It is July 5th. You survived hospital orientation, you just put in your first admission as a real doctor, and someone casually mentions “So when are you reapplying for the categorical spot?”
You realize you have no real plan. You just started residency. And you also basically have to apply again. Soon.
This is the trap of the preliminary year. You are simultaneously:
- Learning how not to kill patients.
- Proving yourself to attendings who do not know you.
- Building a brand‑new application for the next Match… on a brutal schedule.
Let me walk you through it, month by month. What to do. When to ask for letters. When to panic (and when not to).
Big Picture: The Prelim‑to‑Next‑Match Year at a Glance
Here is the rough shape of your year if you are planning to reapply:
- July–September: Survive, identify letter writers, quietly set up your plan.
- October–December: Lock in letters, write personal statement(s), build program list.
- January–February: Submit ERAS when it opens for your cycle, request MSPE/med school docs.
- March–April: Interview season for the new cycle (yes, while still an intern).
- May–June: Rank list, Match, and transition planning.

| Period | Event |
|---|---|
| Start of Prelim Year - Jul | Orientation, first rotations, identify mentors |
| Start of Prelim Year - Aug-Sep | Ask early letter writers, clarify goals |
| Application Build - Oct-Nov | Draft personal statement, update CV, confirm letters |
| Application Build - Dec | Finalize program list, block interview-friendly rotations |
| Application and Interviews - Jan | ERAS opens for new cycle, finalize materials |
| Application and Interviews - Feb-Mar | Submit, wait for invites, early interviews |
| Application and Interviews - Apr | Peak interviews, ongoing residency duties |
| Match Closeout - May | Final interviews, submit rank list |
| Match Closeout - Jun | Match results and plan transition to new program |
You do not have time to “figure it out later.” By the time you feel comfortable as a resident, you are already behind for the next Match.
July–August: Orientation, Reality Check, and Early Positioning
At this point you should focus on three things: reputation, clarity, and opportunity.
Week 1–2 of July: Stabilize and Get the Facts
You are disoriented, exhausted, and terrified you missed something in the EMR. That is normal. Your goals right now:
Get your status crystal clear
By the end of week 2, you should:- Confirm with GME / your PD what your current slot is:
- Prelim IM for advanced derm/rads/anesthesia?
- Prelim surgery hoping to switch into categorical surgery?
- Prelim IM trying to pivot into something entirely different?
- Ask explicitly:
- “Are there any potential PGY-2 openings here historically?”
- “What is the process if I am interested in a categorical spot at this program?”
- Confirm with GME / your PD what your current slot is:
Learn the politics of your program
On day 1, everyone tells you “we support our prelims.” Sometimes that is true. Sometimes it is fiction. Watch:- Who gets staffed with which attendings?
- Which faculty actually acknowledge prelims in conferences?
- Which seniors say: “Yeah, Dr. X actually writes great letters if you show up strong”?
Start a “Match 2.0” document
A simple running document or note with:- Your target specialty (or 2 realistic options).
- Your Step scores, red flags (gaps, failures), and strengths (research, AΩA, prior career).
- A rough plan: “Reapply to IM categorical” vs “Apply to anesthesia advanced spots + TY backups.”
You are not asking for letters yet. You are not emailing random PDs. You are watching and learning.
Late July–August: Build Credibility and Identify Letter Writers
At this point you should be reliably competent on the wards and starting to look ahead.
Week 3–6: Make Yourself “Letter‑worthy”
People write strong letters for interns who:
- Are on time and prepared.
- Communicate clearly.
- Own their patients.
- Ask for feedback and then actually change.
You do not have to be brilliant. You have to be safe, responsive, and teachable.
If you are on:
- Inpatient IM or surgery:
Perfect. This is prime territory for your first strong clinical letter. - Night float or ED early:
Still workable, but you may need a later block with a more longitudinal relationship.
Start a habit:
- End of each week, jot down:
- Attendings you worked with.
- Specific patients where you did something notable (complex discharge, good family meeting).
- Any comments like “You’re doing great for July” or “You’re one of the stronger interns.”
This becomes letter‑fodder later.
Identifying likely letter writers
By mid‑August, you want a shortlist of 3–5 attendings who:
- Saw you over multiple days or weeks.
- Observed real clinical thinking, not just note‑writing.
- Are in or adjacent to your target specialty.
For example:
Prelim IM, aiming for categorical IM:
- 2 inpatient IM attendings.
- 1 clinic attending (if available).
- Optional: a subspecialty attending (cards, pulm) impressed with your work.
Prelim transitional year, aiming for radiology:
- 1 IM or surgery inpatient attending who can speak to work ethic and clinical skills.
- 1 radiology faculty from electives (later in year).
- 1 letter from med school / research mentor, if strong and still relevant.
You are still not asking for letters yet, unless something unusual happens (e.g., a 4‑week July rotation that ends early and you absolutely crushed it).
September: First Wave of Letter Requests
At this point you should ask for your first 1–2 letters.
Why September?
- You have had 2–3 months of contact.
- Attendings remember you.
- You are early enough that they are not drowning in winter obligations.
- You need letters in place by late fall to build your ERAS profile.
How to time the ask
Ask in the last week of a rotation where:
- You have worked with the attending for at least 2 weeks.
- You have not been a complete disaster.
- There was at least one attending comment that felt positive.
Script (email or in person):
“Dr. Smith, I am a preliminary intern this year and I plan to apply for a categorical IM position in the upcoming Match. I have really valued working with you on this rotation. Would you feel comfortable writing a strong letter of recommendation for my application?”
The word “strong” forces honesty. If they hesitate, say “I understand, no worries” and move on.
What you should have ready before asking
By mid‑September, have:
- A clean, updated CV (med school, research, early residency roles).
- A very rough personal statement draft (do not stress perfection yet).
- A one‑page “summary” of:
- Target specialty.
- Where you are applying (roughly).
- Anything you want highlighted: work ethic, comeback story after Step failure, research interest.
When they say yes, reply with:
- Your CV.
- The summary.
- A reminder of specific cases you worked on together (“We admitted two DKA patients and that complex heart failure case”).
October–November: Core Application Build and Final Letter Lineup
At this point you should be actively building the scaffolding of your new ERAS application.
Letters – how many and by when
You want 3–4 letters ready by late November. Breakdown:
- 2 clinical letters from your prelim program (in your target field or general IM/surgery).
- 1 additional letter:
- Med school mentor who really knows you.
- Research PI (only if truly strong and current).
- Subspecialty attending who worked with you meaningfully.
If you are switching specialties (e.g., prelim IM → anesthesia):
- Get at least 1 strong IM letter about your clinical skills.
- Try to secure 1 letter from your new target specialty during an early elective if possible.
- Use 1 “bridge” letter from a med school mentor in the target field.
Personal statement and story – October
You do not have the luxury of writing 6 drafts over 4 months. By the end of October:
- Write a straightforward personal statement that:
- Explains your path: why you did a prelim, what you learned.
- Frames your prelim year as growth, not failure or leftovers.
- Makes a clear, specific case for the specialty you are now committing to.
Bad: “I like variety, I like people, I like procedures.”
Better: Concrete moments from this year that show you functioning as a doctor.
Have 1–2 trusted people review:
- A former med school advisor.
- A senior or chief resident who knows your situation.
Program list strategy – November
Start building a spreadsheet with:
- Program name.
- Location.
- Type (university vs community vs hybrid).
- Whether they routinely take prelims into categorical roles.
- Historical fill rates and competitiveness if you can find them.
| Program Tier | Number of Programs | Example Programs |
|---|---|---|
| Reach University | 10–15 | UCSF, Michigan, Penn |
| Mid‑range Univ/Hybrid | 25–35 | VCU, UMass, Iowa, UC Davis |
| Community/Hybrid | 20–30 | St. Luke's, Reading, Advocate |
| Safety / Rural | 10–15 | Smaller state / community IM |
Most prelims under‑apply. You are risky in the eyes of programs (they know you are basically asking them to fix what did not work the first time). Apply broadly unless you have something exceptional (275+ scores, big‑name research, or major connections).
December: Tighten Application, Plan Rotations Around Interview Season
At this point you should have:
- 3 letters uploaded or promised with specific dates.
- A nearly final personal statement.
- A solid program list.
Confirm logistics with letter writers
Early December, send a polite check‑in:
“Dear Dr. Smith,
ERAS for this upcoming Match cycle will open in January. I wanted to thank you again for agreeing to write a letter of recommendation for my categorical IM application, and to ask if you anticipate being able to upload it by mid‑January. I am happy to resend my CV or summary if helpful.”
If someone has not started and seems slow, line up a backup attending in December or January.
Protect your schedule for interviews
This is where many prelims get crushed. You are still an intern. You do not control much. But:
- Talk with your chief residents by December:
- Tell them you are reapplying.
- Ask if they can place you on:
- Lighter rotations (clinic, electives, radiology, consults) during February–April.
- Avoid back‑to‑back ICU or wards in March if possible.
If your program genuinely supports prelims, they will try. If they shrug and say no, then you know the level of “support” you actually have.
January: ERAS Opens for Your Next Match Cycle
At this point you should be assembling and uploading, not starting from scratch.
Early January (Week 1–2)
- Finalize your ERAS CV with:
- Prelim year entries (rotations, key responsibilities).
- Any new research, QI, or teaching from this year.
- Final edit of personal statement.
- Confirm all letters are either:
- Already uploaded, or
- Guaranteed within 2–3 weeks.
Week 3–4: Application close to ready
By the end of January:
- Your ERAS profile should be 90–100% complete.
- All letters at least “requested,” most already in.
- Program list checked and finalized.

| Category | Value |
|---|---|
| Letters | 80 |
| Personal Statement | 90 |
| Program List | 75 |
| CV/Experiences | 95 |
Those percentages are where I expect a well‑organized prelim to be by late January. If you are at 30–40% on multiple items, you are late.
February: Submission and First Interview Invites
Depending on the exact ERAS dates for your year, you will:
- Certify and submit your application.
- Start watching your email like a hawk.
At this point you should:
- Have your phone number and email correct across everything.
- Check spam daily.
- Respond to invites same‑day, ideally within hours.
Balancing interviews and shifts
You are still an intern. Most prelim programs do not give you big blocks of official interview time off, but some will work with you if you ask early and are not a disaster on the job.
Strategy:
- Front‑load interview–friendly rotations Feb–April if possible (clinic, electives).
- Swap calls early with co‑interns (not at the last minute).
- If you must miss a day of wards/ICU:
- Tell your senior resident and attending well in advance.
- Offer to pre‑round early, pre‑write notes, or cover extra on another day.
You cannot go “full fourth‑year medical student mode” here. You have real responsibilities. But you also cannot skip interviews. Be transparent and reasonable.
March–April: Peak Interview Season and Ongoing Relationship Management
At this point you should be:
- Actively interviewing.
- Keeping your prelim performance from cratering.
- Staying in touch with your strongest supporters.
Before each interview
- Re‑read your personal statement and ERAS.
- Check the program website, recent changes (new PD, new hospital, major expansions).
- Know your narrative cold:
- Why prelim.
- What you learned this year.
- Why you are applying again, to this specific program.
You will get asked directly:
“Why did you end up in a preliminary spot?” / “What went wrong last cycle?”
Answer clearly, briefly, and without whining. Example:
“I applied late and too narrowly as a fourth‑year, and my application did not stand out. This prelim year has been the best thing that could have happened. I have real clinical experience now, I have strong letters from attendings who have seen me take care of complex patients, and I am sure I want to train in internal medicine long term.”
Own your mistakes. Show growth. Move on.
Staying in touch with your prelim program
If you have a supportive PD or APD:
- Let them know where you are interviewing.
- Ask if they would be willing to take calls from other programs.
(Some PDs actively advocate for good prelims. When they pick up the phone and say, “This intern is excellent,” programs listen.)
May–June: Rank Lists, Match Outcome, and Transition
At this point you should be wrapping up interviews and thinking about where you actually want to land.
Rank list strategy as a prelim
You are not in a position to be picky unless you have a spectacular application this time around.
- Rank every program where you would actually go.
- Do not play games trying to “signal interest” by short‑listing unless your advisor, who knows your actual file, tells you your chances are sky‑high.
You also need backup thinking:
- If you do not match categorical:
- Can your current prelim program offer a PGY‑2 spot?
- Is there a realistic option to scramble into SOAP or off‑cycle openings?
- Are you willing to do another prelim or research year? (Not ideal, but sometimes the reality.)
After Match results
If you match:
- Coordinate with both programs:
- Exact end date of your prelim year.
- Exact start date of your new categorical/advanced program.
- Any licensing/logistics issues (some states care about continuous training, some do not).
If you do not:
- Meet with your prelim PD and a trusted mentor within a week.
- Post‑Match openings and unexpected PGY‑2 vacancies appear every year.
- Have an updated “emergency” packet ready (CV, short personal statement, letters) that you can send quickly when positions pop up on emailing lists or program websites.
When Exactly to Ask for Letters: A Simple Timeline
Let me pull it together cleanly:
By Month
- September
- Ask 1–2 attendings who know you well from July–September rotations.
- October–November
- Ask 1 additional attending (especially if you did a standout rotation).
- Line up any med school mentor / research letters.
- December–Early January
- Confirm all letters are either uploaded or will be ready within weeks.
- Add a backup clinical letter if one writer is delayed or unreliable.
By Relationship Depth
Ask for letters:
- After 2–4 weeks of working together.
- When you have had:
- Multiple patient encounters together.
- At least one episode where you demonstrably helped (good handoff, solid family meeting, etc.).
- Feedback that is clearly positive.
Do not wait until:
- May or June to ask your best attendings. Their memory of specific patients fades. Your letter becomes generic.
- The week before ERAS submission. That is how you end up with 1 letter total.

| Category | Value |
|---|---|
| Week 1 | 10 |
| Week 4 | 90 |
| Week 8 | 85 |
| Week 12 | 60 |
Think of that curve as “usefulness” for asking: too early and they barely know you; too late and they have forgotten the details that make a letter compelling.
A Few Hard Truths Prelims Need to Hear
- You do not have the same timeline as your co‑interns in categorical spots. You are on a compressed schedule. Act like it.
- You cannot let your clinical performance slide because you are distracted by applications. Weak evaluations will absolutely leak into your letters.
- Programs are taking a risk on you. Your goal this year is to de‑risk yourself: clean, consistent work; straightforward story; no drama.


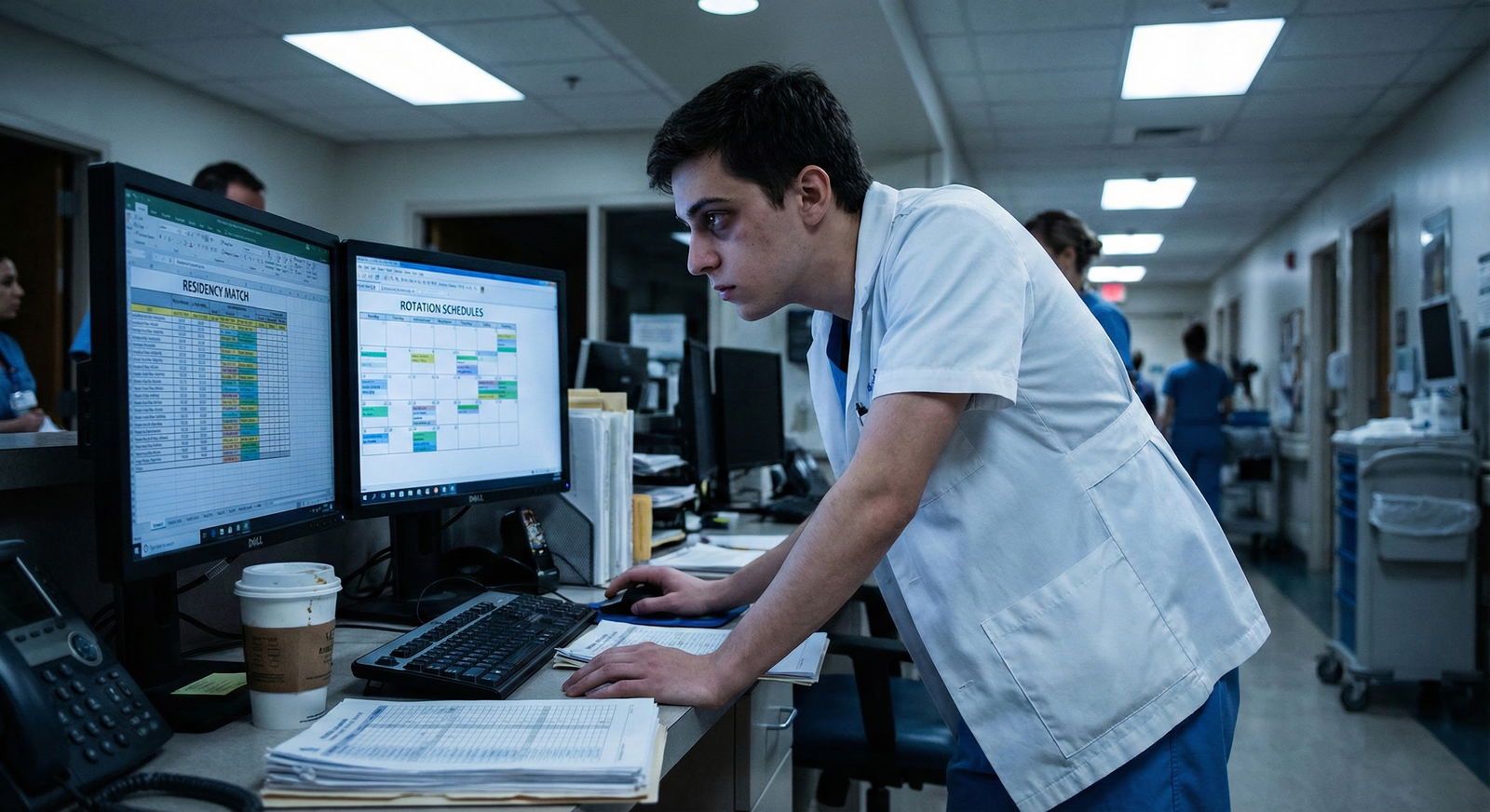
![]()
Key Takeaways
- By September, you should have impressed at least 1–2 attendings enough to ask for strong letters; by November, you should have your full letter set essentially locked.
- Treat your prelim year as an extended audition: solid clinical work, clear communication, and early, organized application prep are what convert a one‑year stopgap into a categorical spot.
- Plan the next Match like a project: structured timeline, protected interview months, broad program list, and ongoing honest feedback from mentors who actually know you and your file.




















