It is mid-January. You just finished an interview day at a “solid” internal medicine program. The PD talked a big game about their fellowship matches. The slide with logos from MGH, UCSF, Penn, and Duke flashed by in 12 seconds. Everyone nodded. You smiled.
Now you are home. You open FREIDA and the program’s website. Their “recent fellowship placements” list looks suspiciously cherry-picked. Two names per specialty. Nothing about who did not match. Nothing about which grads had to scramble to community programs after a re-app. And you realize: if you match here, your entire fellowship trajectory may ride on what this program actually does for subspecialty placement.
That is what this piece is about: using your second look (formal or informal) as a surgical tool to dissect a program’s true fellowship placement patterns. Not vibes. Data.
Let me break this down specifically.
Step 1: Get Clear On What “Good Fellowship Placement” Really Means
Before you can use a second look to evaluate fellowship outcomes, you need a clear framework. Programs love to play optics games. They will proudly mention “we send residents to top programs every year” based on one unicorn match in the last decade.
For fellowship placement, you care about four core dimensions:
- Match rate
- Tier of programs matched
- Internal vs external matches
- Alignment with resident goals (i.e., research vs clinical, academic vs community)
Think about them like this.
1. Fellowship Match Rate
You want to know: Of residents who apply for fellowship, how many match, and how many match on the first cycle?
Most programs will not hand you a spreadsheet, but they often leak enough information with careful questioning.
At your second look, your goal is to triangulate:
- Rough percentage of applicants matching each year
- Which specialties are consistently strong (cards, GI) and which are weak
- How often people re-apply, take chief years to strengthen applications, or pivot to hospitalist jobs when they actually wanted fellowship

| Category | Value |
|---|---|
| Program A | 90 |
| Program B | 75 |
| Program C | 60 |
| Program D | 50 |
A program that consistently matches ~85–90% of fellowship applicants across specialties is different from one where <60% of residents land a spot on their first try. You want to sniff that out.
2. Program Tier
“Top fellowship placement” is meaningless unless you define the tier.
Think in rough buckets:
- Tier 1: National powerhouse (MGH, BWH, UCSF, Penn, Duke, Hopkins, etc.)
- Tier 2: Strong regional academics (UTSW, Emory, Colorado, UMich, Mayo AZ/FL, etc.)
- Tier 3: Solid university/community hybrids or strong regional programs
- Tier 4: Purely community fellowships with limited research & academic exposure
Different goals, different targets. If you want academic cardiology with R01-type research, Tier 1–2 matters. If you want to be a clinically strong pulmonologist in your hometown, Tier 3–4 might be fine.
Your second look is where you stop letting programs toss around logos and instead pin down distribution.
3. Internal vs External Matches
Key question: Is this a place where everyone just “stays for fellowship” because the outside options are weak? Or is it a national launching pad?
A healthy program usually has:
- A strong internal pipeline for the fellowships they actually do well
- A consistent pattern of residents matching externally at peer or higher-tier places
A concerning pattern:
- Fellowship matches are predominantly internal, and you rarely hear about people going to better-known national programs. That often means the program is insular and not competitive on the national stage.
4. Alignment with Resident Goals
Raw match lists lie by omission. Your job is to figure out:
- Are the residents with serious research interests landing research-heavy programs?
- Are clinically focused residents ending up in fellowships that fit their profile?
- Or does everyone seem to “settle” for whatever is available?
You are not just evaluating a list of logos. You are evaluating whether this ecosystem genuinely supports different fellowship trajectories.
Step 2: Pre–Second Look Homework (So You Do Not Waste The Visit)
You cannot walk into a second look cold and expect to get meaningful intel. Show up with a preliminary mental model and then use the visit to sharpen or demolish it.
Here is what to do before you step back on campus.
Scrutinize The Public Match Lists
Open the program website. Screenshot their “recent fellowship matches.” Then actually sort them.
You want to extract:
- Specialty counts (How many cards, GI, onc, pulm, renal, ID, etc. over 3–5 years?)
- Program tiers (How many truly national programs? How many regional?)
- Internal vs external rates
If a program shows “our residents have matched at X, Y, Z top institutions” but you only see one person at each over a decade, that is marketing, not pattern.
| Specialty | Total Fellows | Tier 1–2 Programs | Internal Matches |
|---|---|---|---|
| Cardiology | 10 | 6 | 3 |
| GI | 6 | 3 | 2 |
| Heme/Onc | 8 | 4 | 4 |
| Pulm/CC | 7 | 2 | 5 |
You are looking for consistency. One random “MGH GI” does not make a pattern. Three GI fellows in 5 years at top programs does.
Use Backdoor Intel
Talk to:
- Recent alumni from your med school who matched there
- Residents from adjacent programs in the same city
- Subspecialty fellows you met on away rotations or conferences
Ask very specific questions:
- “Who are the last 3–4 residents from there who matched competitive GI or cards, and where did they go?”
- “Do you see their residents matching at your fellowship?”
- “Would you say their residents are considered strong applicants nationally, or more locally known?”
By the time you schedule a second look, you want at least a working hypothesis: “This place seems strong for pulm/CC and heme/onc, middling for GI, weak for cards.”
Your second look is where you confirm or overturn that.
Step 3: Design Your Second Look Around Fellowship Intel
Most people treat second looks like a vibes check: “Do I like the city? Are people friendly?” That is fluff. You can get vibes on interview day.
For fellowship-focused second looks, you engineer the day around three nodes:
- PD/APD conversation
- Targeted chats with subspecialty fellows and interested residents
- Quiet reality check with rising seniors applying to fellowship now
Let us go through each.
1. The PD / APD Conversation: Force Specifics
You are not going to get raw match-rate spreadsheets. But you can absolutely force the leadership to get specific.
Questions that cut through the fog:
- “For residents who seriously pursue competitive subspecialties like cards and GI, what proportion typically match on the first application cycle?”
- “In the last 5 years, how many of your cards / GI / heme-onc applicants matched at outside academic programs vs internal?”
- “Can you walk me through where your last 5 cardiology applicants ended up?”
Then: shut up and let them talk.
Red flags:
- They pivot to “we support whatever you want to do” without giving numbers.
- They only highlight one or two unicorn matches repeatedly.
- They mix in “some people chose hospitalist jobs” suspiciously often instead of acknowledging non-matches.
Reasonable answers will sound like:
“For GI, in the last five years we had 7 applicants. Six matched on their first try, one did a chief year then matched. Three stayed here, four went to places like [X, Y, Z].”
That is the kind of pattern you can work with.
2. Subspecialty Fellows: The Most Honest Dataset
This is where second looks can be gold. You want time with fellows in your target specialty, especially those who trained at that program for residency.
Ask for this explicitly when you arrange the second look:
“I am strongly considering a career in [cards/GI/onc]. I would really appreciate meeting one or two fellows who did residency here and successfully matched, and maybe someone who trained elsewhere but knows your residents.”
When you get that meeting, do not waste it on “How do you like the fellowship?” You are there to dissect the pipeline.
Concrete questions:
- “Among your co-residents who wanted fellowship, how many actually matched, and where?”
- “Were there people who had to re-apply or pivot to hospitalist work after not matching?”
- “When you applied, did you feel your letters, research, and mentorship were competitive on the national stage?”
- “How known is this program’s IM residency among fellowship PDs at the places you interviewed?”
Listen for tone. Fellows are usually more blunt than residents. They will tell you if:
- “Our cards matches are almost always internal; it is tough to break out nationally without a big research portfolio.”
- “Once you are here and productive, you can go pretty much anywhere for pulm/CC; our PD has strong connections.”
That is the data you came for.
3. Rising Seniors Applying Now: Real-Time Signal
The most underused resource on a second look is the current PGY-3 cohort deep in ERAS for fellowship.
Ask the coordinator or chief to arrange informal time with:
- A PGY-3 applying in your target specialty
- A PGY-3 applying in a different competitive subspecialty
You want live, unpolished information:
- “How many interviews did you get?”
- “Were the places where people last year matched the same places you are interviewing?”
- “Do you feel the program protected your time for research / electives / away rotations to build a competitive application?”
These people are still in the game; their perception of institutional support is very revealing.
Step 4: Tactical Question Sets By Scenario
Let me give you specific scripts you can actually use. Because vague “ask about fellowship” is useless.
If You Want a Top-Tier Research Fellowship
Your angle: “Can this program launch me into a national research track?”
Questions to ask faculty / PD:
- “For residents aiming for research-focused fellowships (e.g., cards with T32 track), how many in recent years have matched to those paths?”
- “Can you name a few residents from the last 5 years who went into research-heavy fellowships, and where?”
- “Do residents commonly get first- or second-author publications before applying to fellowship? In what kind of journals?”
Questions to ask fellows:
- “Did you feel your research CV was competitive compared to co-fellows from big-name residencies?”
- “Who actually mentored your fellowship application—IM leadership, or subspecialty faculty?”
You are looking for evidence that they have a reproducible pathway to high-level academic placements, not just one superstar who walked in with 20 publications.
If You Want a Strong Clinical Fellowship, Not Necessarily Famous
Your angle: “Will I reliably land in a good clinical program that fits my geographic or lifestyle goals?”
Questions:
- “Among residents who wanted [nephrology/ID/endo], did everyone who applied eventually match somewhere they were comfortable with?”
- “For less competitive fellowships, how many people choose to stay versus leave, and is that driven by quality or lack of options?”
- “How flexible is your schedule for away rotations at specific programs I might want to match at?”
You want pattern + support, not just blind optimism.
Step 5: Decode Red Flags And Green Flags From What You Hear
Second looks can overload you with anecdote. You need a mental filter.
Fellowship Placement Green Flags
These are signs a program actually understands and supports the fellowship game:
- The PD and chiefs can rattle off recent match outcomes from memory, including those who did not match and what happened next.
- There is a culture of early mentorship: PGY-1s with fellowship interest are paired with subspecialty faculty within months.
- Fellows and residents both describe strong advocacy from leadership when it comes to letters and networking.
- Match lists show both solid internal placements and consistent external matches at equal-or-better-tier programs.
- People can name multiple alumni currently in high-level fellowships or faculty positions, not just one name they put on every slide.

| Category | Value |
|---|---|
| Internal | 40 |
| Regional Academic | 30 |
| National Top Tier | 20 |
| Community | 10 |
Fellowship Placement Red Flags
These should make you pause:
- Leadership hand-waves specific numbers and talks only in generalities: “Our residents do very well.”
- The only examples of “top” matches are several years old, or always the same one or two names.
- Fellows subtly frame things like: “If you are really motivated and do a lot on your own, you can get where you want.” Translation: the system will not help you much.
- Residents applying right now seem anxious and uncertain about their prospects or feel under-mentored.
- The program heavily emphasizes hospitalist or primary care jobs while hand-waving subspecialty outcomes.
Programs can be fantastic clinically and still mediocre for fellowship. That might be fine for you. But you want to know it before you sign up.
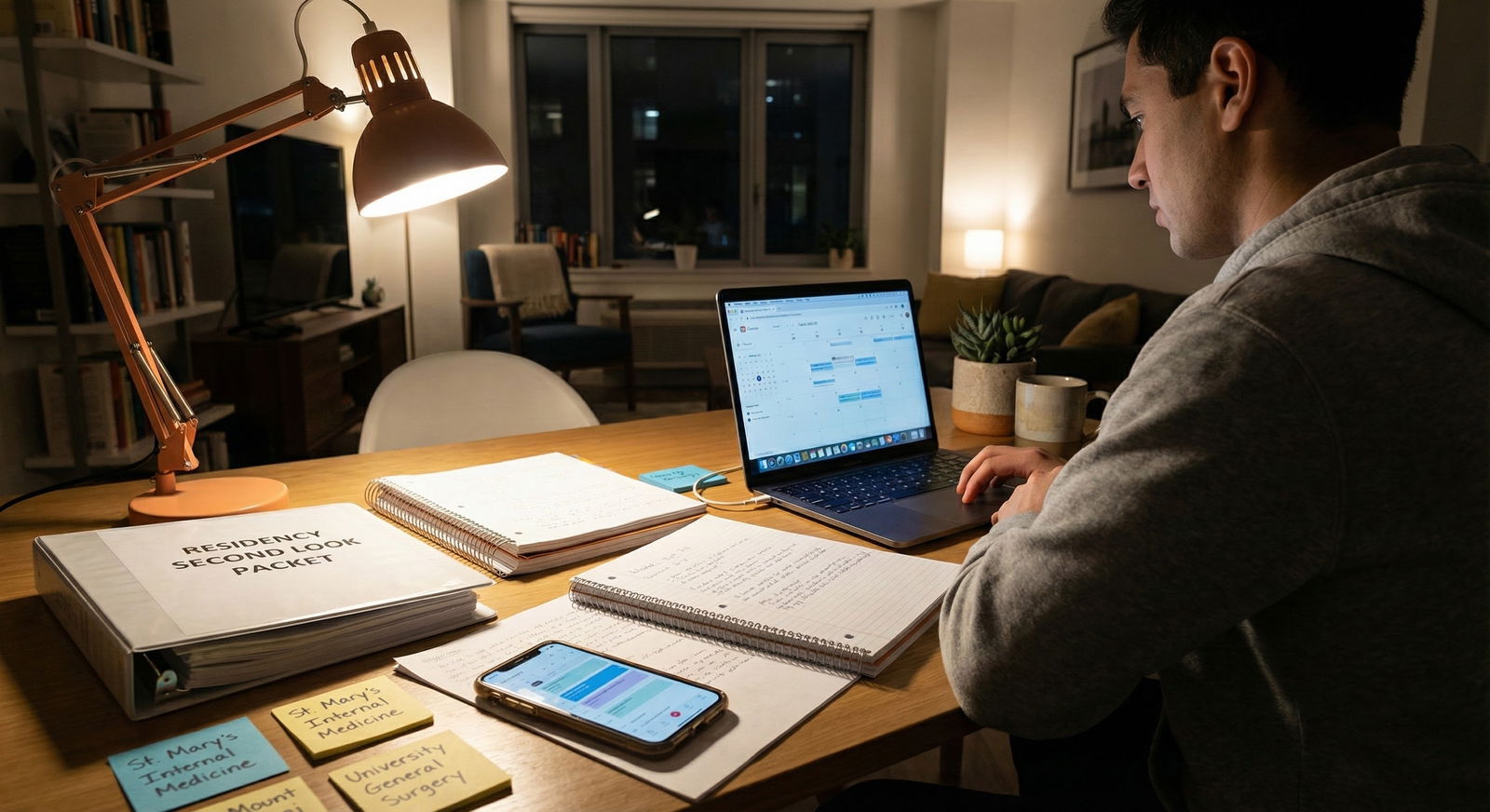
Step 6: Map Observations To Your Own Risk Tolerance
All this intel only matters relative to your own risk profile and goals.
Use a Simple Internal Scoring Framework
After your second look, literally sit down and rate the program on a few axes (1–5):
- Overall fellowship match rate among applicants
- Competitiveness of fellowships achieved in your target specialty
- Consistency of outcomes (year-to-year vs unicorns)
- Strength of mentorship / advocacy
- Research infrastructure and access (if relevant)
| Dimension | Score (1–5) | Notes |
|---|---|---|
| Match Rate | 4 | Most applicants match on first try |
| Competitiveness | 3 | Strong regionally, few national matches |
| Consistency | 4 | Yearly placements in target field |
| Mentorship | 5 | Multiple faculty proactively involved |
| Research | 3 | Some projects, limited T32 exposure |
Then ask yourself:
- Do I need a nationally recognizable name for what I want to do?
- Would I be content with a strong regional academic or community fellowship that trains me well clinically?
- Am I excited enough about this program’s day-to-day training that I would accept a slightly weaker fellowship trajectory?
The second look gives you inputs. The decision is still yours.
Step 7: Future-Proofing – How The Fellowship Game Is Changing
You asked for “Miscellaneous and Future of Medicine,” so let us zoom out for a minute. Fellowship placement is not static. The rules are shifting under your feet.
Three evolving trends you should keep in mind while interrogating programs:
1. Increasing Competitiveness in Historically “Safe” Fields
Nephrology and ID used to be “backup” specialties. That has been changing in certain regions and niches (transplant neph, critical care ID, etc.), particularly where advanced procedures and complex care draw more applicants.
During your second look, ask:
- “Have you seen application patterns change for previously less competitive fellowships?”
- “Are there fellowships where your residents used to easily match that are now requiring stronger portfolios?”
Programs that are paying attention to the national landscape will have a coherent answer.
2. Virtual Networking and Letters Matter More
With more virtual interviews and less in-person away time, your program’s national visibility and your letter-writers’ reputations carry even more weight.
On second look, probe:
- “How well known are your subspecialty faculty on the national stage? Are they involved in guideline committees, specialty societies, multi-center trials?”
- “Do your residents present at national meetings frequently?”

| Category | Value |
|---|---|
| Year 1 | 5 |
| Year 2 | 9 |
| Year 3 | 14 |
| Year 4 | 18 |
You want a program that is not just training solid clinicians but also inserting its residents into national conversations.
3. Shifting Workforce Needs
The demand for certain subspecialties (e.g., critical care, geriatrics, addiction medicine) is changing. Some fellowships may get more funding and spots; others might stagnate.
Ask:
- “In which subspecialties do you see your residents having the easiest time matching?”
- “Where do you anticipate the most growth in fellowship opportunities over the next 5–10 years?”
You are partly betting on a moving target. Programs that take workforce trends seriously will talk about it explicitly.
Putting It All Together On Second Look Day
Let me give you a simple operational blueprint for the day itself.
Morning: PD / APD + Chiefs
- Clarify data: approximate match rates, recent patterns, internal vs external breakdown
- Ask direct “last 5 applicants in X field—where are they now?” questions
Midday: Meet fellows in your target field
- Dissect real trajectories of recent residents
- Ask about research, letters, and national reputation
Afternoon: Sit with PGY-3s currently applying
- Get real-time sense of interview invites and perceived support
- Ask if their experiences matched what they were told as interns and applicants
End of day: Quiet 30 minutes alone
- Jot down names, programs mentioned, specific examples
- Score your axes (match rate, competitiveness, consistency, mentorship, research) while it is still fresh
Then compare that against your other top programs. Not based on food, social hour, or “we’re a family,” but on actual career trajectories.
FAQ (Exactly 5 Questions)
1. How do I ask about non-matches without sounding aggressive or rude?
Phrase it as concern for support rather than accusation. For example: “I know not everyone matches on the first try in competitive fields. How do you support residents who do not match initially, and can you share what has typically happened with them?” A confident program will answer directly. A defensive program will dodge.
2. Is a program “bad” if most fellows stay internal rather than going elsewhere?
Not automatically. If the internal fellowships are strong, well-recognized, and graduates do well afterward, an internal-heavy pattern can be fine. It becomes concerning when there are few or no external matches and the internal fellowships are not especially strong or well-known. That suggests insularity, not excellence.
3. Should I worry if a program does not have an in-house fellowship in my target field?
It depends on your goals. Lack of an in-house fellowship forces you to apply externally, which is riskier, but some residencies without home programs still have strong external match patterns due to good mentorship and regional relationships. On your second look, ask explicitly: “Without a home fellowship in X, how have prior residents interested in X done in the match?”
4. How much weight should I give to one superstar match (e.g., UCSF GI) from several years ago?
Very little, on its own. One outlier usually reflects a single resident’s exceptional CV, not the program’s default pipeline. What matters is whether there are multiple examples in the last 5–7 years in your field of interest and whether those residents had institutional support or succeeded purely on their own steam.
5. If a program is clinically amazing but fellowship placement is just average, should I still rank it highly?
If your goals are flexible—open to hospitalist work, primary care, or non-competitive fellowships—strong clinical training can reasonably outweigh a mediocre fellowship track record. If you are dead set on a highly competitive subspecialty at a top academic center, an “average” placement record is a real risk. In that case, you should only rank it highly if your other options are significantly worse, or if you are prepared to do extra work (research, networking, away rotations) to compensate.
Key takeaways:
First, use your second look as a targeted interrogation of fellowship patterns, not a vibes tour. Push for specific, recent examples. Second, talk to three groups—PDs, fellows, and PGY-3s—and cross-check their stories. Third, map what you learn to your own risk tolerance and goals; a program can be clinically superb but fellowship-mediocre, and that distinction will matter far more to you five years from now than the coffee on interview day.
















