
The usual advice of “sleep is always more important than studying” is wrong on heavy call months. But so is the idea that you can just “grind through” and sacrifice sleep. You need a system, not vibes.
Here’s the answer: on heavy call, you prioritize functional sleep first, then targeted studying. Not the other way around. The trick is knowing (1) your minimum viable sleep, (2) what actually deserves study time, and (3) which days to push and which days to accept “maintenance mode.”
Let’s build that out.
Step 1: Set Your Non‑Negotiables (Safety Before Heroics)
Your first job isn’t to ace boards. It’s to not hurt patients or yourself.
On heavy call months (q4–q6, 24+4, nights, ICU, trauma), you need to define your absolute minimums:
- A minimum sleep floor (non-call days): usually 6 hours for most people
- A safety floor (post‑call / brutal nights): sometimes that’s 4–5 hours, then back to bed after basic life tasks
- A max weekly “studying expectation”: usually less than you think – 4–6 focused hours/week may be realistic
If you’re regularly below these floors, you’re not being “dedicated.” You’re being dangerous.
Quick self-check: are you too sleep-deprived to study?
If any of these are true, you sleep first, no debate:
- You catch yourself rereading the same line 3 times
- You forget why you entered a room more than once in a shift
- You’re getting irritable or unprofessional with nurses/families
- You feel physically dizzy or nauseated from fatigue
- You’re microsleeping (nodding off) at the computer
If that’s you, shut the laptop. Close UWorld. Sleep. You’ll get more out of 90 minutes tomorrow than 3 hours of zombie “studying” tonight.
Step 2: Decide Your Priority for This Month
Not every month is a “try to crush studying” month. Some are “just survive and avoid remediation” months.
You need to honestly label the month you’re in:
| Month Type | Primary Goal | Studying Expectation |
|---|---|---|
| Survival Month | Don’t drown / stay safe | 2–3 hrs/week |
| Maintenance Month | Stay sharp, not progress | 4–6 hrs/week |
| Push Month (lighter call) | Real progress for boards | 7–10+ hrs/week |
Heavy ICU, trauma, night float, or malignant services? That’s usually a Survival or Maintenance month.
You’re allowed to say: “This is not a board-crush month. This is an ‘I will not lose ground and I will not fall apart’ month.”
That mindset alone cuts your anxiety in half, which weirdly makes you more productive.
Step 3: Use the Call Cycle to Your Advantage
You can’t treat all days of a call cycle the same. You’ll burn out fast.
Think in 3-day or 4-day blocks depending on your call schedule.
Example: q4 call (Post‑Call, Recovery, Work, Call)
Here’s how I tell residents to think about it:

| Category | Value |
|---|---|
| Post-Call | 20 |
| Recovery | 60 |
| Work | 70 |
| Call | 40 |
- Post‑Call Day: Energy ~20%. Priority: sleep, food, essential chores. Studying: optional, 0–20 minutes max, only if you feel normal.
- Recovery Day: Energy ~60%. Priority: 1 short focused study block (20–40 minutes).
- Work Day: Energy ~70%. Priority: another short block or some “incidental” learning (podcast, quick reads).
- Call Day: Energy ~40% and variable. Priority: survival; maybe 10–15 minutes of micro‑study if calm.
You’re not trying to study every day equally. You’re front‑loading on the better days and not beating yourself up on the bad ones.
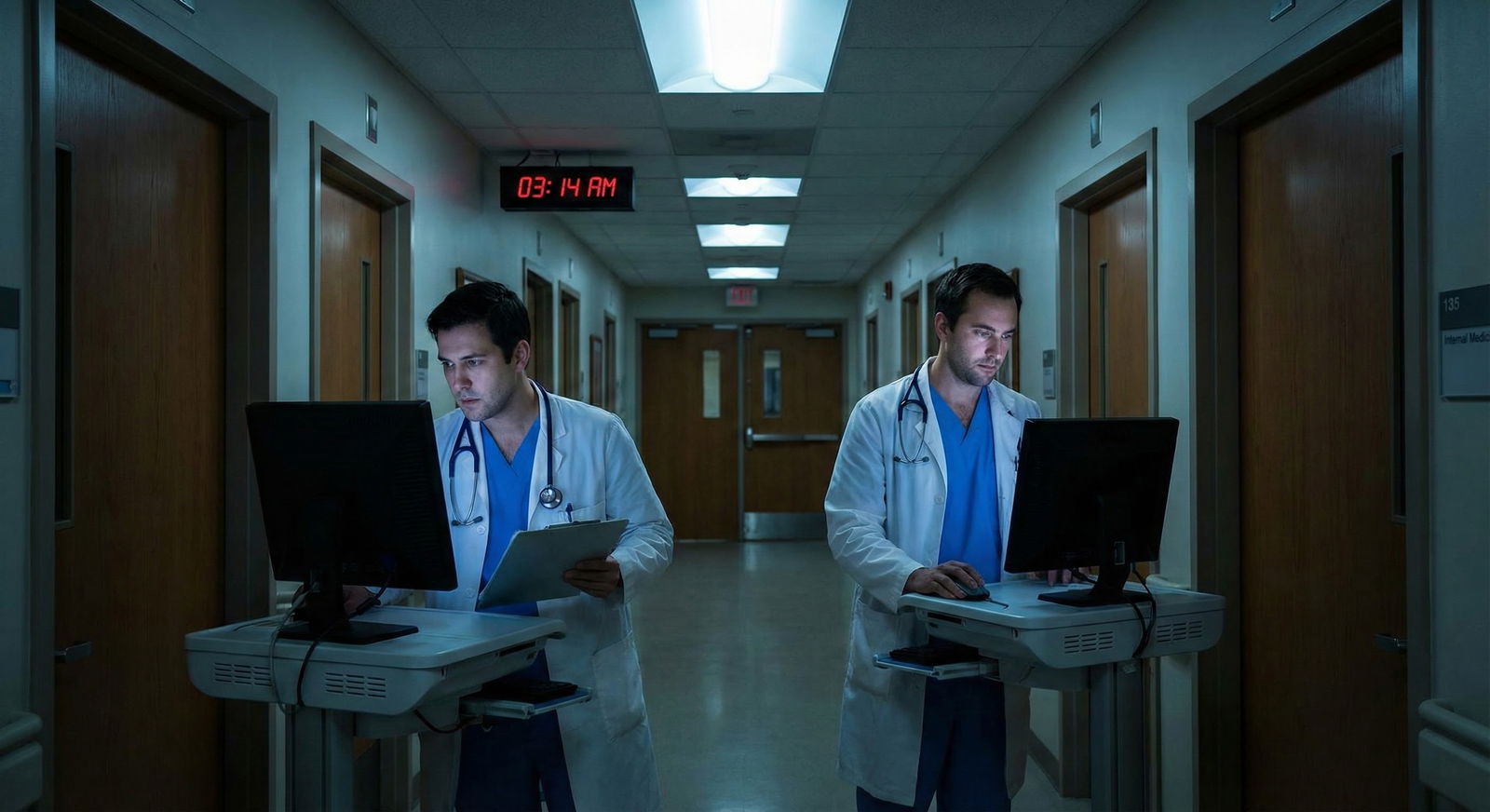
Nights: Completely different game
On nights, flip it:
- Pre‑night: Sleep anchor. You protect this like a procedure consent. If you blow this, the whole week spirals.
- Early nights (1–2): maybe small studying chunks before shift while you’re still fresher.
- Late nights (3–6+): survival mode. If you study, it’s 10–20 minutes max, usually right before bed when you get home or as micro-review during the shift.
Step 4: Shrink the Definition of “Studying”
During heavy call, your biggest mistake is holding onto your “ideal” study day. Two hours. Coffee. Highlighters. Question blocks. Calm.
That doesn’t exist this month.
You need micro‑studying and embedded learning.
Examples that actually work on call:
- One 10-question UWorld block between pages or signouts
- Reading 1 UpToDate topic on something you just admitted (hepatic encephalopathy, DKA, COPD exacerbation)
- Flashcards (Anki) on your phone while waiting for CT
- Reviewing your own “one-pager” on sepsis, AFib, chest pain before shift
Studying doesn’t have to mean “sit at a desk.” You’re surrounded by real patients with real problems. That counts.
What you should NOT do on heavy call months
- Starting a brand-new, massive Qbank
- Trying to “catch up” 200+ Anki cards/day
- Signing up for extra board-review courses
- Committing to daily 2-hour study blocks
That’s fantasy. All that does is create guilt and make you feel like you’re failing. You need small, winnable commitments.
(See also: The Unwritten Rules of Calling Your Attending at 3 AM on Call for practical tips.)
Step 5: Use a Simple Daily Triage: Sleep or Study?
Here’s the direct framework I give interns and PGY-2s:
Ask yourself three questions at the end of your shift:
- How many hours did I sleep in the last 24 hours?
- How many days in a row have I been under 6 hours?
- Do I feel closer to “wired‑tired” or “nodding-off-on-the-toilet” tired?
Then follow this:
(Related: Which Overnight Pages Can Safely Wait and Which Require You Now?)

| Step | Description |
|---|---|
| Step 1 | End of Shift |
| Step 2 | Sleep first 60 to 90 min |
| Step 3 | Do 20 to 30 min focused study |
| Step 4 | Reassess later or next day |
| Step 5 | Last 24h sleep less than 5h? |
| Step 6 | Under 6h for 3 days straight? |
| Step 7 | Nodding off or unsafe tired? |
That’s it. You don’t negotiate with yourself beyond that.
If your brain is mush → sleep.
If you’re tired but functioning → 20–30 minutes of single‑tasked studying, then bed.
Not 90 minutes. Not “until I finish this UWorld block.” You stop early on purpose to protect tomorrow.
Step 6: Choose High-Yield Content Only
On heavy call, your study material has to earn its keep. If it’s not immediately improving your patient care or directly tied to an upcoming high‑stakes exam, it’s out.
Good choices on heavy call:
- Review the top 10–15 bread-and-butter problems for your service:
- For IM: sepsis, DKA/HHS, chest pain, AFib/RVR, COPD/asthma exacer, AKI, GI bleed, encephalopathy, pneumonia
- For surgery: acute abdomen, trauma resuscitation, SBO, post-op fever, shock, GI bleed, wound issues
- For OB: preeclampsia, PP hemorrhage, shoulder dystocia basics, FHR tracings, infections
- Single UpToDate topic on something you saw that day
- UWorld/AMBOSS questions specifically filtered to your current rotation
- Review of your program’s protocols (sepsis bundle, insulin drip, anticoag reversal)
Bad choices this month:
- Random deep-dive into obscure zebras
- Rewriting huge notes or “perfect” cheat sheets
- Watching 90-minute lecture videos after 24h call
- Getting lost in PubMed at 2 a.m. trying to answer a theoretical question
Heavy call studying should feel almost directly connected to “the patients I saw today” or “the boards topic I always miss.”
Step 7: Protect 1–2 Real Recovery Days per Month
If your call schedule offers an actual golden day off (no clinic, no continuity, no mandatory teaching), protect it.
That day has one job: reset your sleep debt and stress level.
Rough structure that actually works:
- Sleep until you wake up naturally (no alarms)
- AM: no studying. Move your body, get sunlight, eat like a human.
- Early afternoon: 45–75 minutes of high‑quality, focused studying. Just once. Timer on, phone away.
- Evening: back to normal life – partner, kids, friends, laundry, whatever makes you feel like an actual person.
You don’t “make up” an entire month of call studying in one day. You just move the needle and feel less behind.
Step 8: Watch for the Red Flags You’re Ignoring Sleep Too Much
Residents are really good at normalizing disaster. You’ll tell yourself you’re “fine” when everyone around you can see you’re not.
Red flags you’re losing the sleep vs study battle:
- You’re making charting or medication errors you never used to make
- You snap at nurses or co-residents over tiny things
- You’re getting sick more often or not recovering from minor illnesses
- You sit down “to study” and scroll for 40 minutes, then feel angry at yourself
- Your partner/friends are saying you’re checked out, short, or constantly exhausted
If 2+ of those are happening, your studying goal this month is now: stabilize your life and your sleep enough to be safe. That’s it.
Concrete Weekly Plan (Sample)
Let’s put this together. Say you’re an IM PGY-1 on q4 call, heavy admissions, with one golden day off every 2 weeks.
Reasonable weekly target: 4 hours of real studying.
Here’s how it might look:
| Day Type | Study Time | Focus Area |
|---|---|---|
| Post-Call | 0–15 min max | Only if feel okay – 5 cards |
| Recovery | 30–40 min | 10–15 targeted questions |
| Work Day | 20–30 min | 1 short topic + 5–10 cards |
| Call Day | 0–15 min max | Bedside learning / quick read |
Spread across a week, this gets you close to 4 hours without sacrificing basic sleep.
The Real Answer: Stop Chasing Perfection
The most successful residents on brutal call months don’t out-tough everyone. They out‑plan everyone.
They:
- Accept that sleep is the foundation, not the leftover
- Shrink studying into small, brutal, high-yield chunks
- Use the patients in front of them as their curriculum
- Stop beating themselves up for not matching their lighter-rotation pace
You’re not a machine. Heavy call months are temporary. The goal is to exit them intact, not with the perfect UWorld percentage.
FAQ: Studying vs Sleep on Heavy Call Months
1. Should I ever stay up late to finish a UWorld block on call months?
Almost never. If you’re post‑call or pre‑call and already under 6 hours of sleep, forcing yourself to finish a block is a bad trade. You’ll do worse on the questions, retain less, and wreck tomorrow. Far better: stop at 5–10 questions, review carefully, and sleep.
2. Is it okay to basically “not study” for a whole heavy ICU or trauma month?
If it’s a truly brutal month and you’re barely keeping your head above water, yes – your only academic job is to learn from your patients and avoid getting in trouble. But “not studying” shouldn’t mean “no learning.” Use what you’re seeing: look up one key topic per shift. That alone will prevent backsliding.
3. What if I have boards or in‑training exams right after a heavy call month?
Then you need a ramp‑up plan before and after. Two to four weeks before the heavy month, increase your studying. During the heavy month, maintain with 3–4 hours/week. After the heavy month, protect a few days for sleep and then hit a 7–10 hours/week pace if possible. Don’t expect peak performance during the worst call weeks.
4. Are podcasts and videos “good enough” studying when I’m exhausted?
They’re fine as supplemental learning but terrible as your only strategy. Passively listening half-awake doesn’t stick. If you’re using podcasts, pair them with very short active steps: pause, write down 2–3 key points, or do a couple questions on that topic later in the week.
5. How do I handle guilt when I choose sleep instead of studying?
Name it for what it is: performance anxiety, not laziness. Remind yourself that chronic sleep deprivation destroys memory, judgment, and exam performance. Write it down if needed: “Sleeping 90 minutes now will help me retain tomorrow’s studying and be safer with patients.” You’re not slacking. You’re choosing long‑term performance over fake short‑term productivity.
6. What’s the minimum studying that keeps me from falling behind?
For most residents on a heavy month: about 20–40 minutes, 3–4 days per week, focused on high-yield problems you’re seeing on service. That’s it. Not pretty, not perfect, but enough to keep your brain engaged and prevent full regression while you ride out the rotation.
Key points: Sleep is your baseline, not the bonus. On heavy call, shrink studying into short, targeted sessions tied to real patients. And stop pretending this month has to look like your easy elective month; aim for “safe and steady,” not “superhuman and broken.”


















