you feel like a human again.
You want at least one or two non‑med anchors.
Where to find them:
- Group fitness or sports (people who see you weekly).
- Hobbies you had before med school: music, art, gaming, writing groups.
- Spiritual/faith communities if that’s your thing.
- Volunteering once or twice a month.

You don’t need these people to understand Step 2 CK. You need them to remind your nervous system that life contains things other than NBME questions.
Example script:
“I’m in med school here and it takes over everything. I really want one place where I’m not ‘the med student’ but just another person. That’s part of why I joined this.”
You’ve now given them permission to treat you like a whole person.
Step 7: Create a “Daily Baseline” Mental Health Routine (Local Version)
Support isn’t just people. It’s your environment and habits. You can’t teleport home to your childhood bedroom, but you can set up local rituals that keep you from mentally fraying.
Think in three buckets: body, mind, connection.
Body (stabilize your basic physiology)
- Sleep window you protect like an exam. Maybe it’s 11–6. Not perfect, but consistent.
- One movement anchor: 20‑minute walk after class, short run, yoga in your room.
- Food that doesn’t wreck you: Simple cheap meals you can default to when stressed (frozen veggies + protein + rice counts).
Mind (give your brain exit ramps)
- Pre‑bed rule: last 20 minutes, no Anki, no question banks. Just something that signals “not exam mode.” Fiction, short podcast, breathing app.
- Micro‑reset between tasks: genuinely 3–5 minutes of looking out a window, stretching, or walking a hallway without your phone.
Connection (micro‑social habits)
- One small human contact daily:
A text, a 1‑minute conversation, a meme to a friend. I’m not romanticizing loneliness; I’m saying complete isolation accelerates the spiral.
This stuff feels small until you stop doing it. Then you realize it was the only thing between you and being feral.
Step 8: Have a Plan for Exam Weeks and Rotations From Hell
Your mental safety net needs a “storm mode” for acute stress periods: big exams, surgery rotation, night float.

| Category | Value |
|---|---|
| Orientation | 3 |
| M1 Midterm | 6 |
| M2 Blocks | 7 |
| Step 1 | 9 |
| Core Rotations | 8 |
| Step 2 | 9 |
Storm mode means you pre‑decide:
What gets protected, no matter what
- Therapy appointment? Keep it. Exam stress is exactly when you need it.
- 10 minutes to walk around the block daily? Non‑negotiable.
What gets paused without guilt
- Optional meetings, extra research tasks, non‑critical group obligations.
Who you warn in advance
Text a close friend: “Hey, I’m going to be buried in Step prep next 2 weeks. If I go dark, it’s not you. I may need a reality check or meme dump day 10.”What you will not do to cope
Write this down. “I will not: pull 3 all‑nighters in a row, isolate completely for more than 48 hours, drink alone to sleep, stop all movement.”
You are not making this up on day 3 of a meltdown at 1 a.m. You’re writing it now, while semi‑sane.
Step 9: Digital Support That Actually Helps (Not Just Doomscrolling)
You can’t teleport your favorite people to your city. But you can weaponize your phone in a way that’s actually supportive.
There’s a right and wrong way to do this.
Use digital support intentionally:
- Schedule recurring video calls with a trusted person from home. Put them on the calendar like a class. “Every other Sunday at 8 p.m. we talk. No med school small talk only.”
- Curate one or two online communities (Discord, subreddits, group chats) that are supportive, not toxic brag pits.
Avoid:
- Pre‑bed doomscrolling in r/Step2 or hypercompetitive group chats that just worsen your anxiety.
- Trauma dumping into group chats that never respond; that just reinforces “nobody cares.”
If your family isn’t safe to talk to, create a chosen‑family thread. Three people you trust, even if they’re in different cities. Use that space for the “this week sucks and I need encouragement” messages.
Step 10: Know Red Flags That Mean “Use the Net Now”
Here’s where people screw up: they build some pieces of a safety net, then wait until they’re in full collapse before using it.
These are your activation thresholds. If any of these show up and last more than a few days, you use your supports:
- You’re thinking “If I got hit by a car and didn’t have to deal with this, that’d be a relief.”
- Passive or active thoughts of self‑harm, even if you’re “not going to act on it.”
- Can’t get out of bed for class multiple days in a row.
- Panic attacks, or feeling like you’re constantly on the verge of one.
- Not eating or bingeing consistently because of stress.
- Using alcohol/weed/sedatives daily just to get through.

| Category | Value |
|---|---|
| Sleep Issues | 80 |
| Irritability | 65 |
| Crying Spells | 50 |
| Numbness | 45 |
| Panic Symptoms | 35 |
If these hit, that’s not “try to be stronger” time. That’s:
- Email therapist / counseling center: “Symptoms worsening, need sooner slot.”
- Text one local person: “Not okay today, could we meet up or at least talk?”
- Use your crisis plan card if you’re feeling unsafe.
Step 11: What If Your Home Is the Problem?
Different level of difficulty, but common.
If your family is:
- Dismissive (“just toughen up”).
- Abusive (emotionally, physically, financially).
- Over‑controlling (threatening to pull support if you “show weakness”).
Then “going home for support” isn’t just unavailable—it’s actively dangerous.
Your priorities shift:
Emotional distance, even if you still rely on them materially.
That means you don’t bring them the rawest parts of your mental state. You treat them as you’d treat a difficult attending: polite, brief, low‑information.Build “chosen family” locally and digitally.
Friends, mentors, older residents, therapists—these become your primary emotional home.Plan long‑term for independence.
If they’re paying tuition or rent and using it to control you, part of your mental safety net is a multi‑year plan: scholarships, cheaper housing, part‑time work if realistic, social work or financial aid office consult.
You’re not going to fix your family while also surviving pharmacology. Protect yourself first.
Putting It All Together: A Simple Blueprint
Here’s a 30‑day build‑your‑net plan that doesn’t require your whole life to change.

| Step | Description |
|---|---|
| Step 1 | Day 1-3: Crisis Plan |
| Step 2 | Day 4-7: Resource Audit |
| Step 3 | Week 2: Book Therapy/Counseling |
| Step 4 | Week 2-3: Deepen 1-2 Peer Connections |
| Step 5 | Week 3: Join 1 Activity or Group |
| Step 6 | Week 4: Set Exam Storm Mode Rules |
| Step 7 | Ongoing: Adjust & Use Supports |
If you do nothing else, do these:
Week 1
– Write your crisis plan.
– Find and save your school’s mental health resources.
– Identify at least one person you could text on a bad day.
Week 2
– Book a counseling/therapy intake, even if you “don’t need it yet.”
– Ask one classmate to study/have coffee and be 10% more real than usual.
Week 3
– Start a small, sustainable non‑med activity locally.
– Set 2–3 “storm mode” rules for exam weeks.
Week 4
– Review what’s working. Add one more layer (non‑med friend, faculty mentor, or online support that doesn’t suck).
You’re not designing some perfect wellness program. You’re building a net that turns “free fall” into “hard landing, but survivable.”
FAQ (Exactly 5 Questions)
1. What if I genuinely don’t trust anyone in my class?
Then split your strategy: professional + non‑med + digital. Get a therapist (campus or community). Anchor yourself in one non‑med space weekly: gym class, religious group, art group, whatever. And build a chosen‑family text group from people outside your city—old friends, cousins, online friends you trust. You do not have to force intimacy with classmates who feel toxic or unsafe. Some classes are like that. Your mental safety net just leans more heavily on non‑class resources.
2. How do I ask a classmate for support without making it weird?
Start small and concrete. “This week’s been rough. Would you want to grab coffee after lab and just decompress?” Or: “I’m getting crushed by this block and it’s messing with my mood. Do you ever feel that?” If they respond with empathy, you can share a bit more over time. If they minimize or mock, you file them under “good for notes, not for feelings” and move on. You’re not proposing a marriage; you’re testing whether they can handle humanity.
3. I’m scared therapy could affect my future licensing. Is that real?
In most places, seeing a therapist alone does not tank your license. What boards care about is impairment—not the act of getting care. Many boards have already revised their questions to focus on current functional impairment, not past treatment. Get precise: read your state’s board wording, talk anonymously to your counseling center, or ask a trusted faculty member. Unmanaged mental illness is far more risky to your career (and safety) than documented treatment.
4. What if my schedule is too packed for all of this?
Then you ruthlessly prioritize. You don’t need ten things; you need a few non‑negotiables. For example: a 45‑minute therapy session every other week, a 20‑minute walk most days, and one real social interaction weekly. That’s under 3 hours total per week. Some rotations truly are brutal (surgery, nights), so you scale for those weeks—but you don’t go to zero. Going to zero is how people break.
5. How do I know if it’s time to consider a leave of absence?
If you’re consistently unable to function—missing multiple exams or required sessions, constant suicidal ideation, heavy substance use to cope, or your therapist/psychiatrist is telling you you need more time—that’s leave‑of‑absence territory. A LOA is not a moral failure; it’s an intervention to prevent long‑term damage. Talk to a mental health professional first, then to a student affairs dean you trust. You can rebuild academic progress; rebuilding from a full psychological crash is much harder.
Key points to walk away with:
- You cannot wait for “home” to fix things. You must build a layered, local safety net—professional, institutional, peer, and community—on purpose.
- A crisis plan, even when you feel “fine,” is non‑optional. You prepare the net before you fall.
- You don’t need perfect people or a perfect schedule. You need a few non‑negotiable supports and the courage to actually use them when the red flags start flashing.




















