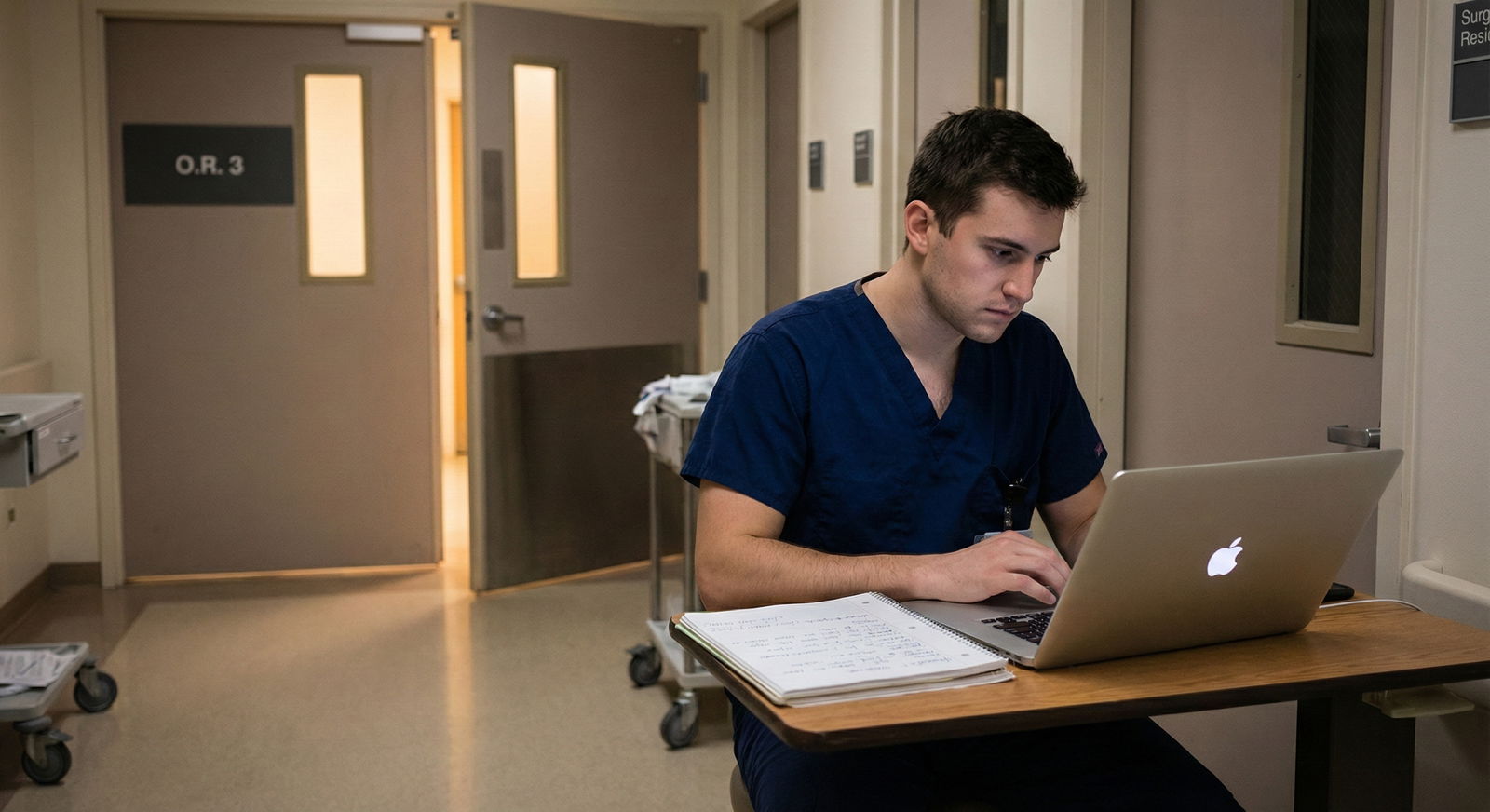
It is 4:17 a.m. You are on a surgery month, pager still quiet, and you know there is a full OR slate today. You also know that by 10 a.m., a consult or add-on case will pop up. The question is not if there will be extra cases. It is whether you will be positioned to take them.
Residents who consistently grow their surgical case volume do not “get lucky.” They run a 24‑hour routine that makes them the default answer when someone asks, “Who can do this case?”
Here is that routine. Hour by hour. At each point: what you should be doing to position yourself to capture extra OR time.
The Night Before: 18:00–23:00 – Setting Up Tomorrow’s Volume
At this point you should stop thinking about today’s chaos and set up tomorrow’s opportunities.
18:00–19:00 – Post‑Op Wrap and Intel Gathering
You are finishing cases or floor work. Before you walk out:
Hit the board and tomorrow’s schedule.
- Check:
- Finalized OR schedule for tomorrow.
- “Open” rooms or “Add-on” slots.
- Surgeons with historically chaotic lists (they create opportunities).
- Identify:
- Which rooms you are already assigned to.
- Which rooms are uncovered or loosely assigned (“resident TBD,” “PA,” or “none”).
- Check:
Talk to the charge nurse and OR board runner.
Five‑minute conversation that can double your case numbers over a month.- Ask:
- “Which rooms usually run late tomorrow?”
- “Which surgeons often add cases day-of?”
- “Any big cases where you will need an extra pair of hands?”
- Say explicitly: “If you get an add-on and need a resident, page me first. I want the cases.”
- Ask:
Quick debrief with your attendings for tomorrow.
- Ask:
- “What time are you planning wheels in?”
- “Any chance of add-on cases or late cases tomorrow?”
- “Would you be okay if I scrubbed into any emergency / add-on cases with you if they come up?”
- Ask:
You are seeding tomorrow’s volume before you leave the hospital.
19:00–20:00 – Targeted Case Prep (Not Endless Reading)
This is not the time for general “read about appendicitis.” It is sniper‑level prep.
Pick 2–3 priority cases from tomorrow’s list:
- Complex / rarely available (e.g., Whipple, re-do laparotomy, major vascular).
- With attendings who control lots of volume.
- With potential for intra‑day add-ons (e.g., ACS, vascular, ortho trauma).
For each priority case, spend 15–20 minutes on:
- Indication, anatomy, and key steps.
- Usual intra-op decision points.
- Your role: where a resident can actually do something meaningful (ports, dissection planes, exposure, closure).
Have one pearl and one question ready for each case. You want to sound prepared at 06:45, not like you skimmed UpToDate in the locker room.
20:00–21:30 – Logistics and Sleep Protection
At this point you should be making sleep possible and morning delays impossible.
- Layout:
- Scrub cap, compression socks, badge, hospital shoes.
- Call bag stocked (charger, snacks, caffeine, backup pen).
- Check:
- Tomorrow’s call status. If you are post-call the following day, you might get more flexibility to stay late tonight versus tomorrow.
- Set:
- Two alarms: 1st wake up, 2nd “you must leave your apartment/house now.”
Aim for a 6–7 hour minimum sleep block if you are not on in-house call. Residents who think they can function on three hours every night stop learning technique. They just survive.
21:30–23:00 – Soft Shutdown
No heroic productivity sprints here. You are tuning your brain for high‑stakes motor learning.
- 10–15 minutes:
- Mentally rehearse tomorrow’s biggest case stepwise.
- Visualize your hands, your instruments, your positioning.
- Then stop.
Phone away. Blue light down. If you “just check the schedule one more time” at 22:45, you will find something that keeps you up another hour. Do not do it.
Early Morning: 04:00–06:30 – Owning the List and the Board
This is where people either own the day or chase it.

| Period | Event |
|---|---|
| Evening Before - 18 | 00 |
| Evening Before - 19 | 00 |
| Evening Before - 20 | 00 |
| Morning - 04 | 30 |
| Morning - 05 | 30 |
| Morning - 06 | 30 |
| Midday - 10 | 00 |
| Midday - 13 | 00 |
| Late Day - 16 | 00 |
| Late Day - 18 | 00 |
04:00–04:30 – Wake, Scan, Prioritize
Before you leave home, 10 minutes of deliberate review:
- Check:
- Any overnight changes to the OR board.
- New consults or ED admits that might become add-ons.
- Decide:
- Your “must not miss” cases.
- Which parts of rounds can be streamlined or delegated so you are not pulled from the OR later.
At this point you should know: the single most important case you need from this day.
04:30–05:30 – Pre‑Round with Purpose
You are not just checking boxes. You are eliminating reasons for cancellations and delays.
For first-case patients and high-yield cases:
- Verify:
- NPO status.
- Anticoagulation management.
- Labs done and resulted (Hgb, Type & Screen, BMP, etc.).
- Imaging available and labeled correctly in PACS.
- Fix problems before they surface:
- Missing consent? Get it.
- Unclear side/level? Re‑confirm with patient and chart.
- Questionable optimization (e.g., hypertensive, on O2)? Call anesthesia or medicine early.
When an add-on comes at 11 a.m., anesthesia and OR staff decide who they trust to not create a disaster. They remember the resident who always has labs, consent, and imaging sorted.
05:30–06:15 – Consents, Orders, and Anesthesia Alignment
At this point you should be physically near your first‑case patients and the OR.
Consents: zero tolerance for sloppiness.
- Correct procedure name.
- Correct side.
- Clear documentation of indications and major risks.
- Mark the site early if allowed by local policy.
Pre‑op orders and checklists.
- Antibiotics timed.
- DVT prophylaxis plan clear.
- Blood products ordered and available if relevant.
Track down anesthesia early.
- “For Ms. X at 7:15 – labs are good, she is NPO, consent is signed, imaging is in PACS under today’s date. Anything else you need?”
- Plant the idea: “If any urgent case comes in today and you need a resident who will have everything ready, I am happy to take it.”
You are quietly branding yourself as “the path of least resistance” for extra cases.
06:15–06:45 – Board Check and Attending Touch-Base
Head to the OR board in person.
- Identify:
- Rooms that still say “TBD” under assistant.
- Cases with two surgeons scrubbed (possibility to be a second resident).
- Long, multi‑stage cases where an extra pair of hands is genuinely useful.
Walk to each attending you might work with today:
- “I saw you have a [case] at [time]. I am free between [X–Y]. I would like to scrub that if you are okay with it. I will be completely ready.”
No one is going to hunt you down and invite you into their cases. You have to ask. Early. Calmly. Professionally.
Pre‑Case and Early OR Time: 06:45–09:00 – Showing You Add Value
Now you are in the room. This part matters more than you think.
06:45–07:15 – Pre‑Induction Setup
At this point you should be doing the unglamorous work fast and well:
- Positioning.
- Foley placement.
- Line setup if needed.
- Padding and pressure point protection.
- Making sure all essential instruments and special equipment are available.
Why? Because when a trauma or emergent case arrives at 10:30, the scrub nurse will tell the charge nurse: “Get [your name], they do not slow us down.”
07:15–09:00 – Intra‑Op: Learn, Then Advertise (Subtly)
Two goals here:
- Actually improve your operative skill.
- Signal to the attending and staff that giving you more cases is a good investment.
Practical approach:
- Be one step ahead instrumentally and anatomically.
- Ask 1–2 targeted questions that show prep, not insecurity.
- Volunteer for:
- Exposure.
- Suturing.
- Closing (and close well, meticulously, without drama).
Near the end of the case, as you are closing or writing the op note:
- “I am free later this afternoon between [X–Y]. If anything urgent pops up or if you want help on additional cases, I would like to scrub those too.”
You are training attendings to think of you as “the resident who wants more volume and does not make my day harder.”
Midday: 09:00–15:00 – Hunting Extra Volume Without Neglecting Service
Middle of the day is where extra cases either appear or evaporate.

| Category | Value |
|---|---|
| ED/Trauma | 40 |
| Urgent Consults | 25 |
| Schedule Add-ons | 20 |
| Coverage Gaps | 15 |
09:00–10:30 – Quick Rounds, Then Scout
At this point you should have rounded cleanly enough that:
- Dispositions are in motion.
- Orders are in.
- Pages are not exploding.
Then you walk.
Check the OR board again.
- Any new add-ons?
- Any cases moved rooms or times?
- Any rooms behind schedule?
Visit the ED / admission points.
- Touch base with:
- ED physician.
- Surgical consult/triage resident.
- Line you use: “If you have any surgical patient going to the OR and need someone to staff the case or help with consent, page me.”
- Touch base with:
Your goal is simple: you want to be notified at the ordering of the OR case, not when the patient is already rolling.
10:30–13:00 – Swapping, Stacking, and Being Visible
This is prime time for add-ons and coverage gaps.
Tactics that work:
Know your team’s bandwidth.
- If a co‑resident is drowning in floor work and has a low‑yield case, trade:
- “I will take your scut and notes for an hour if you let me scrub this lap chole / fracture fixation.”
- Done respectfully, this grows everyone’s case counts.
- If a co‑resident is drowning in floor work and has a low‑yield case, trade:
Offer to cover breaks intelligently.
- Tell the charge nurse: “Between 12 and 14 I can cover cases for resident lunch breaks. If an interesting case is running, I would like to help.”
- You scrub in, do part of the case, and build a reputation.
-
- If your first attending has a quick follow‑up case and there is no assigned resident:
- “Can I stay and scrub the next case with you as well? My floor work is handled and I am up to date on the patient.”
- If your first attending has a quick follow‑up case and there is no assigned resident:
You are designing your day so that every 90‑minute window has the maximal number of minutes in the OR consistent with not being a terrible teammate.
13:00–15:00 – Protecting Late Afternoon Volume
Temptation kicks in here. People start thinking about going home. You should be thinking about 16:00–20:00.
This window is where many ED‑to‑OR patients materialize:
- Appys.
- Choles.
- Abscesses.
- Trauma washouts.
- Ortho fractures.
Actions:
- Make sure:
- All discharges, notes, and high‑priority floor tasks are done or safely handed off.
- Page or find:
- Acute care surgery / trauma / ED triage, and say: “I am looking for OR time this afternoon and evening. If you get an emergent / urgent case, please loop me in.”
If you are constantly “just finishing notes” at 17:30, you will miss these.
Late Day and Evening: 15:00–22:00 – Capturing the Cases Others Abandon
Here is where you can quietly double your monthly case volume.

15:00–17:00 – The “Who Is Still Around?” Window
At this point you should be:
- Visible.
- Clearly not in a rush to leave.
- Obviously on top of your service.
Practical moves:
- Walk by:
- OR board.
- Charge nurse desk.
- Ask simple, non‑needy questions:
- “Any cases still unassigned for tonight?”
- “Any rooms that might run late and need an extra resident?”
If a borderline case is being debated for tonight vs. tomorrow and you say, “If the team wants to do it tonight, I am available to scrub,” you tip the scale sometimes.
17:00–20:00 – Prime Time for Extra Volume
This is where commitment is obvious. You are either the person:
- Still in scrubs and ready to go.
- Or the person in street clothes looking at the clock.
Your job during this block:
Stay in the OR zone.
- Do your floor or documentation work near the OR if possible.
- Answer pages quickly, but try not to disappear for 45 minutes.
Tell the right people you are willing.
- Charge nurse.
- Trauma / ACS senior.
- Any attending still operating.
- “If you need someone for any emergency case tonight, page me. I am here and free after [X].”
Be realistic about duty hours and safety.
- Do not wreck your next day’s first case by staying until 02:00 for a low‑yield case if you are first assist on a big case at 07:00.
- But within those limits, late‑day and evening cases are often the best technical reps.
20:00–22:00 – Shutdown and Setup Again
If you are not on call, this is the time to start closing your 24‑hour loop.
- Quick reflection:
- How many minutes were you in the OR today?
- Which moments cost you potential cases? (Messed up pre‑op? Slow notes? Missed ED consult?)
- Touch base with:
- Night team if relevant: “If anything goes emergently to the OR and you need help, you can wake me for a good case.” (Use this selectively. Your sleep is not infinite.)
Then, once again:
- Check tomorrow’s preliminary board.
- Repeat the 18:00–21:30 routine from above.
Consistency beats talent here.
Week-Level Structure: How This Routine Scales
If you run this 24‑hour routine 4–5 days per week:
| Approach | Avg Cases/Week | Typical OR Hours/Week |
|---|---|---|
| Passive (no routine) | 5–7 | 8–12 |
| Mildly proactive | 8–10 | 12–18 |
| Full 24-hr routine (above) | 12–18 | 18–30 |
These numbers are not fantasy. I have watched residents on busy ACS and trauma services do exactly this and log 600+ cases by graduation while their peers barely broke 400.
The key is not heroic bursts. It is the quiet, boring habits:
- Early board checks.
- Perfect pre‑ops.
- Making yourself the least stressful option when someone is assigning an extra case.
Two Subtle but Critical Principles
1. Reliability Buys You Cases
If you:
- Never disappear.
- Answer pages.
- Finish your floor work.
- Show up early and prepared.
Then attendings and staff will want you in their OR. They will go to bat for you when there is one resident slot and two claimants.
2. Explicit Ask > Hoping to Be Noticed
Hints do not work. People are too busy.
You have to say actual words:
- “I would like more OR volume. Please consider me for any add-on or uncovered cases.”
- “I am free from 1–3 p.m. and want to scrub. Who can I help?”
Done respectfully and repeatedly, this is not annoying. It is professional and ambitious.
FAQs
1. How do I balance floor work and chasing extra OR cases without burning out my co-residents?
You front‑load floor work aggressively: early rounds, decisive pages, and clear handoffs. Then you trade fairly. Offer to take someone’s admissions or notes for half a day in exchange for a case you want. If you consistently dump work on others just to scrub, people will block you. If you consistently help them offload scut in exchange for you taking hard cases, they will gladly send you to the OR.
2. What if my program culture does not support residents asking for more cases?
There is a difference between being pushy and being clear. You do not demand cases; you position yourself so that when something needs to be done, you are the obvious solution. You still show up early, fix pre‑op problems, know the patients cold, and let your chiefs and attendings know, quietly: “If there is an extra case and it does not disrupt the team’s work, I would like to scrub.” Over time, culture bends toward people who handle responsibility well.
Actionable next step today:
Set a 10‑minute timer right now, pull up tomorrow’s OR board, and identify one high‑yield case you want and two people (attending, chief, or charge nurse) you will proactively talk to before 07:00 tomorrow to make it more likely you are in that room.




















