If you treat locums like a throwaway gig, you’re leaving permanent job offers on the table.
You are doing short-term assignments, but you want long‑term leverage. This is where most physicians blow it. They either act like a temp worker who’s “just here for a few weeks,” or they wait passively, hoping someone will magically say, “Would you like to stay forever?” That’s not how it works in the real world.
You want to turn locums work into strong permanent offers? You have to manage three things very deliberately:
- How you perform clinically and politically while you’re on site.
- How and when you signal interest in staying.
- How you use the locums rate to anchor a smart permanent negotiation.
Let’s walk through what to do, step by step, if you’re a resident/fellow or early‑career attending using locums as a bridge to a permanent job.
1. Before You Start Locums: Set Up Leverage On Purpose
If you’re already in a locums assignment, skip to the next section. If you’re planning to start locums and want it to lead to a permanent role, set it up right from the beginning.
You need to be clear on one thing: are you open to converting to permanent, or absolutely not? If it’s “maybe,” treat it as “yes” for planning purposes. It costs you nothing to create options.
Tell your recruiter or agency plainly:
- “I’m open to staying permanent if the fit and numbers are right. I’d like assignments where there’s at least a theoretical chance of conversion.”
That single sentence changes what they pitch you. Now you’re more likely to see places that are truly understaffed and might be willing to buy you out of the locums contract and lock you in.
Also, be clear about your floor for a permanent job before you start:
- Minimum base salary you’d accept.
- Rough schedule limits (nights/weekends, call expectations).
- Deal‑breakers (non‑compete radius, tail coverage, strict RVU-only comp, etc.).
You don’t need a perfectly formed number, but you do need a gut sense. Otherwise you’ll be negotiating from fatigue and flattery instead of strategy.
2. On Assignment: Behave Like You’re Already Permanent
You convert to permanent by making yourself painful to lose.
Not by asking repeatedly, “Are you hiring?” Not by sucking up to the CMO. By making the day‑to‑day lives of the people who matter noticeably easier.
Here’s what that looks like in real life:
- Show up early your first week, consistently on time afterward.
- Learn their EMR shortcuts, order sets, local protocols fast. Ask the nurses how people actually do things there.
- Do not complain about the schedule in public. Handle the work, ask for adjustments quietly through the right channel.
You’re trying to flip the narrative from “temporary coverage” to “we’d be worse without them.”
Build the right relationships (and ignore the wrong ones)
Your “conversion coalition” in most hospitals or groups:
- Department chair or medical director
- Nursing/clinic manager who runs the floor or clinic
- A couple of well‑liked senior physicians
- Scheduler and/or practice manager
- If small group: the owner/partner with real authority
Treat them like your core audience. Ask them questions that signal longevity without promising anything:
- “If someone stayed here long term, what do they usually like about this place?”
- “Is the volume now what you’d call ‘normal’ or is this a temporary surge?”
- “What’s the long‑term plan for this department? Growing? Holding steady?”
These are not idle questions. They plant the idea that you’re evaluating them for a real job, not just passing through.

| Category | Value |
|---|---|
| Dept Chair/Director | 95 |
| Nurse or Clinic Manager | 85 |
| Senior Influential Physicians | 80 |
| Practice Manager/Scheduler | 75 |
| Recruiter/Agency Rep | 60 |
Quietly document your value
You want receipts. Anecdotes and numbers you can use later when you’re talking about conversion.
Start a simple running note on your phone or a private document:
- Average daily patient volume you’re handling vs others (if you can tell).
- Any days you stayed late to help.
- Situations where you covered extra shifts at the last minute.
- Examples of compliments from nurses, staff, or patients.
- Leadership tasks you took on (protocol tweaks, teaching, case reviews).
You’re not creating a brag sheet for Instagram. You’re creating ammunition for: “Here’s what I’ve already shown I can do here” when you start talking permanent.
3. When (And How) To Signal You’re Open To Staying
The most common mistake: saying nothing until the last week, then blurting out, “Uh, so, are you guys hiring?” That smells desperate and gives all the power to them.
Do it in stages.
Stage 1: Early “fit” conversation (week 2–3)
Once you’ve settled into the workflow, request a short meeting with the department chair or medical director. Ten to fifteen minutes, not a formal summit.
Say something like:
“I appreciate you bringing me in for coverage. I like the team and the patient mix so far. I want to do this well for you, so if there’s anything you want me focusing on or avoiding culturally, please tell me now.”
You’re doing two things here:
- Showing you care about fit, not just clocking hours.
- Opening the door for them to give you feedback early (so it doesn’t quietly kill your chances later).
Stage 2: Soft interest flag (middle of assignment)
If you still like the place after a few weeks:
“I’m enjoying working here more than I expected. Long term I’m looking for a permanent position somewhere that feels like a good fit. I have a few irons in the fire, but I wanted you to know this is on my radar. If you see any potential long‑term need here, I’d be open to a future conversation.”
That’s it. Don’t ask for a job yet. Don’t talk money. Just put a pin in their mind: this person could be a solution to our staffing problem.
If they say, “We’re actually trying to recruit someone permanent,” you respond:
“Good to know. If you think my performance lines up with what you’re looking for, I’d be happy to talk specifics at the right time.”
Now they know you’re open. And you look selective, not needy.
Stage 3: Direct conversion talk (4–8 weeks before end date)
If you want to convert and it still hasn’t been addressed, you need a more explicit conversation. Email or message the chair/director:
“I’m about X weeks out from the end of my current locums contract here, and I need to firm up my plans. I’ve really liked the team and practice, and I’d like to explore whether a permanent role could make sense for both sides. Can we set up 20–30 minutes to talk about that?”
This forces clarity. They’ll either:
- Say yes, and you’re into the real discussion
- Punt with “we’re not in a position to…” which tells you not to count on them
- Or ignore you (also information: huge red flag about how they value physicians)

| Period | Event |
|---|---|
| Early Assignment - Week 1-2 | Settle in, observe culture |
| Early Assignment - Week 2-3 | Early fit check with director |
| Mid Assignment - Week 4-6 | Soft interest flag |
| Late Assignment - Week 8-12 | Direct conversion conversation |
| Late Assignment - Final 2 weeks | Negotiate details or close the loop |
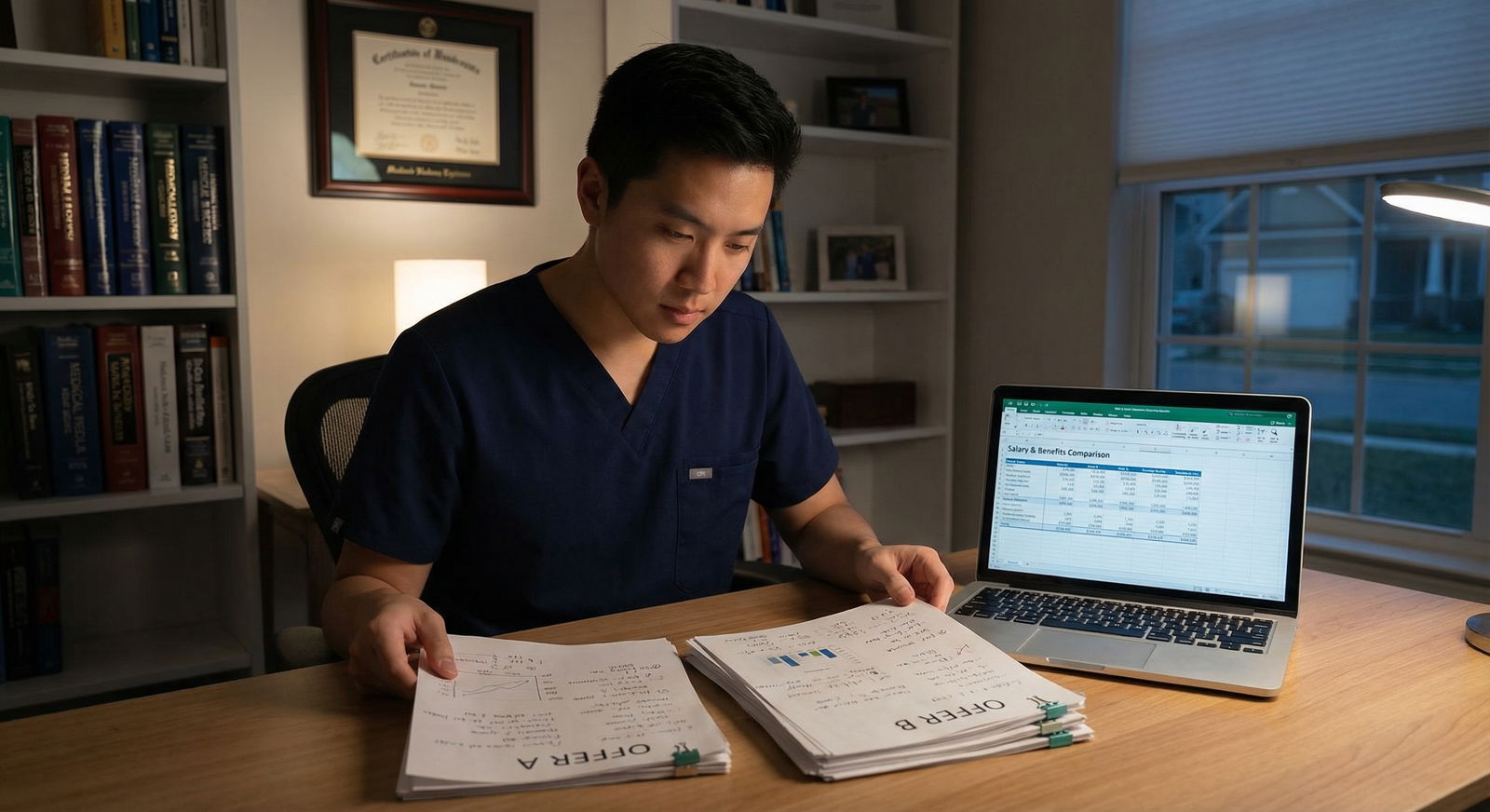
4. Using Your Locums Rate as a Negotiation Weapon (Without Being Naive)
You’re probably making a higher hourly rate as a locums doc than you’d get in a traditional salaried job. You cannot just multiply your hourly rate by 2,000 hours and demand that number as base salary. They’ll laugh you out of the room.
But your locums rate is still incredibly useful. It anchors the conversation.
Here’s the basic reality:
- Locums rate = hazard pay for flexibility, instability, and sometimes misery
- Base salary = lower per-hour, but you’re trading for benefits, stability, bonus structure, PTO, retirement match, etc.
You need to understand what your current locums income really is.
Take one typical month at that site:
- Total hours worked (include call if paid, and estimate unpaid call burden)
- Total locums income (hourly/shifts + any call/OT)
- Subtract travel/lodging differences if those change with permanent employment
Then annualize it roughly:
Annualized locums income ≈ (monthly net income) × 12
Now compare that to reasonable permanent offers in your specialty and region.
| Item | Locums Assignment | Hypothetical Permanent Job |
|---|---|---|
| Effective annual pay | $420,000 | $340,000 base + bonus |
| Health insurance | You pay full | Employer subsidized |
| Retirement match | None | 4–6% match |
| Malpractice/tail | Covered by agency | Claims‑made, tail negotiable |
| Schedule control | Some (you can leave) | Less, but more stable |
How to bring this into the conversation
When they ask about your expectations:
“Right now as locums, my effective annualized income here is around $X, but that comes with zero benefits, no retirement match, and I’m absorbing the instability. For a permanent role that includes benefits, retirement, and some predictability, I’d expect a total compensation package in the neighborhood of $Y, with a base of roughly $Z and realistic bonus structure.”
You’re not saying, “Pay me my locums rate as salary.” You’re saying, “Here’s what I’m walking away from, so the permanent package has to be in the same ballpark of total value.”
If they try the classic line: “Well, we can’t match locums rates,” you respond:
“I understand. I’m not asking you to. I am asking that the permanent offer reasonably acknowledge what I’m already producing here and what I’m currently earning to provide that coverage.”
You anchor, but you stay rational. That’s how you get real numbers, not insulting lowballs.

| Category | Value |
|---|---|
| Locums Effective | 420 |
| Permanent Base | 340 |
| Permanent Total with Bonus/Benefits | 380 |
5. The Actual Conversion Negotiation: What To Push On
Once they say, “We’d like to discuss a permanent role,” you’re now wearing three hats:
- The person they already know and (hopefully) like
- The professional who knows their true staffing pain
- The businessperson negotiating a contract
The biggest mistake here is acting like you’re still “just the locums doc.” You’re not. You’re an inside candidate with leverage.
Use insider information without being obnoxious
You know:
- Actual patient volume, not what the job posting claimed
- How often people get stuck late
- Who burns out and why
- The real call burden
- How administration treats physicians in conflict
If the contract terms don’t match reality, say that.
For example, the contract says 14 shifts/month but you’ve seen them regularly schedule 16+:
“The contract lists 14 shifts per month as standard. During my time here, I’ve consistently worked closer to 16–17 because of coverage gaps. If 16 is the real expectation, let’s make the contract and compensation match the actual practice. Otherwise we need protections around added shifts and pay differentials.”
This is where most applicants from the outside guess. You don’t have to guess. You can call out mismatches calmly.
What to prioritize in converting from locums
If you’re early‑career, I’d rank negotiation priorities like this:
- Schedule/scope sanity (how many hours, how much call, what you’re actually responsible for)
- Compensation floor and structure
- Malpractice and tail coverage
- Non‑compete and restrictive covenants
- Pathways for growth (leadership, partnership, academic time)
You already know if the schedule works because you’ve lived it. Use that. Push hardest where you know they’re understating the burden.
Malpractice and tail
Do not assume that because the locums agency covers your malpractice, the permanent job will be as simple. Ask flat out:
- “Is this occurrence or claims‑made?”
- “Who pays for tail if I leave?”
- “Does the tail obligation change based on years of service?”
If they want you badly enough, you can negotiate tail coverage as part of signing or retention. Especially if they’re rural or have been desperate for coverage.
Non‑compete
You already know the local market now. Don’t blindly accept a 50‑mile non‑compete if that would effectively exile you from your home region.
Push for:
- Narrow radius (5–15 miles depending on density)
- Narrow scope (your specialty, not “all clinical practice”)
- Clear carveouts for academic, telemedicine, or government work if applicable

6. Handling Politics: Colleagues, Permanent Staff, and the “Threat” Narrative
There is a quiet tension when a locums doc becomes “the favored candidate.” Some existing staff will be thrilled. Some will see you as a threat to their bargaining power or seniority.
You cannot fix everyone’s feelings, but you can manage yours.
A few practical rules:
- Don’t brag about the offer process or numbers to colleagues. Ever.
- Don’t side with administration against your future peers in front of them.
- Ask senior folks privately: “If I did stay, what do you think I’d need to know to make this sustainable long term here?”
You want at least one or two respected physicians in your corner saying, “We should keep them.” That matters more than you think when your offer hits the exec table.
At the same time, you’re allowed to be honest with yourself: if the politics feel toxic as a locums doc, they’ll be worse as a permanent hire. Don’t underestimate that.
7. When To Walk Away (Even If They “Really Want You”)
Sometimes a site is wonderful clinically and awful on paper. Or you get a lowball offer framed as, “But we really love you here.”
Here are clear walk‑away signals:
- The permanent offer would cut your annual income by 25–30% or more compared to realistic alternatives, with no offsetting lifestyle gain.
- Non‑compete is broad and they “never” negotiate it.
- They delay or dodge basic questions about schedule, call, or RVU expectations.
- Everything is verbal; they resist putting critical items in writing.
- You’ve already seen them treat other physicians badly (sudden schedule changes, public shaming, retaliation for speaking up).
I’ve seen docs ignore those signs because the team “feels like family.” Six months later, they’re trying to get out of a bad contract and back into locums.
Remember: you already have proof you can earn and function as a locums doc. You’re not stuck. If they can’t match basic market standards, you say a polite no and keep your flexibility.
When you decline, keep it short and professional:
“I appreciate the offer and my time here. After reviewing the terms and comparing them to my other options and priorities, I’ve decided not to pursue a permanent role at this time. I’d be open to future locums coverage if needed, but I can’t accept the current permanent structure.”
You preserve the relationship, keep the door open for high‑rate locums, and move on.

8. Turning Multiple Locums Sites into a Bidding War
If you’ve worked locums at more than one place and more than one is interested in you permanently, you’re in a rare and powerful position.
You don’t have to orchestrate a dramatic auction. Just be honest and strategic:
- Tell each site, “I am in active discussions with another group as well, and I expect to make a decision by [date].”
- When you get one offer in writing, you can tell the other: “I have another offer at $X with [key features]. If you’re serious about bringing me on, I’d need your proposal to be competitive in that range, especially regarding [schedule / RVUs / non‑compete].”
You’re not threatening. You’re letting market forces work for you. And because they’ve seen you in action, you’re not just words on a CV—they know what they’ll get.

FAQ (Exactly 4 Questions)
1. When is the best time during a locums assignment to bring up the possibility of a permanent job?
Around the midpoint of your assignment is ideal for a soft interest signal—once you understand the workflow and they’ve seen enough of your performance to have an opinion. Then, 4–8 weeks before your contract end date, you should ask explicitly for a meeting to discuss a potential permanent role. Too early and you look overeager without context; too late and they won’t have time to run the internal approval process.
2. Can I ask for the same income as my locums rate if I convert to permanent?
No, and if you insist on that, you’ll look naive. Locums rates include a premium for flexibility, uncertainty, and lack of benefits. You should calculate your annualized locums income and use it as leverage, but you translate it into total compensation expectations (base + bonus + benefits), not a straight salary demand at the same hourly rate.
3. Should I tell my agency or recruiter that I’m discussing a permanent position with the site?
Usually yes, but not at the very beginning. Many locums contracts have conversion clauses or fees if the site hires you permanently within a certain timeframe. If you start serious talks, the facility and agency will need to deal with that. Springing it on them late can sour things. Once both you and the site are seriously exploring conversion, loop in the recruiter with a simple, “We’re starting to discuss a possible permanent role; I know there may be a conversion process on your end.”
4. If I like a site clinically but hate the contract they offer, is it reasonable to keep doing locums there instead of going permanent?
Yes. That’s actually a smart move in many cases. You can enjoy the team and patient mix while maintaining higher pay and flexibility, and you avoid trapping yourself in bad contractual terms. Just be honest: thank them for the offer, decline it professionally, and say you’re happy to continue helping in a locums capacity when available. You keep the relationship, preserve your leverage, and stay out of a contract that doesn’t respect your value.
Key points to remember:
- Treat every locums gig at a potentially desirable site as a months‑long working interview—for them and for you.
- Signal interest in stages, use your real performance and locums economics as leverage, and refuse to accept contracts that do not match the reality you’ve already seen.





















