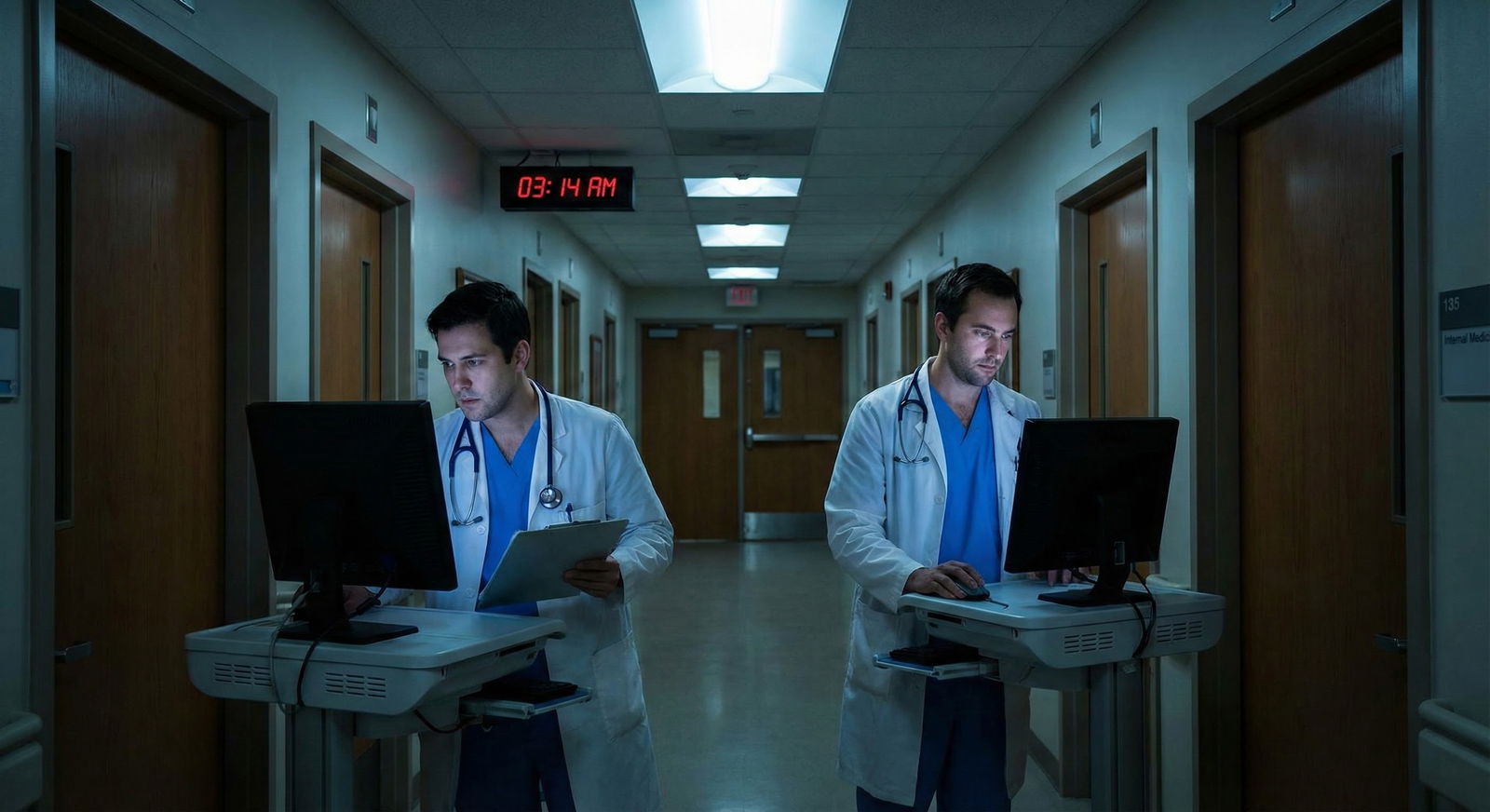
You’re on night float. It’s 2:17 a.m. The cross-cover pager goes off:
“Hey doc, this is RN on 7W. Your patient in 733, Mr. Jones, is more short of breath. Can you come take a look?”
You have never seen this person. You barely recognize the name. You’ve got three other pages blinking, and your brain is at 40% battery.
Here’s what you actually do to quickly review an unfamiliar patient overnight without missing something dangerous or wasting 30 minutes clicking in the chart.
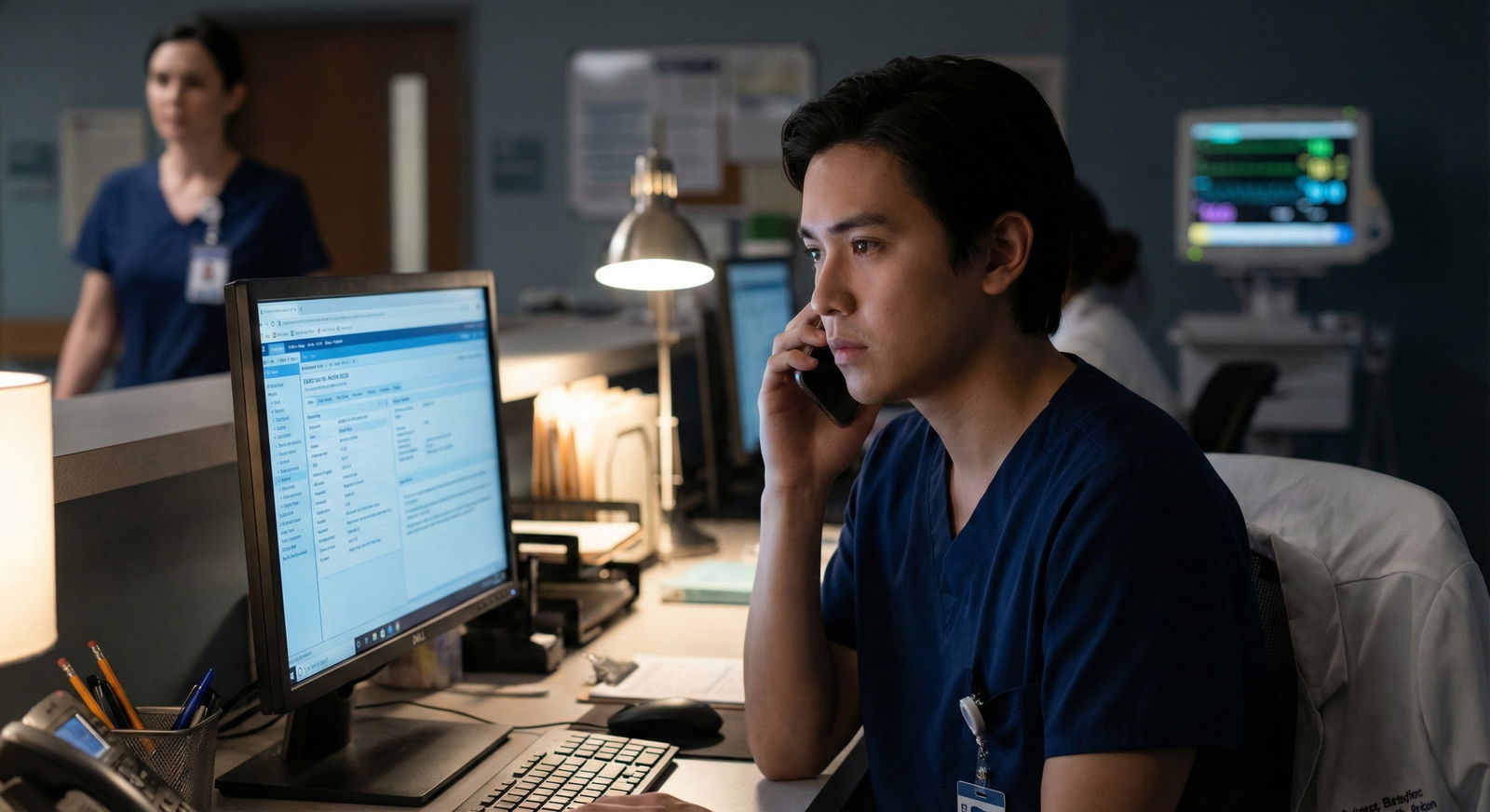
Step 1: Before You Walk In – Grab the Non-Negotiables
Do not sprint blindly to the room without any context unless the nurse clearly says, “They look awful / may code.” If this is a non-crashing situation, you get 2–3 minutes to arm yourself.
Here’s the tight pre-room checklist I use.
Open the chart; find the “why are they here” sentence.
Look at:- Admission note first line or hospital problem list
- Most recent attending or resident progress note "Assessment/Plan" top line
You’re hunting for: “Admitted for…” or “Principal problem: …”
Example: “Admitted for acute decompensated systolic heart failure.” That already tells you what’s likely to kill them tonight.Scan the problem list like a radar, not a textbook.
Take 10–15 seconds to clock:- Major chronic diseases: CAD, HF, COPD, ESRD, cirrhosis, cancer
- Any bleeding/clotting history: DVT/PE, GI bleed, stroke
- Serious psych or substance history: withdrawal risk, SI, agitation
You’re not memorizing. You’re just building a mental “risk map.”
Check current vitals and trend.
Don’t just look at the last set. Look at the trend over the last 6–12 hours:- HR
- BP
- RR
- O2 sat and mode (room air vs 2L NC vs 10L NRB)
- Temp
- Pain score if relevant

| Category | Value |
|---|---|
| Resp Rate | 10 |
| O2 Sat | 9 |
| Heart Rate | 8 |
| Blood Pressure | 7 |
| Temperature | 5 |
If RR is 30 and sats are dropping, you already know this is not a casual visit.
Look at meds like a landmine map.
Two quick questions:- Are they on anything that can tank them overnight? (opioids, benzos, insulin, IV diuretics, anticoagulation, chemo, pressors)
- Are they on something you must never miss? (anticonvulsants, Parkinson meds, steroids in adrenal patients, transplant immunosuppression)
Know their code status.
Glance at Orders → Code status.
You need this in your head before you walk in if they start to crash.
This should take under 3 minutes. If you’re at 10–15 minutes browsing, you’re doing too much for an initial check.
Step 2: Get a Tight, Purpose-Driven Handoff From the Nurse
When you call or arrive on the floor, don’t ask vague questions. Nurses are busy and it’s 2 a.m. You need focused data.
Ask something like:
- “What specifically changed that made you call?”
- “How long has this been going on?”
- “Any recent vitals trends?”
- “Oxygen changes? New oxygen or increase?”
- “Any new pain, bleeding, confusion, chest pain, shortness of breath, or decreased urine?”
If the nurse sounds very worried — “They just don’t look right” — that’s a huge red flag even if the numbers look okay. I’ve watched residents ignore that sentence and regret it an hour later.
While they’re talking, you’re already forming:
- Sick vs not sick?
- Airway/breathing/circulation concern?
- Do I need backup early (senior, ICU, rapid response)?
Step 3: At the Bedside – Quick, Focused Exam That Actually Matters
Don’t do a ceremonial exam. Do the exam that answers “Are they crashing or heading there?”
I use a mental mini-ABCD.
A – Airway
Can they speak in full sentences? Any stridor, gurgling, obvious obstruction, vomiting with decreased responsiveness?
If airway is questionable, this is not the time for deep chart review. Call for help.
B – Breathing
- Look: work of breathing, accessory muscles, tripod, cyanosis
- Listen: breath sounds symmetry, wheeze, crackles, absent on one side
- Check: RR yourself; O2 sat and what device
C – Circulation
- Quick pulse check (rate, regularity, weak vs bounding)
- BP on the monitor and maybe repeat manually if weird
- Skin: cool/clammy vs warm, mottling
- Check for obvious bleeding, melena, hematemesis if indicated
- Look at I/O if relevant (esp. sepsis, HF, renal)
D – Disability (neuro status)
- Is this their baseline mentation? Ask the nurse or family.
- Orientation x3, slurred speech, focal deficits, new agitation or lethargy.
You can add whatever’s relevant to the complaint:
- SOB: JVD, peripheral edema, lung exam, cardiac exam
- Abdominal pain: focused abdominal exam, rebound/guarding, check last BM, surgical history
- Fever/sepsis concern: line sites, lungs, urine bag, surgical wounds, skin
This bedside eval should be under 5 minutes unless you’re dealing with a very complex situation or they’re deteriorating.
Step 4: Decide How Sick They Really Are (Triage Level in Your Head)
Now you combine bedside + brief chart review into a mental triage. I think of three buckets:
Red – Potentially crashing / needs immediate escalation
- Hypotension, new O2 requirement or increasing rapidly, altered mental status, chest pain with concerning features, new focal neuro deficits, severe sepsis picture
- Actions:
- Call rapid response or ICU if needed
- Call your senior early
- Start stabilizing orders (fluids, oxygen, labs, EKG, ABG/VBG)
This is not the time to deeply read the discharge summary. Move.
Yellow – Concerning but stable
- New SOB but sats stable on same O2
- New pain but hemodynamically okay
- Mild confusion in a high-risk delirium patient
Actions:
- Focused chart deep-dive targeted at the problem (CHF hx? Recent imaging? Labs?)
- Order a narrow set of tests that answer today’s question, not repeat the resident’s entire admission workup
- Safety-net: nursing parameters (e.g., “Call me if RR > 24, SBP < 90, new O2 need”)
Green – Likely minor problem / symptom management
- Chronic pain requesting adjustment
- Insomnia, constipation, mild nausea
- Stable vitals, no red flags
Actions:
- Quick review for allergy and contraindications
- Symptom-directed treatment
- Inbox message or sticky note for day team if you made a non-trivial change

| Step | Description |
|---|---|
| Step 1 | Page about patient |
| Step 2 | Chart and nurse quick review |
| Step 3 | Bedside ABCD exam |
| Step 4 | Call rapid or ICU |
| Step 5 | Targeted workup and close monitoring |
| Step 6 | Symptom management and handoff note |
| Step 7 | Sick or stable |
That mental model keeps you from both underreacting and overreacting at 3 a.m.
Step 5: Do a Laser-Focused Chart Deep-Dive (Only If Needed)
Once the urgent part is handled or you’ve ruled out crisis, then you zoom in. But not indiscriminately.
Here’s how to do a 5-minute targeted chart review that actually helps you:
Find the last good note with a real assessment.
Usually the attending or senior’s note earlier that day:- What did they think was going on?
- What were the “active problems” and next steps?
- Any “watch out for X” comments?
Check a few key prior data points:
- Labs: last CBC, BMP, lactate, troponin, BNP, LFTs depending on complaint
- Imaging: last CXR, CT, echo if relevant
- Recent events: procedure notes, consult notes from same day
Look at nursing flowsheets briefly.
- Vitals trend
- I/Os over 24 hours
- Pain scores / PRN use

| Category | Value |
|---|---|
| 08:00 | 98 |
| 12:00 | 100 |
| 16:00 | 102 |
| 20:00 | 101 |
| 00:00 | 99 |
| 04:00 | 100 |
- Sanity-check meds vs new problem.
- SOB + on high-dose opioids? Think hypoventilation.
- Confusion + benzos/anticholinergics? Delirium cocktail.
- Bleeding + anticoagulation? Don’t miss this.
Avoid the rabbit holes:
- You do not need to read the full 6-page admission H&P at 3 a.m. unless it’s directly relevant.
- You do not need to read every old discharge summary going back 5 years.
If you catch yourself scrolling more than 5–7 minutes, ask, “What specific question am I actually trying to answer?” If you can’t name it, you’re just procrastinating on making a decision.
Step 6: Communicate Clearly, Document Briefly, Protect Yourself
Overnight, your documentation doesn’t need to be poetry. But it must:
- Show you assessed the situation
- Show your clinical reasoning
- Show what you’ll do if things change
A quick structure that works:
Why you were called.
“Called by RN for increasing shortness of breath in 68-year-old admitted for CHF exacerbation.”Pertinent exam and vitals.
“On arrival: T 37.8, HR 102, BP 112/68, RR 22, O2 94% on 2L (baseline). Mild increased work of breathing. Bibasilar crackles. No JVD increase compared with prior exam per day note.”What you reviewed (briefly).
“Reviewed chart including admission H&P, cardiology note from today, last labs and CXR.”Assessment – 1–2 lines.
“Likely mild progression of volume overload vs anxiety in setting of known CHF exacerbation, currently hemodynamically stable without new O2 requirement.”Plan and safety net.
- “Give additional 20 mg IV furosemide now.”
- “Recheck vitals and O2 sat in 1 hour.”
- “If RR > 24, O2 sat < 90% on >4L, or new chest pain, page on-call resident or call rapid response.”
You don’t need a full problem-based note at night for every Tylenol order. Use this kind of note for anything remotely serious, anything where you changed management in a meaningful way, or anything that made you nervous.

Step 7: Know When to Escalate (And Don’t Be a Hero)
One of the biggest early-resident mistakes I see: trying to “tough it out” alone overnight. That’s how people miss evolving sepsis or a slow GI bleed.
Escalate early if:
- You’re seeing something you’ve never managed before
- You think the patient is okay, but your gut says something’s off
- The nurse or RT is clearly worried
- You’ve already been to the bedside twice for the same issue and it’s not improving
- Vital signs are borderline and trending the wrong way
Escalation can mean:
- Call your senior with a clear, concise SBAR (Situation, Background, Assessment, Recommendation)
- Call rapid response / MET
- Loop in ICU if they’re borderline and might need a higher level of care
Here’s a quick SBAR format that doesn’t waste anyone’s time:
- Situation: “I’m cross-cover for 7W. 68-year-old CHF patient with new increased SOB overnight.”
- Background: “Admitted 2 days ago for acute decomp HF, EF 25%, on 2L O2 at baseline, currently on IV diuresis.”
- Assessment: “RR 24, sat 92% on 3L (baseline 2L), mild increased work of breathing, bibasilar crackles slightly worse than day note, BP stable 118/70, afebrile. Labs from this morning showed stable Cr.”
- Recommendation: “I gave an extra 20 mg IV lasix. I think they’re borderline but okay for now, but I want you to know in case they worsen and to see if you’d add anything or want to see them.”
Your senior will love you for calling like that instead of, “Hey, 7W has this guy who’s kind of short of breath, not sure.”
Step 8: Build Yourself a Simple, Reusable Mental Template
Do this enough nights and you’ll realize you’re basically running the same play over and over with different details.
If you want a simple mental template, here’s one that actually sticks:
- Why are they in the hospital?
- What changed right now?
- Sick or stable? (ABCD at bedside)
- What’s the one worst thing I must rule out?
- What’s my immediate action + backup plan?
That’s it. If your brain is mush at 4 a.m., you can still walk through those five.

Step 9: Common Traps to Avoid
You’ll pick these up faster if someone just tells you directly:
Trap: Reading the whole chart before seeing the patient.
Fix: 2–3 minutes max, then go to the bedside. Sick vs stable first.Trap: Treating numbers instead of the patient.
Example: calling a rapid for a BP of 88/54 in a chronically low BP patient who’s asymptomatic and looks fine.
Fix: Compare to baseline. Look at the human being, not just the screen.Trap: Over-ordering “just to be safe.”
Every SOB is not a CT-PE at 3 a.m.
Fix: Ask, “What will I do differently based on this test tonight?”Trap: Under-documenting when you were actually worried.
Fix: 3–5 sentence cross-cover note for anything causing you genuine concern.Trap: Ignoring your gut because you’re “just a PGY-1.”
If your spidey sense says this patient doesn’t look right, get backup.
| Change Type | Examples to Worry About |
|---|---|
| Respiratory | New O2 need, RR > 24, tripod |
| Hemodynamic | SBP < 90 or MAP < 65 trending |
| Neuro | New confusion, focal deficits |
| Cardiac | New chest pain, arrhythmia |
| Infection/Sepsis | Fever + hypotension + tachycardia |
Your Next Step (Tonight or Before Your Next Call)
Open your note template or a blank page and write out your own 5-step overnight unfamiliar patient script based on this:
- 3 things you’ll always check in the chart before walking in
- 5 questions you’ll ask the nurse every time
- Your bedside ABCD script in your own words
- The 3 big “red flag” situations that will make you call your senior without hesitation
- A 4–5 line note skeleton for cross-cover encounters
Save it where you can see it on your next night shift. When the pager goes off for that unfamiliar patient, you won’t improvise from panic; you’ll just run the play you already wrote.

















