The dirty secret is this: some program directors quietly flag applicants with a real mindfulness practice as “less likely to implode under pressure.”
Not “nice extra.” Not “cute wellness hobby.” A risk-reduction marker.
They’ll rarely say it out loud in a faculty meeting, and it will never appear in the official selection criteria. But it shows up in the side comments, the offhand remarks after interviews, the way certain applications get a second look when a PD is deciding who will actually survive their program.
Let me walk you through how this really works behind closed doors.
What PDs Actually Worry About (It’s Not Your Yoga Pose)
Behind the public talk about diversity, scholarship, and “fit,” program directors are obsessing over three things:
- Who is going to crack under pressure and create disasters—clinical, interpersonal, or legal.
- Who is going to drain faculty and chief residents with constant fires to put out.
- Who can function at 2 a.m. on post-call day 5 without becoming dangerous or toxic.
And they’re making these judgments with incomplete data: a test score, a few letters, a personal statement someone maybe edited to death, and 20–30 minutes in an interview.
So they search for patterns. Little tells that someone has internal tools, not just external performance.
A genuine, sustained mindfulness practice is one of those tells.
I’ve sat in rank meetings where a PD literally said, “That applicant who does meditation and retreats… they seemed oddly grounded for someone with their CV. I trust them more than the 270 robot.” No joke. It’s not that they care about meditation as a spiritual thing. They care about what it signals:
- You’re not purely driven by external validation.
- You’ve spent time watching your own mind.
- You have at least experimented with not reacting to every stressor.
Those traits matter more to PDs than another abstract on your CV, especially now.
Why Burnout Broke the Old Selection Game

| Category | Value |
|---|---|
| Clinical competence | 90 |
| Professionalism issues | 70 |
| Burnout/mental health | 80 |
| Interpersonal conflict | 65 |
| Duty hour violations | 40 |
Historically, the unspoken rule was: pick the highest scores and the hardest workers, and they’ll gut it out. The ones who struggled were dismissed as “weak” or “not cut out for this.”
That model quietly collapsed over the last decade.
Here’s what changed:
- Burnout is now a regulatory and financial problem. Residents quitting mid-year costs serious money and accreditation headaches.
- Trainee mental health crises are more visible. Suicides, leave of absence patterns, impaired physicians—PDs are getting called into offices over this.
- Patients are watching and complaining. An over-stressed, snappy resident is now a patient-satisfaction issue, not just an internal “coaching” matter.
So PDs started looking for something beyond raw horsepower. They still want horsepower—do not misread that—but they want adaptive horsepower. People who can modulate themselves under chronic stress.
Mindfulness, when real, is a proxy for that adaptability. It’s not magic. It’s a signal.
The Difference Between Real Practice and Wellness Theater
Let me be blunt: most “mindfulness” references in applications are garbage.
“I like mindfulness and yoga” slapped into the hobbies section.
“I’ve learned the importance of being present with my patients” as a throwaway line.
Or the worst: a cliché paragraph clearly stolen from a wellness blog.
Faculty can smell this a mile away.
The applicants who get quiet points for mindfulness look different:
- They reference specific practices or traditions: Vipassana, MBSR, Headspace, Insight Timer, body scan, noting practice.
- They talk about how they use it on call, during exams, or after bad outcomes—concrete, situational detail.
- Their demeanor matches the claim: slower speech when things get tense, genuine listening, not jumping to defend themselves.
In one IM program I know, a faculty member literally said, “He mentioned doing a 10-day Vipassana retreat. Anyone who voluntarily sits with their own mind that long can probably tolerate being cross-covered in the unit.”
Was he fully serious? Half. But half is enough to shift a rank by 10–20 spots.
What Mindfulness Signals to a PD’s Brain
Here’s the translation happening in a PD’s head that no one spells out for applicants.
1. Emotional Regulation Under Fire
They have seen too many residents who:
- Melt down when criticized.
- Get into petty wars with nurses and consultants.
- Spiral after a bad outcome and become functionally useless for days.
If they see evidence you’ve practiced watching your own thoughts and emotions without identifying with every one, they think:
“This person might not lose it when an attending tears them apart on rounds. They’ll feel it, but they’ll recover.”
The mindful applicant often answers stress questions differently:
“Tell me about a time you got difficult feedback.”
The standard applicant: “I took it constructively and worked harder.” (Empty.)
The mindful applicant: “My first instinct was defensiveness; I could feel my chest tighten. I’ve been working on pausing before reacting, so I took a day, reflected, then went back to ask specific questions.”
One line like that can shift a PD’s gut feeling.
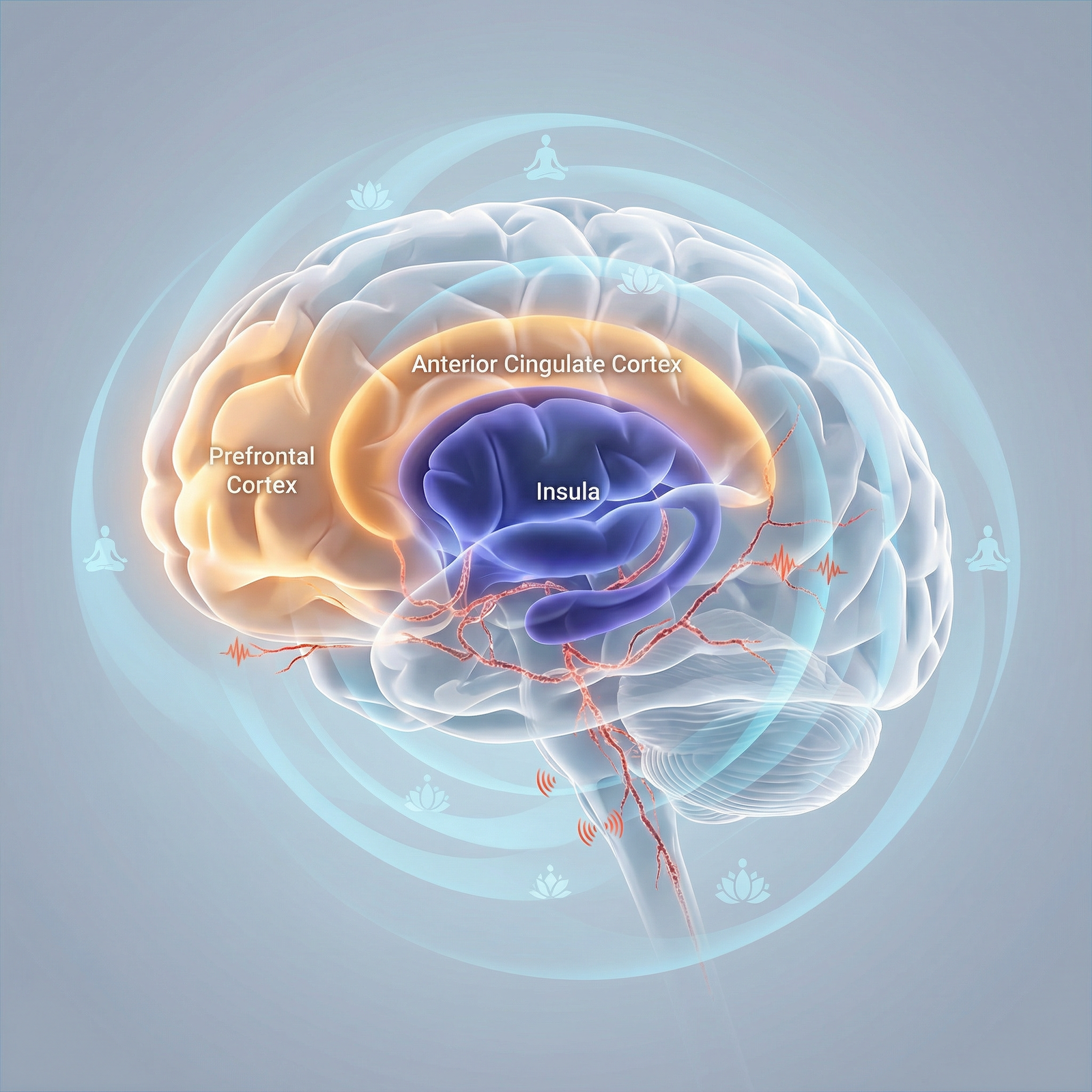
2. Attentional Control = Fewer Dangerous Mistakes
Mindfulness is basically attention training. Focus, re-focus, notice distraction, come back.
Residency is an environment designed to shred attention: pagers, alarms, EHR clicks, side conversations, fatigue. The resident who can hold a thread in their mind without being yanked by every noise is safer.
PDs don’t say, “We want meditators.” They say, “We want people who are meticulous and present at the bedside.” Same thing, in disguise.
I’ve watched faculty comment after an interview: “She had this way of pausing before answering, like she actually took in the question. I trust that more than the rapid-fire answers.” That “pause” is what long-term mindfulness practice looks like externally.
3. Lower Probability of Becoming an HR Problem
No PD wants to say this out loud, but it’s absolutely true: they’re screening for people less likely to generate HR complaints.
Residents who have at least some self-awareness are less likely to:
- Fire off explosive emails at 3 a.m.
- Snap at a nurse in front of a patient.
- Lash out at med students and create a toxic subculture.
Does mindfulness guarantee you won’t do those things? Of course not. But if you’ve practiced watching anger arise and not acting on it immediately, the probability drops.
Behind closed doors, the language is cruder:
“I don’t want another PGY-2 like last year, constantly in my office crying or furious. Give me the one who sits and breathes.”
Yes, that exact phrase has been said.
Where Mindfulness Shows Up in Your Application (When It Helps, When It Hurts)

You do not need to brand yourself as “the mindfulness person.” That can actually backfire if it feels like a gimmick or identity costume.
What works is integrating it as a background operating system that occasionally surfaces in concrete ways.
Personal Statement
Where it helps:
- A specific story: you had a panic reaction, you used a breathing or awareness technique to stabilize yourself enough to function, and you reflect honestly on that.
- Describing how mindfulness changed the way you show up for patients, not just how you “felt more present.”
Where it hurts:
- Grand claims like, “Through mindfulness, I have mastered my emotions.” Faculty will roll their eyes.
- Vague spirituality disconnected from clinical reality.
Interviews
This is where the signal really lands.
You do not need to say the word “mindfulness” even once to get the benefit. What faculty respond to is:
- That half-second pause before answering.
- The way you handle a challenging or slightly confrontational question.
- Your willingness to describe your own internal process without melodrama.
If you do explicitly mention mindfulness, keep it utilitarian and grounded:
- “I started a 10-minute daily meditation practice during second year because I noticed I was constantly running mental simulations of failure. It helped me see those as thoughts, not facts, which made studying more sustainable.”
That sounds like: mature coping, insight, no theatrics.
Letters of Recommendation
Where this secretly helps a lot: faculty describing you as “calm under pressure,” “reflective,” “takes feedback well,” “stable presence on the team.”
They don’t have to mention mindfulness at all. But guess what’s often behind that? Some kind of contemplative practice, even if you never paraded it around.
I’ve watched PDs scan letters and say, “I like that word—‘equanimous’—that’s rare in a LOR.” That one adjective did more than the list of conferences.
The Programs That Care About This (And the Ones That Pretend Not To)
Let’s be very clear: not all PDs care. Some still worship at the altar of raw metrics and call anything “soft” a distraction.
But the tide is shifting harder than you think.
| Program Type | Quiet Favorability for Mindfulness |
|---|---|
| Academic IM / Psych | High |
| EM / Anesthesia | Moderate |
| Surgery (traditional) | Low to Moderate |
| Primary Care–oriented FM/Peds | High |
| Malignant legacy programs | Very Low |
Then there’s the punchline: even in some hard-core surgical and EM programs, the savvy PDs are clocking who has emotional regulation skills, they’re just calling it something else—“grit with insight,” “self-awareness,” “coachability.”
One trauma surgery PD I know rolled his eyes at the word mindfulness. But when he watched interviews, he kept picking applicants who described some version of mental training. His chief later pointed out, “You realize half your top-ranked people mentioned meditation, journaling, or therapy?” He shrugged and said, “Yeah, I just don’t want screamers anymore.”
So even if the culture looks old-school macho on the outside, the selection filters are evolving.
How to Talk About Mindfulness Without Sounding Like a Wellness Brochure

| Step | Description |
|---|---|
| Step 1 | Personal Practice |
| Step 2 | Specific Experiences |
| Step 3 | Application Content |
| Step 4 | Personal Statement |
| Step 5 | Interview Answers |
| Step 6 | Letters by Mentors |
| Step 7 | Behavior on Rotations |
The worst thing you can do is parrot generic language. PDs and faculty have been force-fed “resilience,” “burnout,” and “mindfulness” slides at mandatory workshops for years. They’re numb to it.
Here’s how you sound like a grown, thinking person instead:
Use concrete, short examples.
“I started doing a 5-minute breathing practice before pre-rounds because I noticed I was showing up edgy and rushed. It helped me catch myself before snapping at people.”Be honest about imperfection.
“I still get anxious, but I catch it earlier now” is more convincing than “I stay calm in all situations.”Tie it to patient care.
PDs don’t care about your inner peace in a vacuum. They care about that inner peace when a family is screaming at you, or when you missed something on a lab and have to own it.
And then, importantly: drop it. Don’t over-sell. Let them connect the dots.
What a Real Practice Looks Like When You’re in Training

| Category | Value |
|---|---|
| Short daily sits | 60 |
| On-the-fly breaths at work | 50 |
| Longer weekly session | 30 |
| Retreats/courses | 10 |
| Informal awareness in daily life | 50 |
You do not need to sit on a cushion for an hour a day and attend three retreats a year to “qualify.”
Here’s what faculty recognize as real when residents describe it:
- 5–15 minutes most days of some intentional, non-distracted practice: breath, body scan, noting, or even mindful walking.
- Using micro-practices before or after emotionally intense events: codes, breaking bad news, being chewed out.
- A basic literacy of what’s happening in your own mind: “Oh, that’s shame,” “That’s anger,” “That’s catastrophizing.”
Residents who actually do this talk differently in supervision. They say things like, “I noticed I was clenching and mentally defending myself, so I paused,” instead of, “I don’t know, it just all exploded.”
And PDs hear that back-channel from attendings and chiefs. The informal narrative around you absolutely matters.
The Ethical Layer: Why This Belongs in Medicine at All

Let’s step out of the purely tactical for a second.
There’s a reason mindfulness has crept into ethics discussions and professionalism committees.
Being mindful is not just about your stress level. It changes:
- How quickly you react versus respond.
- How much space you create between an impulse and an action.
- How you hold moral distress: when you’re forced to discharge someone into a bad situation, or follow a family’s wishes you disagree with.
Ethically, a mindful clinician:
- Is less likely to dehumanize patients when burned out.
- More likely to notice when they’re practicing on autopilot and missing crucial cues.
- Better able to witness their own bias arising—and not automatically act on it.
Some PDs, especially in internal medicine, psych, peds, and palliative-heavy programs, are very aware of this. They’ve watched who crumbles under moral injury and who can stay present with suffering without numbing out or attacking others.
When they quietly favor applicants with a mindfulness practice, part of what they’re saying is: “This person may be able to face how ugly this can get without losing their humanity.”
That’s not a soft skill. That’s core medical ethics in the trenches.
What You Should Actually Do With This Information

Let me be clear on a few things.
Do not:
- Slap “I practice mindfulness” onto your application if you don’t, just because you read this. Faking it will show the second someone asks a follow-up question.
- Make mindfulness your whole brand unless it’s deeply authentic and backed by serious work (e.g., you’ve taught MBSR, done retreats, etc.).
- Expect mindfulness to rescue low scores, red flags, or poor clinical performance. It won’t.
Do:
- If you already have a practice, tighten it up. Make it regular. Make it real.
- Let that practice change how you show up on rotations: listening better, reacting slower, apologizing faster. Word of that travels further than you think.
- Mention it briefly and concretely in your application or interview if—and only if—it’s honest and clearly connected to how you function as a physician-in-training.
And then trust this: in some rooms you’ll never enter, your name will be on a slide, and someone will say, “I just feel like this applicant is stable.” If your mindfulness practice helped create that impression, it has already done serious work for your career.
FAQ
1. Will starting mindfulness right before applications actually help, or is it too late?
If you start four weeks before ERAS opens just to have a line to write about, no, that will not help. Faculty can tell when you’re describing a fresh, intellectual idea versus lived experience. But starting now—even if you’re late in med school or early residency—will absolutely change how you handle interviews, tough questions, and real-time stress. The benefits show up more in how you behave than what you claim.
2. Should I explicitly say “I do mindfulness meditation” on my CV or personal statement?
Only if it’s true, specific, and meaningful. Listing “meditation” under hobbies is fine but low-yield unless you can talk about it in depth. A brief, concrete mention in your personal statement or interview—tied to a real clinical or learning situation—is much more powerful. If you can’t back it up with clear examples of how it affects your work, leave the word out and let your presence speak for itself.
3. Will some PDs see mindfulness as soft or flaky and judge me negatively?
A few will, especially in more traditional or macho cultures. But even in those environments, what they really value is composure, resilience, and focus—all of which mindfulness builds. You don’t need to use the label. Just show the outcomes: calm under pressure, thoughtful responses, ability to handle feedback. The PDs who quietly care about mindfulness will recognize it. The ones who don’t will still appreciate the traits it produces.
Key points: mindfulness is not magic, but it’s a real signal; it must be genuine and grounded; and when practiced consistently, it gives you exactly the internal tools PDs are secretly praying their residents will have.



















