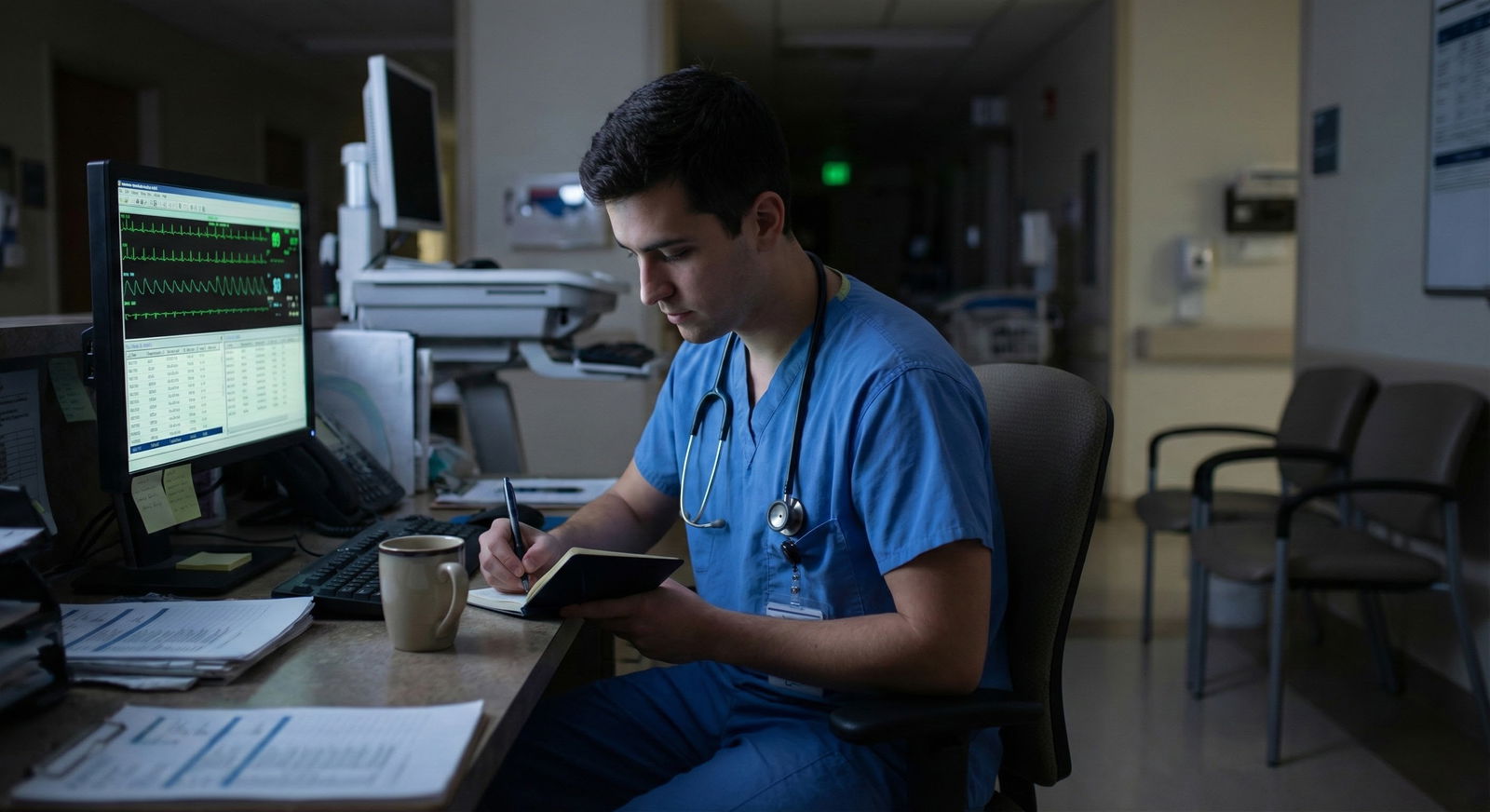
You’re on call. It’s 2:37 a.m. You’ve been up since 5:30 a.m. yesterday. Your senior is scrubbed in a case or stuck at another hospital or just not answering. The nurse just paged you stat about two things at once: chest pain in 3B and a crashing post‑op in PACU. The attending is a name on the schedule, not a person you can see. It feels like you’re the only doctor in the building.
You are not the first resident put in this spot. You will not be the last. The difference is how you handle the next 30–60 minutes.
This is about what to actually do when you’re on call with effectively zero backup.
Step One: Get Your Head Straight in the First 60 Seconds

| Category | Value |
|---|---|
| Routine | 55 |
| Urgent | 30 |
| True Emergencies | 15 |
The first disaster in these situations usually isn’t clinical. It’s psychological. Panic, tunnel vision, and shame (“I should know this”) will hurt patients faster than your lack of experience.
So you give yourself 60 seconds.
Quiet hallway, bathroom, empty call room—doesn’t matter. You do three things, fast:
Name what is happening.
“I am the only in-house doctor right now. My senior is not immediately available. I need to keep people alive until help arrives.” Say it in your head. Reality check.Decide your priority: circulation and oxygenation.
Not “solve the entire problem.” Your job is to keep air going in and blood going around. Everything else is second tier until that’s covered.Pick a structure and stick to it.
Use ABC (airway, breathing, circulation) or “Look, Listen, Feel”:- Look: mental status, work of breathing, bleeding
- Listen: vitals, monitors, what the nurses are telling you
- Feel: pulses, skin temp, diaphoresis
The point is: you can feel as scared as you want, as long as your hands follow a script. Scripts beat panic.
Step Two: Make a Rapid Triage List When Everything Hits at Once
Here’s the scenario you actually get:
- Telemetry calls: “New run of VT, patient asymptomatic.”
- Floor nurse: “BP is 70/40, patient looks pale.”
- PACU: “Sat is 82% on 2L, patient drowsy.”
- ED: “We just got a direct admit from outside, sepsis, can you see them?”
You cannot see everyone at once. So you triage.
Use this mental sorting. It takes 10–20 seconds and will keep you from running in circles.
| Priority Level | Examples |
|---|---|
| Red (Go Now) | Unresponsive, SBP < 80, SpO2 < 88% |
| Orange (Next) | Chest pain, sepsis, arrhythmia |
| Yellow (Later) | Fever, pain meds, high BP |
| Green (Phone) | Sleep aids, bowel regimen, labs |
You respond in this order:
- Red – crashing: hypotension, unresponsiveness, severe respiratory distress, anaphylaxis, uncontrolled bleeding.
- Orange – could crash: chest pain, new neuro deficit, sepsis vitals, serious arrhythmias with symptoms.
- Yellow – uncomfortable but stable.
- Green – stuff that can be handled by orders over the phone or deferred.
You tell nursing honestly what you’re doing:
- “I’m going to 5A first; that patient is hypotensive with altered mental status. I will get there in under 3 minutes. After that I’m coming to you in PACU. Stay on the monitor and call me if SBP drops under 80 or SpO2 under 90 again.”
Nurses understand triage if you explain your priorities. What they hate—and will remember—is silence and vanishing.
Step Three: Use the “3-Question Nurse Handoff” Before You Run
When you get a “come now” page, you do not just run blindly. Spend 10–20 seconds on the phone first. You’ll make better decisions the moment you walk in the room.
Ask the nurse three specific questions every time:
“What are the vitals right now?”
Get numbers. HR, BP, SpO2, RR, temp if relevant.“What is the mental status and work of breathing?”
Alert? Confused? Gasping? Using accessory muscles?“What has already been done?”
Oxygen changed? Fluids started? Meds given? Any allergies?
This does two things. It pre-triages in your head. And it shows the nurse you’re engaged and not just running around reacting.
If the situation sounds truly bad (unresponsive, pulseless, apneic, or close), do the following before you hang up:
- “Call a rapid response / code.”
- “Put them on the monitor and high-flow oxygen / non-rebreather now.”
- “Get a crash cart in the room.”
You’re activating resources that exist even when “the doctor” seems to be only you.
Step Four: Stabilization When Senior Help Is Not Coming (Yet)

Let’s walk through specific high-acuity situations you will actually see when you feel alone. I’ll keep it concrete.
A. Hypotensive, Possibly Septic Floor Patient
You walk in: SBP 70s, tachy 130s, febrile, looks toxic. You can’t get your senior. What you do:
ABC check at the door.
Talking? Then airway and breathing are at least functional for the moment.Oxygen first.
Slap on non-rebreather 15 L if SpO2 < 92% or they look dyspneic.Two large-bore IVs or IO.
If one 22-gauge IV is dripping in the hand, that’s not enough. Ask for 18g or bigger, or an IO if nursing has that capability.Fluids.
You do not need permission to start 1–2 L of crystalloids in a hypotensive adult without cardiogenic shock signs. If they’re elderly with bad EF, you still give a bolus, but you watch closely and reassess breath sounds.Order stat labs.
CBC, CMP, lactate, blood cultures, venous blood gas if available, troponin if chest pain, EKG.Start broad-spectrum antibiotics.
If your hospital has a “sepsis order set,” use it. If not, pick the standard combo you’ve seen your team use 100 times: for example, piperacillin-tazobactam + vancomycin, adjusted to your local protocol.Push for higher level of care.
Call the ICU directly, or call the hospitalist/ICU fellow on-call if your senior is MIA:
“I have a hypotensive patient with probable sepsis, currently on 2 L of fluids, BP 78/40, lactate pending. I need step-up to ICU and help with pressors.”
Can you start pressors? If you’re trained and credentialed and you know how to do it safely through central or appropriately selected peripheral lines, yes. Norepinephrine at a reasonable starting dose while you’re arranging ICU makes sense. If you’ve never seen it done and have zero ICU backup, your priority is volume, early antibiotics, and physically getting this patient to people who do this every day.
B. Chest Pain / Possible ACS
Middle-aged patient, chest tightness, sweaty. Telemetry calls: “New ST depressions.” Senior not answering.
You do this in order:
Vital signs and appearance.
If they’re crashing—hypotensive, altered, gray—you call a rapid/code and treat as such.Oxygen only if hypoxic.
Old habit was oxygen for everyone. Now: oxygen if SpO2 < 90–92% or respiratory distress.Get an EKG in under 10 minutes.
Stand there while they do it. Don’t allow it to be “queued.” You prioritize this yourself.Give aspirin.
325 mg chewable if no contraindications.Pain control.
Nitroglycerin SL if SBP > 100 and not right ventricular infarct suspected. Morphine is not first-line anymore, but if severe pain and you’ve discussed with cardiology before, you know your local style.Call cardiology / ED attending early.
“I have a 58-year-old with new ST depressions in V4–V6, active chest pain, SBP 130/80, HR 90. I’ve given ASA, first EKG is done and I’m sending it to you now. I need your input on next steps and whether you want to activate the cath lab.”
You are not managing the entire ACS algorithm alone. You’re stabilizing and then pulling in the system.
Step Five: When You Literally Cannot Reach Your Senior
This is the part programs rarely talk about openly, but it happens. Pager dead. Phone off. Senior scrubbed in a six-hour case in another building. You’re the PGY-1 or new PGY-2 and something bad is happening.
You need a fallback chain that is not “keep trying the same number.”
Here’s the hierarchy I’ve seen work in real life:
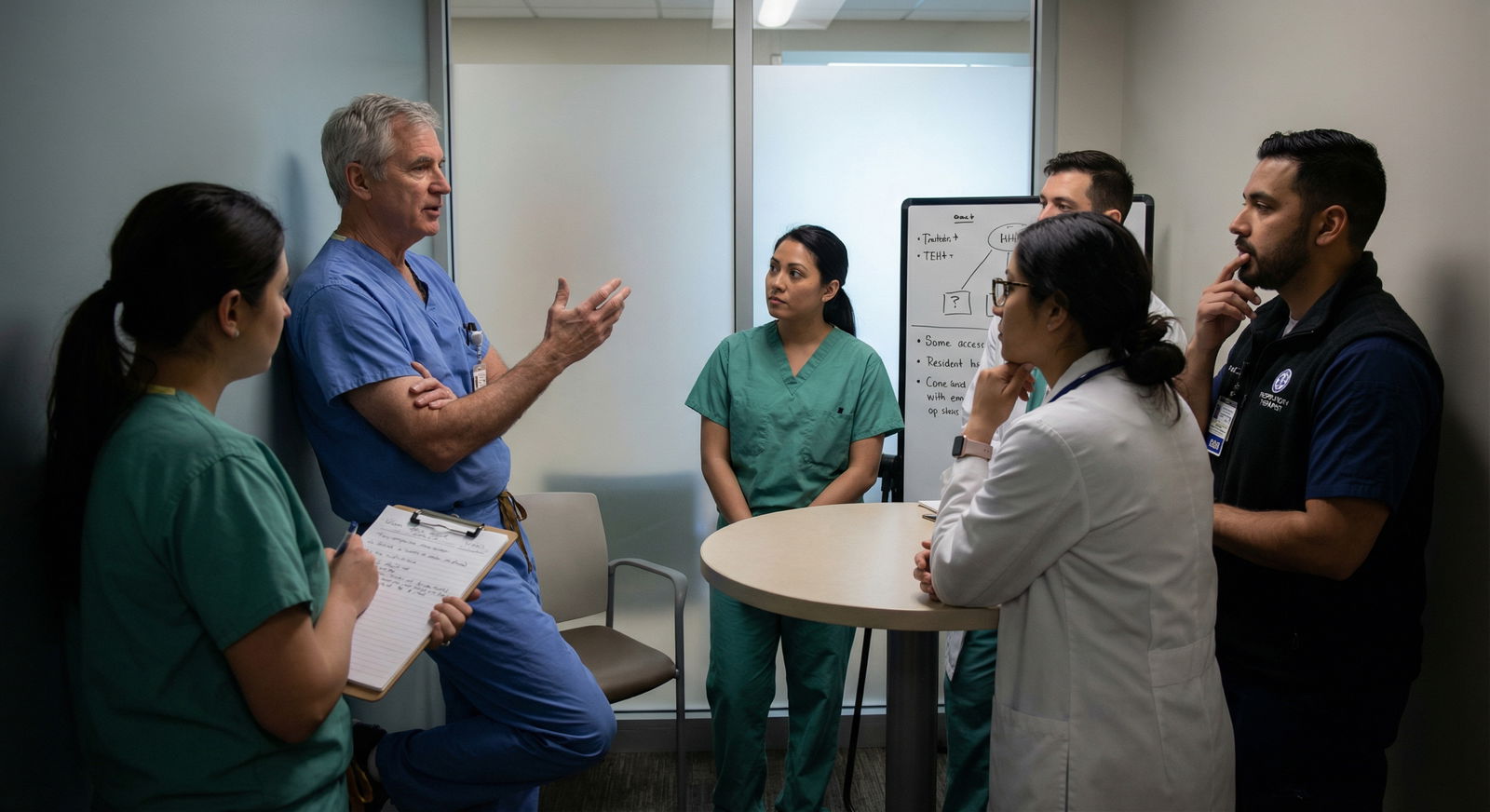
Charge nurse / nurse supervisor.
They know how to escalate inside the hospital. They’ve called attendings, anesthesia, rapid teams, and hospitalists long before you were a med student. Tell them plainly:
“I’ve been trying my senior for 10 minutes without success. This patient is unstable. I need help escalating this.”Identify any in-house physician with critical care skills.
Anesthesia. ICU fellow. ED attending. Hospitalist in the building. You say:
“I’m the overnight resident for X service. My senior is unavailable and I have a crashing patient. Can you assist at the bedside?”Call the attending yourself.
This feels terrifying as a junior. Do it anyway. Script it:
“Dr. Smith, I’m the PGY-1 on call. I’ve been unable to reach my senior for 15 minutes. I have a patient with [one-line summary: hypotensive, unresponsive, severe dyspnea]. I’ve done [specific steps]. I need your guidance right now.”
Most attendings will be more upset you didn’t call than that you “bothered” them.
- Document the escalation later.
Not in a petty way, but to protect future patients. Email your PD or chief with a factual description. Programs need to know when coverage systems are failing.
Step Six: Use Scripts When You Don’t Know the Perfect Answer
Most of the fear at 3 a.m. isn’t “I don’t know anything.” It’s “I don’t know the perfect thing and I’ll sound stupid.”
You don’t have time for that. Use scripts.
When a nurse calls with a concern you don’t fully understand, say:
- “Okay, I’m coming to see the patient now. While I’m on the way, please put them on a monitor, get a full set of vitals, and start an EKG if chest pain or arrhythmia is suspected.”
When you’re calling someone more senior for help, say:
- “I’m worried about this patient because…” and give 1–2 concrete facts (vitals, mental status, lab or EKG change).
- Then: “So far I’ve done…” and list what you’ve already initiated.
- Then: “My specific questions are…” with 1–2 targeted asks.
This turns you from “panicked intern” into “junior physician taking action and seeking targeted backup.”
Step Seven: Protect Yourself From Classic 3 a.m. Mistakes

| Category | Value |
|---|---|
| Delay calling for help | 40 |
| No re-check vitals | 30 |
| Over-sedation | 10 |
| Missed sepsis | 15 |
| Bad documentation | 5 |
A lot of night disasters are not esoteric. They’re the same 5–6 mistakes repeated.
Here are the ones I’ve seen over and over, and how you avoid them when you’re basically solo.
Not repeating vitals.
One set of vitals is a snapshot, not a story. If something concerns you, you order repeat vitals q15–30 min until stable. You can literally write that order.Ordering sedatives on unstable or unknown patients.
Patient “agitated” with unclear cause? No vitals? Unknown respiratory status? Do not reflexively push lorazepam or opioids from your bed. Go see them. Agitation can be hypoxia, hypoglycemia, sepsis, stroke, withdrawal. Sedation without assessment is how people stop breathing.Forgetting to check fingerstick glucose.
Altered? Weird behavior? Unresponsive? Check a glucose. It’s quick, and you’ll feel ridiculous if you missed it.Ignoring nursing intuition.
If a nurse you trust says, “I just don’t like how this patient looks,” go see them. That’s not superstition; it’s pattern recognition from thousands of patient encounters.Not documenting what you did in real time.
You don’t need a novel, but you want a timestamped, focused note:- Why you were called
- What you found (vitals, exam)
- What you did (orders, discussions, calls made)
- Your impression and plan
It protects you and your patient, especially when backup was delayed or absent.
Step Eight: Know What You Can Safely Say “No” To
Being alone on call doesn’t mean you say yes to everything.
Examples where “no (for now)” is correct:
Request for routine sleep meds in a stable patient while you’re managing an unstable one.
“I’m managing a critical situation right now. I can’t safely come adjust sleep meds yet. Please offer non-pharmacologic measures; I’ll re-evaluate in an hour.”Request to come re-consent a stable patient for something elective at 1:30 a.m.
No. That can wait for daytime.Pressure to discharge someone quickly because “transport is here” while you have real medical concerns.
You’re the doctor. If they’re not safe, they don’t leave.
You’re prioritizing survival and serious morbidity. Not customer satisfaction scores at 2 a.m.
Step Nine: Debrief the Next Day (Even If No One Asks)

| Step | Description |
|---|---|
| Step 1 | Post Call |
| Step 2 | Write Brief Timeline |
| Step 3 | Identify 1-2 Good Moves |
| Step 4 | Identify 1-2 Mistakes |
| Step 5 | Ask Senior for Feedback |
| Step 6 | Adjust Mental Checklists |
After a night where you were flying solo, your instinct might be to just sleep and forget it. That’s how people repeat the same errors.
Do a quick debrief with yourself before you crash:
- Write down a 5–10 line timeline: what happened, when, what you did, when backup finally arrived.
- Circle 1–2 things you did well. Keep that.
- Circle 1–2 things you never want to repeat.
Then, when you’re human again, find someone you trust—senior resident, chief, attending—and say:
“I had a rough call where my senior was unreachable for a while. Here’s what happened. Can we walk through what I did and what you’d adjust?”
If they’re dismissive or hand-wavy, fine, move on. But the ones who sit down and really dissect it with you—those are the people you attach yourself to for the rest of residency.
Step Ten: Long-Term Fixes So You’re Not Alone Again
Most residents treat these “abandoned on call” nights as bad luck. Sometimes it is. Sometimes it’s a system problem your program needs to fix.
You can push that conversation without sounding like you’re whining.
Bring specific facts:
- How long your senior was unreachable.
- Who you called instead.
- What kind of patient situation you were in (no PHI, just level of acuity).
- What resources were and were not available.
Then say something like:
“I’m not asking to be protected from responsibility. I am asking for a clear, reliable backup chain so that when the senior is scrubbed or off-site, we know exactly who to call and how fast they’ll respond.”
Programs listen more when you talk systems and safety, not vibes and feelings.
Final Thoughts
Three things to keep in your pocket for the next time you feel like the only doctor in the building:
- Stabilize first, perfect later. Airway, breathing, circulation. Oxygen, IV access, fluids, monitors. You don’t need the final diagnosis to start life-saving basics.
- Use the system, not just people. Charge nurses, rapid/ICU teams, ED, anesthesia, attendings. If your senior is a ghost, climb the ladder anyway.
- Debrief and upgrade your script. Every rough call can either traumatize you or upgrade your internal playbook. Write it down, review it, and next time you’ll be scared—but faster, sharper, and more effective.


















