
The backchannel calls matter more than the glossy brochure or the ACGME approval letter. Programs live or die on those quiet conversations you’ll never hear.
Let me walk you through what really happens when a program director is deciding how to rank (or whether to trust) a brand-new residency program.
Everyone talks about case logs, didactics, and board pass rates. That’s surface level. The people actually deciding whether to send their residents, their graduates, their reputation into a new program’s orbit pick up the phone and start asking questions that never show up in any official document.
Who’s Calling Whom (and Why)
Here’s the part applicants never see: the first serious “rank or not” decision on a new residency program doesn’t happen in March. It happens months earlier, in quiet one-on-one calls between:
- Established program directors in the same specialty
- Department chairs
- Former co-residents and fellowship directors
- GME office leaders who’ve “seen this movie before”
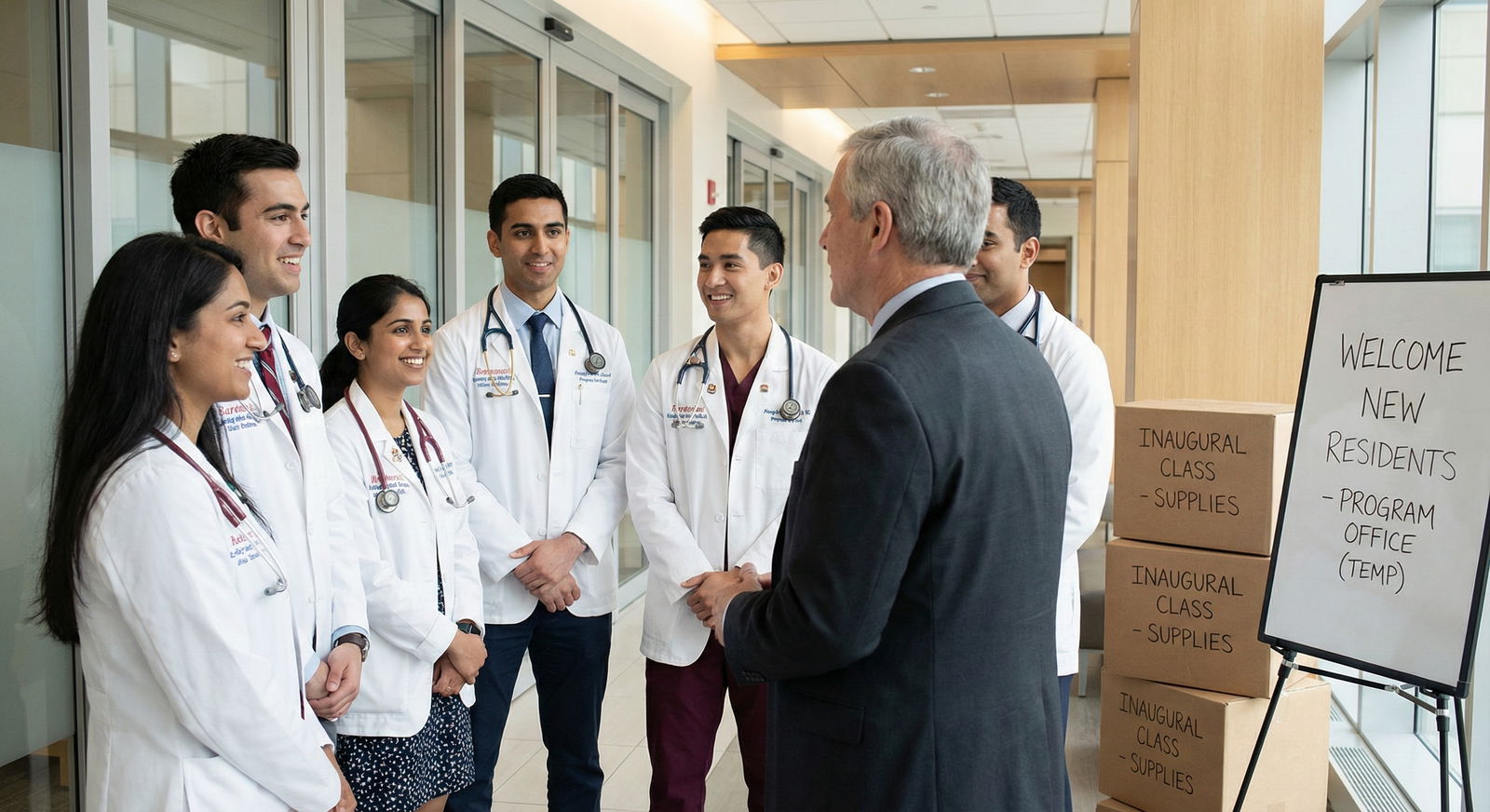
The newer the program, the more skeptical the established PDs. ACGME accreditation is considered the bare minimum, not a stamp of quality. So before they rank a brand-new program high enough to risk matching someone there, PDs start working the backchannel.
Typical scenario I’ve watched play out:
A new internal medicine program at a mid-sized community hospital gets initial accreditation. Slick website. Strong marketing. They tout “academic affiliation” with a big-name university hospital 45 minutes away.
Now it’s rank list season. An established IM PD at a nearby university program has a borderline applicant who might end up at this new place. Before ranking that program high enough for a potential swap or SOAP implication, the PD calls someone they trust:
- A subspecialist who moonlights there
- A former colleague who left to become APD at the new site
- Or the university’s own GME office, who quietly knows how real that “affiliation” is
Those calls decide whether the new program is treated as “legit but young” or “avoid if possible.”
And you, as an applicant, will never see that label written anywhere.
The Real Questions PDs Ask in Backchannel Calls
These aren’t polite, scripted conversations. When PDs call each other about a new program, they ask the stuff no marketing team would ever approve.
They want three things: stability, seriousness, and integrity.
1. “Is this program actually stable?”
Translation: Will it still exist, unchanged, in 3–4 years?
The biggest fear with new programs is collapse or major restructuring. I’ve seen PDs ask:
- Who controls the money? The hospital CEO, or the department?
- How committed is the C-suite? Is this just a branding project or a real investment?
- Have they had leadership turnover already, pre- or early-accreditation?
Here’s the kind of thing you hear on these calls:
“Look, they burned through two PDs before they even interviewed their first class. That’s not leadership ‘transition.’ That’s a red flag.”
Or:
“The hospital is trying to fix a staffing crisis by creating residents. They don’t understand education; they just want cheap labor.”
If the answer to “stable?” starts coming out shaky, that program quietly drops on rank lists across the region.
2. “Who’s actually teaching, and do they give a damn?”
Paper faculty lists are fiction. They’re bloated to satisfy ACGME requirements and look impressive on a website. PDs know this. So they call someone who has actually worked there:
- “Are the hospitalists any good as teachers?”
- “Do the surgeons actually let residents do cases or is it all PA-run?”
- “Are the intensivists in-house or remote tele-ICU people phoning it in?”
There’s one question that comes up a lot:
“If your own kid went into this specialty, would you be okay with them training there?”
If the person hesitates, or says “Maybe in a pinch,” that’s all the answer they need.
3. “What’s the culture? Be honest.”
Culture kills or saves a new program. And you can’t read culture from a website.
The backchannel questions:
- Is the PD respected or just a figurehead?
- Are residents treated as learners or warm bodies to plug staffing gaps?
- Do nurses and consultants take residents seriously or routinely bypass them?
- Is it malignant-lite or truly supportive?
I’ve heard faculty say:
“The PD is solid, but the hospitalists are burned out and hostile. Residents get chewed up on nights.”
Or the opposite:
“Leadership’s green, but the hospital culture is surprisingly good. Nurses love teaching. Attendings are protective of residents. I’d take that over a chaotic ‘big name’ any day.”
That nuance never shows up in official program descriptions. But it absolutely shows up in how PDs rank you relative to other programs.
The Unspoken Rating Scale PDs Use
Most established PDs carry around a mental 4-tier system when they talk about new programs. They don’t say it out loud, but I’ve watched it play out in GME conversations for years.
| Tier | How It’s Described Behind the Scenes | How It Affects Ranking |
|---|---|---|
| 1 | Solid new program, real vision | Will rank normally |
| 2 | Decent but unproven | Rank, but not top |
| 3 | Risky, structural problems | Avoid if possible |
| 4 | Do not send residents here | Essentially blacklisted |
Tier 1: “Solid new program”
These have a PD people know and trust. Real faculty. Real educational structure. The backchannel comments sound like:
“They’re new but serious. The PD came from a well-run program, the hospital is stable, they fought for protected time. I’d be okay matching someone there.”
Tier 2: “Decent but unproven”
Usually smaller community sites that may not be academic superstars but aren’t dangerous. Typical comments:
“They’ll be fine. Not amazing, not toxic. Good for a certain type of resident who wants community practice.”
These programs get ranked, just not ahead of well-known stable programs.
Tier 3: “Risky”
This is where the real damage happens. Red flags include:
- Leadership churn before first graduating class
- Rumors of hospital financial trouble
- Stories of chronic understaffing, unsafe overnight coverage
- Faculty resistance to having residents
PDs will say things like:
“I’d rather our applicant scramble than end up there.”
Tier 4: “Blacklisted”
Nobody will ever tell you this exists, but it does. These are the “over my dead body” programs.
Reasons:
- Serious patient safety concerns
- Documented abuse or malignant culture
- Administrators pressuring faculty to “work residents harder”
- PDs being forced to graduate unsafe residents
I’ve watched rank meetings where a program’s name comes up and an attending says one sentence—“We do not send anyone there”—and the discussion ends. Backchannel intel made that decision months earlier.
The Triggers That Make PDs Pick Up the Phone
Program directors are busy. They don’t cold-call every time a new curriculum appears. What makes them start working the phones about a new residency program?
Three big triggers.
Trigger 1: Aggressive expansion
When a hospital suddenly announces 5 new residency programs in 2 years, everyone in GME smells the same thing: administration- and revenue-driven expansion.
That doesn’t automatically mean it’s bad. But experienced PDs get nervous.
They ask:
- Did they build up case volume and faculty first, or are they retrofitting education onto existing service lines?
- Are chief residents or junior attendings being thrown into “core faculty” roles they’re not ready for?
- Is the DIO being pressured to push accreditation through at all costs?
The more frenzied the expansion, the more backchannel skepticism.
Trigger 2: Name-brand affiliation gymnastics
You’ve seen the websites: “Affiliated with the University of ___ School of Medicine.”
Sometimes that means real integration. Sometimes it means a single loose rotation and permission to use the logo in small print.
Other PDs know which is which. They call the academic institution and ask bluntly:
“Is this actually one of your core sites or just a contractual affiliate where you send a couple students?”
If the answer is: “They’re technically affiliated, but we don’t control anything there,” that changes how that new program is perceived across the specialty.
Trigger 3: Early resident complaints leaking out
Even in the first year, word gets around. Quietly. Usually not on Reddit first.
Common sources:
- A fellow who covers that hospital and hears interns venting at 2 a.m.
- A faculty member who still has friends at their old academic center
- Residents rotating there who go back and debrief honestly with their home PD
Once you start hearing:
“They’re violating duty hours regularly.”
“No one supervises nights.”
“The PD is great but admin shut down every change they tried to make.”
…that program starts dropping on rank lists, fast.
How These Calls Change Your Fate as an Applicant
Here’s the part you actually care about: How does this backchannel gossip affect you?
Directly. More than you think.

| Category | Value |
|---|---|
| Backchannel Reputation | 40 |
| Official ACGME/ADS Data | 30 |
| Website & Recruitment | 10 |
| Geography/Institutional Politics | 20 |
When PDs are deciding how to advise their own students and how to build rank lists for their program (especially for swaps, couples, and SOAP), the unofficial weighting looks a lot like that.
Concrete examples of what happens after those calls:
- An internal medicine PD tells their borderline applicant: “You can rank that new community IM program, but don’t put it above any established university or VA programs. They’re still sorting themselves out.”
- A surgery PD quietly removes a brand-new surg program from any scenario where their home applicants might end up swapping into it.
- An FM PD hears glowing backchannel feedback about a new rural program with phenomenal hands-on training, and suddenly they’re actively recommending it to certain residents who want broad-scope practice.
You think you’re just filling out a rank list based on interview day. But your own PD’s comfort level with those new programs—shaped almost entirely by backchannel intel—changes how they coach you, how hard they advocate if there’s post-interview communication, and how they react if you say you’re ranking a “Tier 3” place first.
What PDs Are Trying to Protect (That You Don’t See Yet)
A lot of this sounds like gossip. It isn’t. It’s risk management.
Program directors are protecting three things when they make these calls.

Protecting their residents
If there’s any chance of a transfer, shared rotations, or joint call coverage, PDs want to know: Will my residents suffer if they interact with this new program?
A malignant or disorganized new program can poison a shared ICU, ED, or subspecialty service. The PDs who’ve been burned before work harder to screen this out.
Protecting their graduates
When your PD ranks another program highly (for a swap, prelim-to-categorical path, or off-cycle placement), their name is tied to that program’s outcome.
If they send you to a dumpster fire of a new residency, and you’re miserable, burned out, or poorly trained, guess who feels responsible? The PD who said, “Yeah, that place is fine.”
After a couple of bad outcomes like that, PDs become very conservative about new programs with shaky backchannel reputations.
Protecting their brand
People don’t say it out loud, but institutional prestige paranoia is real.
If an established academic program is seen as “feeding” residents into a chaotic or low-quality new program, it reflects badly on them. Chairs notice. Deans notice. Applicants talk.
So PDs ask the hard backchannel questions before they put their institutional name anywhere near a new program’s orbit.
How You Can Read the Backchannel Without a Phone
You don’t have a PD’s contact list. You’re not going to call every DIO or chief. But you can infer a surprising amount from patterns, if you know what to look for.

| Step | Description |
|---|---|
| Step 1 | New Residency Program |
| Step 2 | Experienced PD from known program |
| Step 3 | Multiple PD or APD changes |
| Step 4 | High Risk |
| Step 5 | Positive Backchannel Likely |
| Step 6 | Mixed Backchannel |
| Step 7 | Safer to Rank Higher |
| Step 8 | Rank with Caution |
| Step 9 | Consider Avoiding |
| Step 10 | Stable Leadership |
| Step 11 | Faculty Depth |
Here’s what actually correlates with good or bad backchannel chatter:
Leadership CVs tell a story.
If the PD and APDs came from well-run programs with a reputation for fairness and strong education, that’s a big plus. If leadership is made up of people whose main qualification is “been here the longest,” that’s weaker.How many residents did they take in Year 1 and 2?
Too big too fast is a red flag. Slow, deliberate growth—3–6 per class at first—is more reassuring.Listen closely to how your own PD talks about them.
If your PD says: “They’re new, but I’ve heard good things,” that’s not filler. Someone they trust gave them that green light.
If they say: “They’re new; hard to know much yet,” with a flat voice and a quick subject change, that’s code for: “I’ve heard things but I’m not going to say them out loud.”Watch where strong applicants rank them.
When top-of-class people deliberately choose a new program and seem genuinely happy and well-trained a year or two later, that’s invaluable information. That only happens when the backchannel is positive.Look at how quickly they fill.
If a brand-new program in a solid location isn’t filling its spots, especially after 2–3 cycles, there’s a reason. That usually reflects quiet PD-to-PD warnings, not just bad marketing.

| Category | High-Trust New Program | Low-Trust New Program |
|---|---|---|
| Year 1 | 80 | 40 |
| Year 2 | 100 | 60 |
| Year 3 | 100 | 65 |
The Ugly Side: Politics and Grudges
I’d love to tell you that every backchannel call is objective and fair. It isn’t.
Sometimes you get:
- A threatened nearby program trash-talking a new competitor
- A department chair with an ego issue downplaying a new PD they used to supervise
- Long-standing academic snobbery: “If it’s not university-based, it’s garbage” (which is simply wrong in many fields)
I’ve heard older faculty say asinine things like:
“It’s a community hospital… how good could the training really be?”
Meanwhile their own residents are fighting for autonomy because there are 5 fellows on every service.
So you have to hold two truths in your head at once:
- Backchannel calls capture real, critical safety and quality concerns that won’t show up anywhere else.
- They’re also contaminated by politics, turf wars, and old prejudices.
Your job is to look for patterns, not one-off opinions.
If You’re a Student Considering a New Program
Here’s how to use all of this without access to the calls themselves.
Talk to your own PD or trusted faculty and ask targeted questions:
- “Have you heard anything about the new ___ program at ___ hospital?”
- “If one of your own kids were going into this specialty, would you be comfortable with them training there?”
- “Do you know anyone on faculty there? What do they say off the record?”
Listen not just to the words, but the temperature behind them. PDs won’t slander on email, but in a closed-door meeting they’ll tell you much closer to the truth.
Then combine that with what you can see:
- Is leadership stable, experienced, and protected with real FTE?
- Do rotations look like they give you real responsibility, not just scut and coverage?
- Are early residents (if any) burned out and evasive, or tired but proud and specific about what they’re learning?
If your gut says “this feels slapped together,” and your PD’s face tightens when you mention the program, trust that combination.
If your gut says “these people are new but serious,” and your PD says, “I’ve heard good things about the PD; they’re trying to build something real,” that’s a different scenario.
Three things to walk away with:
- Backchannel calls between PDs shape how new residency programs are trusted, ranked, and recommended long before you ever submit a list.
- Those calls focus on stability, leadership quality, and culture—things you can infer from patterns in leadership CVs, growth rate, and how your own mentors talk about the place.
- A new program with strong leadership and good backchannel reputation can be an excellent choice; a shiny new program with ugly whispers behind the scenes can quietly become a place PDs refuse to send their residents—no matter how nice the website looks.















