Most residents underestimate how brutally work hours sabotage medication safety.
Not in a vague “I am tired” way. In specific, predictable, physiologic ways that show up as wrong-drug, wrong-dose, wrong-patient errors at 03:17 when your pager will not shut up and you are on hour 25.
Let me break this down specifically. You should walk away from this knowing exactly how exhaustion translates into medication errors, what patterns to watch for on your own service, and which countermeasures actually work on the ground (not just in policy documents).
The Reality Check: Work Hours vs Error Risk
Before mechanisms, anchor this with data.

| Category | Value |
|---|---|
| 8 hrs | 1 |
| 12 hrs | 1.15 |
| 16 hrs | 1.25 |
| 24 hrs | 1.36 |
| ≥28 hrs | 1.5 |
Those multipliers are roughly consistent with several large sleep and safety studies: once you cross 16 hours, your cognitive performance is in the same ballpark as a blood alcohol concentration around 0.05–0.08. Yet you are still writing heparin, insulin, pressors, chemo pre-meds.
The important point: the risk does not increase linearly. There are thresholds.
- Under ~12 hours with decent sleep the night before: your brain compensates reasonably.
- 16–24 hours: sharp drop in vigilance, working memory, and decision speed.
- Beyond 24 and especially after a string of heavy shifts: compounding cognitive debt. You are not “a bit tired;” you are clinically impaired.
Now let us walk through how that impairment converts into medication errors you will actually see on the floor.
Mechanism 1: Sleep Deprivation and Cognitive Architecture
Sleep loss does not hit all brain functions equally. Medication safety relies heavily on three functions that get decimated when you are post‑call: attention, working memory, and executive control.
1. Attention and Vigilance
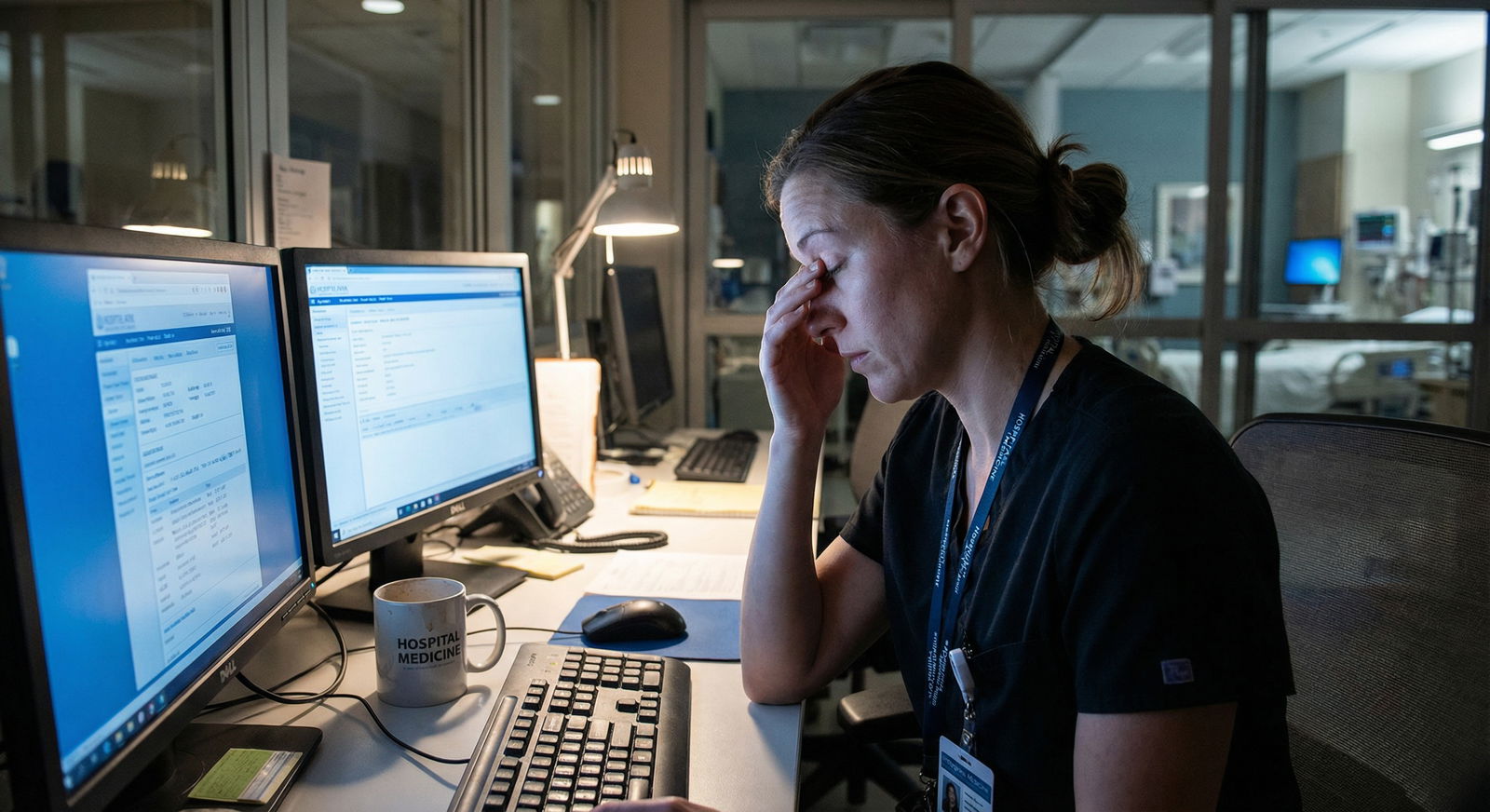
On a night shift, after 02:00, your sustained attention collapses. This is not willpower; it is circadian physiology.
What that looks like at the bedside:
- You scan the MAR and see “heparin 5,000 units subQ q8h” and your eyes just… slide past the route. You click “sign all” without noticing that the nurse is asking about an IV heparin order for DVT treatment.
- You are reconciling medications from an outside hospital. You see “metoprolol 25 mg bid.” You do not notice that someone accidentally entered it as “metoprolol IV” instead of PO.
Attention lapses create errors of omission (missing critical details) and commission (acting on misleading or incomplete cues).
This is also why look‑alike/sound‑alike drugs get you when you are tired:
- Hydralazine vs. hydroxyzine
- Clonidine vs. clonazepam
- Celexa vs. Celebrex
At 3 AM, those do not just look similar. They are identical blobs of text to your fatigued visual system.
2. Working Memory Failure
Medication ordering is a working-memory heavy task. You hold multiple data points in your head simultaneously:
- Creatinine and GFR
- Weight (actual vs ideal)
- Current vasopressors and sedation
- Last QTc
- Current antibiotic regimen and recent cultures
Sleep deprivation cuts your working-memory capacity. You can hold fewer chunks at once, and you lose them faster.
Real-world pattern: you start to enter vancomycin for a septic, obese patient with AKI.
- You think you remember their latest creatinine and weight.
- You flip to the order screen before re‑checking the labs.
- You enter something like “vancomycin 1.5 g q12h” based on your mental template from a previous patient with normal kidneys.
- You never go back to verify dosing against current creatinine clearance.
Nothing “dramatic” happens in your mind. No alarm bell. You just fail to update the mental buffer with new data.
3. Executive Function and Risk Assessment
Executive function is the part of your brain that says: “Slow down. This is high-risk. Let’s double-check.”
When you are exhausted:
- You default to heuristic thinking (“I always order X this way”).
- You underappreciate context changes (“This is not my standard ward pneumonia; this patient is post‑CABG with a tenuous graft.”).
- You get tunnel vision and miss alternatives.
This shows up in:
- Keeping a home medication like SGLT2 inhibitor on board in a patient who is now hypotensive and NPO.
- Continuing dual antiplatelet therapy in a patient with a new, unaddressed GI bleed because “they had a stent, it must be important.”
You are not “stupid” post‑call. You are running on a different cognitive mode: fast, heuristic, shortcut-driven. Which is exactly the wrong mode for nuanced medication decisions.
Mechanism 2: Circadian Rhythm, Night Shifts, and Temporal Patterns of Errors
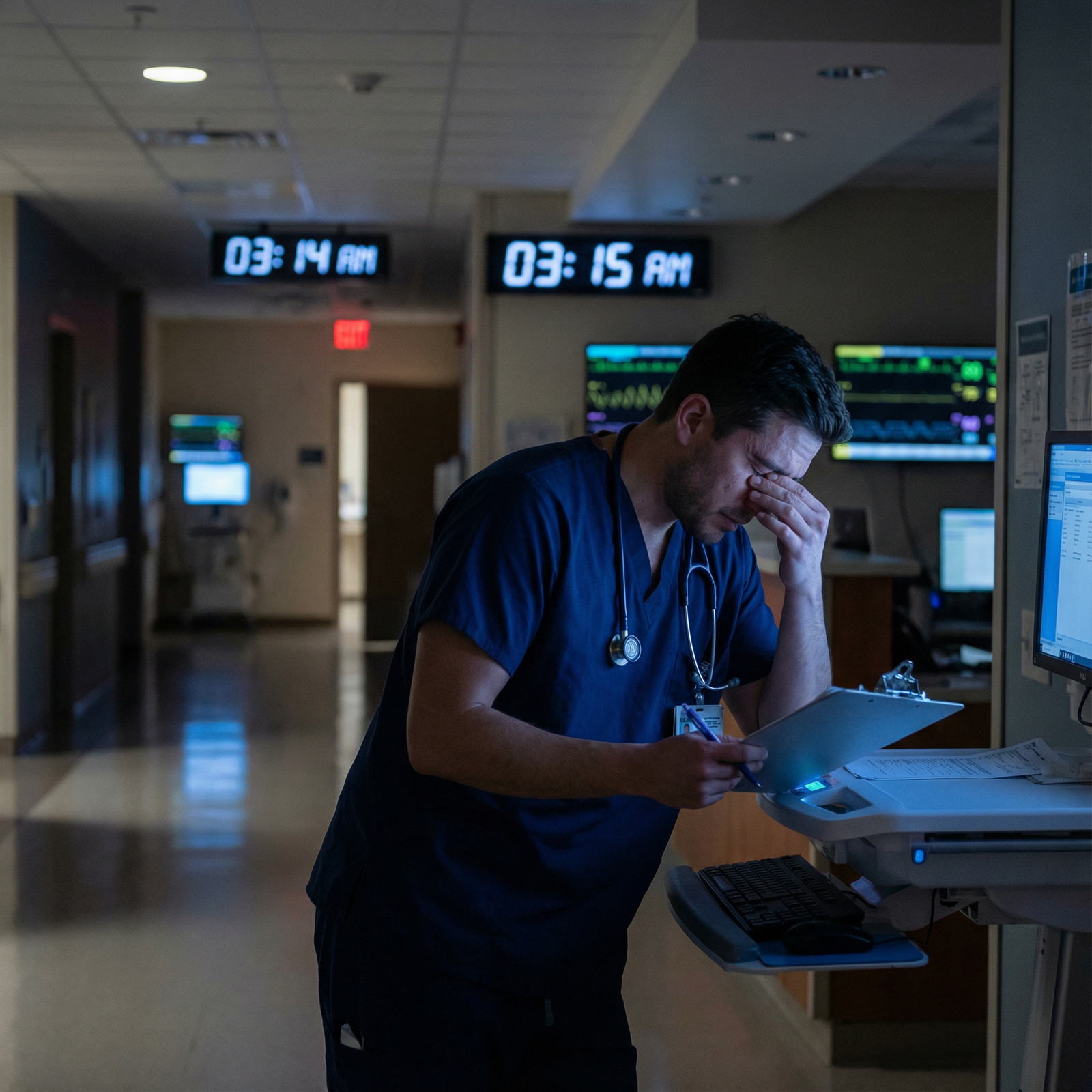
There is a very specific reason the worst medication errors cluster in the night/early morning window.

| Category | Value |
|---|---|
| 00-04 | 25 |
| 04-08 | 20 |
| 08-12 | 15 |
| 12-16 | 12 |
| 16-20 | 13 |
| 20-24 | 15 |
Most hospitals that actually audit this data see a spike between midnight and 08:00, often peaking around 02:00–04:00. Let me unpack why.
Circadian Low and Microsleeps
During your circadian low (roughly 02:00–06:00), the pressure for sleep is highest. You get:
- Slowed reaction time.
- Increased frequency of microsleeps—those 1–2 second “blank” periods you will deny having but absolutely do have on night 5 of 7.
If a nurse is calling you for a STAT insulin order at 03:30 while you are mid-note and mid-yawn:
- That 1–2 second blank can mean you do not register that the blood glucose was “48” and not “148.”
- You click through warning pop‑ups without processing them.
- You confuse the D10 bolus order with the insulin infusion order in the EHR.
These are tiny temporal gaps in consciousness. But medication ordering is a sequential, linear process. Break any link and you have an error.
Phase Shifting and Chronic Night Float
Your body never fully adapts to one week of nights.
Residents on 5–7 night runs sit in a circadian no‑man’s land:
- Not fully diurnal.
- Not fully nocturnal.
- Fragmented sleep on both ends.
I have seen residents on night 3 performing worse than on night 1. They feel more “used to it,” but in every meaningful metric (vigilance, impulsivity, error rate), they are worse. This is exactly when pattern-driven medication errors appear:
- Copy‑pasting yesterday’s complex infusion regimen with zero fresh review.
- “Renew all” on a long med list without seeing that the patient now has a creatinine of 4.5 and was started on CRRT.
Shift Handoffs at Vulnerable Hours
The handoff time itself is a risk point, especially when it happens at 06:30–07:30, still in the circadian low.
You get:
- Half‑awake overnight resident giving an imprecise verbal plan.
- Day team, still ramping up, catching only part of it.
- Medications falling off (home beta-blocker never reordered) or being duplicated (heparin infusion and prophylactic heparin injections both active).
You will see this as:
- “Why is this patient on two PPI formulations?”
- “Who renewed the warfarin after we reversed it last night?”
Often, nobody decided to do it. It happened in the cracks between two tired brains at the worst physiological time of day.
Mechanism 3: Workload, Interruptions, and the Swiss Cheese Model
Work hours alone are not the whole story. You can survive a 14‑hour day reasonably intact if the workload is sane and somewhat protected. The real disaster is long hours + high task load + constant interruptions.
Think Swiss cheese: each defense layer has holes. When enough holes align, the error passes through.
Memory Fragmentation from Interruptions
Typical scenario at 01:45:
- You start entering an amiodarone load for new‑onset afib with RVR.
- Pager: “Stat page ICU – hypotension in bed 7.”
- You stop mid‑order, run to the bedside, adjust pressors, call your fellow.
- You come back 25 minutes later and see the half-completed amiodarone order in your EHR window.
Your fatigued brain now reconstructs what you think you were planning, not what is clinically appropriate now:
- You finish the order as originally planned, not realizing the patient has since converted to sinus on their own.
- Or you complete only the infusion, forgetting the bolus. Or vice versa.
In a fresh brain, you might restart the reasoning process: “Do we still need this? Let me check rhythm and vitals again.”
In a tired brain, you just “resume task” and close the loop, because your cognitive fuel is almost gone.
Cognitive Overload and Defaulting to Templates
Another pattern: on post‑call ICU or a floor with 20+ patients, cognitive bandwidth is gone by early afternoon.
When you are overloaded, you gravitate to templates:
- The “standard sepsis bundle” antibiotic combo, regardless of local microbiology.
- The same morphine PCA settings you use for every post‑op, regardless of age, renal function, or OSA.
- Reloading a med list by clicking “reorder all previous meds” on admission, then skimming it instead of rebuilding from scratch.
Templates can be helpful—but under fatigue, you stop individualizing therapy. That is medication error by context blindness.
Alert Fatigue: The EHR That Cried Wolf
Every resident has clicked through thousands of EHR medication alerts that are clinically irrelevant.
After enough hours, this becomes pure muscle memory:
- Red box: click override.
- “This dose exceeds recommended maximum”: click justify.
- “Potential interaction with X”: click continue.
Under normal conditions, you will occasionally pause on relevant alerts.
On hour 24 of a bad call:
- The system flags a real issue (e.g., QT‑prolonging combo, critical renal function change).
- You override it with the same speed as the hundreds of fake alerts before it.
Work hours magnify alert fatigue. Long shifts and chronic overload strip away the mental energy needed to distinguish noise from signal.
Mechanism 4: Team Dynamics, Supervision, and Hierarchy under Fatigue
Medication safety is not just an individual cognitive game. It is a team sport. And long work hours distort the team.
Supervisors Are Tired Too
Attendings and senior residents who “trust you” more on nights often do that for the wrong reasons: they are exhausted and overwhelmed themselves.
You will see patterns like:
- Senior on home call half-awake at 03:00: “Yeah, that sounds fine, go ahead and order it,” without pulling up the chart.
- Attending post‑call morning: “Did pharmacy approve it?” If you say yes, they stop there and do not re‑check the renal dosing or the protocol details.
Supervision quality degrades with fatigue. The idea that you are “more independent” at night can be code for “we are all too tired to properly double-check each other.”
Hierarchy and Reluctance to Challenge
Now combine that with hierarchy:
- A tired senior says, “Just give another 4 mg IV hydromorphone.”
- The intern thinks, “This is an elderly patient with OSA on high‑flow,” but it is 02:00, the senior is drowning in pages, and the intern does not push back.
Or:
- Pharmacy pings you with a dosing question. You are stretched thin and reply, “That’s fine, just leave it,” instead of meaningfully engaging.
Pay attention to how often “because the senior/attending said so” becomes the only safety check. Under long hours, that happens more than anyone wants to admit.
Mechanism 5: Chronic Fatigue, Burnout, and Risk‑Taking Behavior
Acute fatigue is bad. Chronic sleep debt plus burnout is worse. That state fundamentally shifts your risk calculus.
You start to care less.
Not because you are a bad doctor. Because your brain is blunt from cumulative stress, emotional exhaustion, and moral injury.
This shows up subtler:
- You know technically you should reconcile each medication with indication, dose, and timing. Instead you skim because “no one dies from a missed statin.”
- You rationalize: “If pharmacy really hates this order, they will call me.” You push local responsibility to someone else.
Over months, the threshold for “good enough” drifts lower. That is how you end up with:
- Multiple days of duplicated anticoagulation.
- Unnecessary continuation of high‑risk drugs like antipsychotics or benzos started for transient delirium.
- Sloppy syringe labeling in busy codes or rapid responses.
Burnout is not just an emotional problem. It is a direct medication safety issue.
Where Residents Actually Get Burned: Common Error Patterns
Let me be specific about the kinds of medication errors that show up disproportionately on long or night shifts. If you recognize these patterns, you are halfway to preventing them.
| Pattern Type | Typical Scenario |
|---|---|
| Renal dosing errors | Aminoglycosides, vancomycin, LMWH in AKI |
| Duplicate anticoagulation | Heparin drip + prophylactic subQ heparin |
| Insulin mismanagement | Basal continued in NPO, or sliding scale only |
| Look-alike drug selection | Hydralazine vs hydroxyzine, Celexa vs Celebrex |
| Missed home critical meds | Parkinson, anti-epileptics, transplant meds |
1. Renal and Hepatic Dosing
Why it clusters with fatigue:
- Requires multiple data pulls (labs, weight, comorbidities).
- Requires updating mental models, not just copying previous orders.
- Protocol tables are annoying to look up when you are on hour 22.
You see:
- “Just do what they were getting before” despite new AKI.
- Forgetting to re‑order renally dosed meds after patient starts dialysis.
- Rounding errors in mg/kg dosing when your math brain has left the building.
2. Anticoagulation Chaos
Multiple classes, overlapping indications, procedural holds, bridging. Perfect setup for a tired brain to:
- Resume full‑dose anticoagulation too early post‑procedure.
- Hold it longer than needed “until morning team figures it out.”
- Stack prophylactic and therapeutic doses.
Most residents will eventually have a “who ordered this combination?” case. Often the honest answer is “a sleep‑deprived me, half a day ago.”
3. Insulin and Glucose Management
This is an all‑time classic:
- Patient is NPO after midnight for an early case. You are on night float.
- The nurse asks: “What about their Lantus 40 units?”
- It is 01:00, you are behind. You say: “Just give their usual dose.”
The next morning the patient is found hypoglycemic.
Or the opposite: you panic and hold all insulin, including basal, in a brittle type 1 diabetic, and they drift into DKA over 24 hours.
Insulin requires nuance. Nuance is precisely what chronic fatigue erases.
4. Look‑Alike / Sound‑Alike Selection Errors
Fatigue narrows the perceptual filter. EHR search fields are traps:
You type “meto…” and click the first thing:
- Metoprolol tartrate vs succinate.
- Methotrexate daily instead of weekly.
- Methylphenidate instead of methimazole.
These are classic sentinel events. Residents are not immune. They are more vulnerable when running on fumes.
5. Failure to Reconcile High‑Risk Home Medications
On busy admits, the med rec becomes a check‑box exercise:
- You miss that the Parkinson patient’s carbidopa/levodopa timing matters to the minute.
- You overlook transplant immunosuppression doses and schedules.
- You delay restarting anti-epileptics in a patient with a history of status.
These are not “fancy” cognitive tasks. They are tedious. Tedious tasks get sacrificed when you are sleep-deprived and drowning.
Mechanism 6: System Design That Assumes a Well‑Rested Human (Which You Are Not)
Hospital systems and EHRs are usually built as if the user is:
- Fully awake.
- Under minimal time pressure.
- Capable of reading dense text, small fonts, and subtle warnings.
You, the resident, are none of those things most of the time.
This mismatch creates friction:
- Critical orders buried three clicks deep.
- Important safety info (e.g., “dose adjusted for CrCl”) in microscopic footnotes.
- Repetitive credential prompts that train you to click through anything with a button.
Long work hours + clunky systems = more opportunity for errors to slip through all layers.
Practical Countermeasures Residents Can Actually Use
You cannot fix ACGME rules or redesign Epic this month. But you are not helpless either. The goal is to put a few low‑friction guardrails in place that work especially when you are tired.
1. Establish Non‑Negotiable “Pause” Moments
Pick a short list of orders where you force yourself to pause, regardless of fatigue:
- Any IV opioid for an opioid‑naïve patient.
- Any new anticoagulant or major dose change.
- Any insulin regimen change (not sliding scale add‑ons).
- Any chemotherapy adjunct, high‑dose steroid, or immunosuppressant.
Your rule: before you click sign, you check:
- Weight, creatinine, LFTs.
- Indication.
- Route and timing. Takes 20–40 seconds. Saves you from the majority of serious harm events.
2. Use Written or Digital Checklists, Not Memory
For night float admits or cross‑covering:
Have a short med safety checklist at the top of your note or task list:
- Restarted essential home meds?
- Reviewed anticoags with renal function and procedural plans?
- Insulin plan documented with NPO status?
- QT‑prolonging combos checked in high‑risk patients?
You will not remember to think of these on hour 24. Offload to paper or screen.
3. Leverage Nurses and Pharmacists as Active Safety Nets
If you treat pharmacy as an obstacle, you are making your life harder.
Better approach:
- Proactively tell nurses and pharmacists on heavy nights: “If any order looks off, please page me; I genuinely want the second look.”
- When pharmacy calls, listen for the meta-message: “Does this make sense?” is often their diplomatic way of saying “This might hurt someone.”
Your ego will be slightly bruised a few times. Your patients will be safer. So will your license.
4. Time‑Protect High‑Risk Tasks
Bad idea: entering all your heparin drips and insulin regimens between rapid responses and cross‑cover pages.
Better:
- Batch high‑risk med orders in brief windows when you can focus for 5–10 minutes uninterrupted.
- If you get pulled away mid‑order, abort and restart the cognitive process later rather than resuming blindly.
If this means telling a nurse, “Give me 10 minutes to finish this heparin order safely, then I’ll call you about the constipation meds,” do it.
5. Protect Your Own Sleep Ruthlessly
No, you are not weak for needing real sleep. You are unsafe without it.
Basic but often ignored:
- Dark, quiet, cool sleep environment post‑call. Phone on Do Not Disturb with emergency bypass for family only.
- Caffeine early in the shift, tapering before the last 4–6 hours so you can actually sleep later.
- Cut the heroic nonsense like, “I can function on 3 hours, I’m fine.” That is how people lose careers over preventable errors.
You cannot eliminate fatigue. You can reduce the severity and frequency of being completely cognitively bankrupt.
FAQs
1. Are shorter shifts always safer for medication errors?
Not automatically. A 12‑hour shift with 20 admits and chaos can be more dangerous than a 16‑hour shift with controlled workload and good backup. What matters for medication safety is the combination of duration, sleep quality before the shift, cognitive load, and the presence of functioning safety nets (pharmacy, nurses, senior backup, reasonable EHR design).
2. Is it reasonable to refuse to write certain high‑risk orders when I feel too tired?
You are within your professional rights to slow down and insist on help. Saying, “I want to run this by my senior/attending because I am not comfortable doing it solo at this hour” is not weakness. That is risk management. If you truly feel unsafe, escalation is appropriate. The only indefensible choice is blindly pushing through a high‑risk decision when you know you are cognitively impaired.
3. How can I tell if I am too fatigued to be safe?
Red flags: rereading the same order three times and still not processing it; forgetting what you were doing mid‑task repeatedly; almost falling asleep at the computer; irritability to the point where any question feels like an attack. If you see those, you are not “a little tired.” You are impaired. At that point, offload high‑risk decisions, use checklists aggressively, and involve your team.
4. Why do I make more mistakes on night float week 2 than week 1? Shouldn’t I adapt?
You rarely get full circadian adaptation because days off, morning conferences, and sunlight exposure pull you back toward a diurnal rhythm. Instead of adapting, you accumulate chronic partial sleep deprivation. Subjectively you feel more “used to it”; objectively your vigilance and executive function are worse. That is why errors creep up in week 2.
5. Does double‑checking every medication order solve the problem?
No. You do not have the bandwidth to scrutinize every multivitamin. The point is not paranoid perfection; it is targeted vigilance. Identify the 5–10 high‑impact medication categories and situations on your service—opioids, anticoagulants, insulin, narrow‑therapeutic‑index drugs, renal dosing changes—and build habits and micro‑systems around those. Aim for smart, prioritized safety, not blanket overchecking that you will abandon on busy nights.
Key points:
Long work hours degrade specific cognitive systems—attention, working memory, executive control—that medication safety depends on.
Medication errors under fatigue follow recognizable patterns (renal dosing, insulin, anticoagulation, look‑alike drugs) that you can anticipate and guard against.
You cannot eliminate fatigue in residency, but you can design your habits so that when you are at your worst, your system—not just your willpower—catches you before an order harms someone.



















