It’s June 30th. Your MS3 year schedule just dropped. Surgery clerkship is in October–November, sandwiched between medicine and psych. You’ve heard the stories:
“Show up at 4:30 and maybe they’ll let you close.” “If you’re not aggressive, you’ll scrub three cases all month.” “You have to fight for cases with the other students.”
You’re not trying to survive this rotation. You want numbers. Real case volume. You want to actually do things in the OR, not just stand behind anesthesia and memorize the Krebs cycle.
This is your month-by-month, week-by-week plan to squeeze every case you can out of your surgery clerkship—without being annoying, burning out, or getting blacklisted by the OR staff.
3–4 Months Before Surgery: Quiet Prep, Systems Building
At this point you should not be memorizing Robbins or trying to learn every operation. That’s how people spin their wheels. You’re building two things now:
- A basic surgical vocabulary
- A system to track and chase cases
Focus on these targets:
Content prep (short, focused, non-miserable)
- Pick one resource for core surgery knowledge:
- Pestana
- DeVirgilio (if your school uses it)
- NMS or OnlineMedEd surgery videos
For the next 8–10 weeks:
- Do 2–4 vignettes or pages per day max.
- Focus on:
- Acute abdomen
- Trauma
- Post-op complications
- Common bread-and-butter (chole, appy, hernia, breast, colon)
You’re not trying to feel “ready.” You’re trying to not be completely useless in morning rounds.
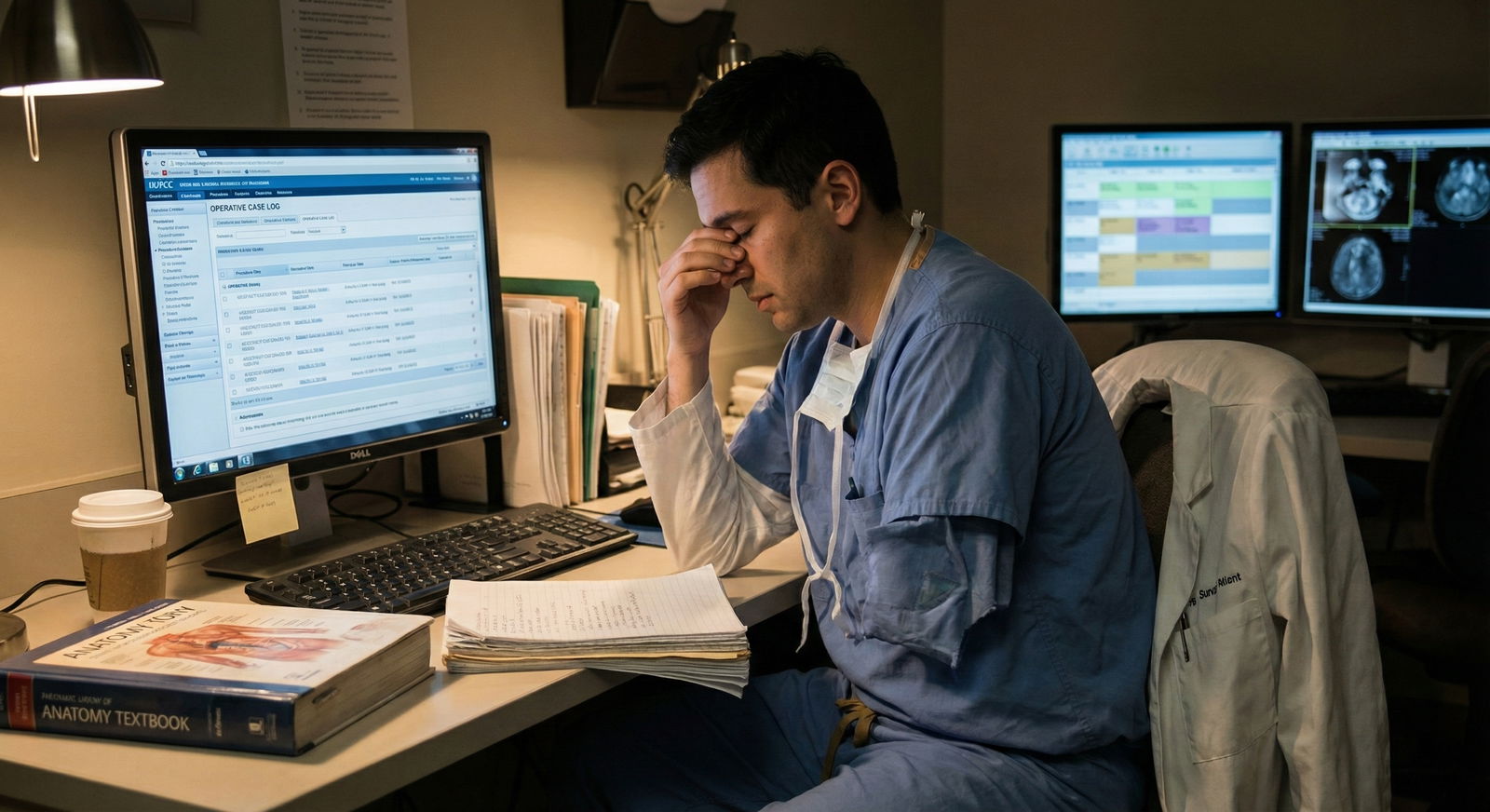
Build your tracking system
You want to hit the OR like a person who already thinks in cases.
Create:
- A simple spreadsheet or Notion table with:
- Date
- Service
- Attending
- Procedure
- Your role (observer, first assist, closing skin, etc.)
- Key steps you observed / performed
- One thing you learned
This will matter later when:
- You need numbers for your CV
- You want talking points for letters
- You need to quickly recall, “What’s the difference between a Lichtenstein and TEP?”
| Task Category | Specific Action |
|---|---|
| Knowledge | Choose 1 core surgery resource |
| Skills | Review sterile technique video |
| Logistics | Set up call room / locker essentials list |
| Tracking | Build case log spreadsheet |
| Mindset | Decide daily wake time and sleep cutoff |
Learn OR basics before anyone is watching
You should:
- Watch a 10–15 minute video on:
- Scrubbing, gowning, gloving
- Sterile field: what you never touch
- Ask a PGY2 you trust: “What annoys scrub techs the most about students?”
Write those things down and do the opposite.
1 Month Before: Schedule Intel and Service Strategy
Now you shift from passive prep to active planning.
At this point you should:
- Know your rotation dates and sites
- Have a rough target case volume in mind
Get real about numbers
Most students on a standard 8-week surgery clerkship end up around:

| Category | Value |
|---|---|
| Low | 20 |
| Average | 40 |
| High | 70 |
You are aiming for the high end: 60–80 cases seen/scrubbed over the block, with at least 20–30 where you actually do something more than retract.
Map the rotation
Email or ask:
Clerkship coordinator:
- Which services will I rotate on, and for how long? (General, trauma, vascular, colorectal, surg onc, etc.)
- Will I have clinic days or pure OR?
Senior students who just finished:
- “Which services have the highest OR volume?”
- “Where did students get to actually operate more—community or main campus?”
- “Who are the attendings that like to teach students in the OR?”
Make a simple priority list like:
- Trauma / acute care (high volume, many add-ons)
- General surgery (repeatable bread-and-butter)
- Vascular / colorectal (less volume but big learning)
- Specialty (ENT, plastics, etc. — often slower, but good if you’re interested)
This isn’t to avoid low-volume days. It’s to know where to lean in.
2 Weeks Before: Logistics and Expectations
At this point you should have answers to:
- What time does my team round?
- Where do I find the OR schedule?
- Where do I get scrubs and locker access?
Set up the mechanical stuff
Visit the hospital once:
- Find the locker room
- Find the scrub machine
- Find the OR board (physical board or EMR view)
- Figure out where the call room is
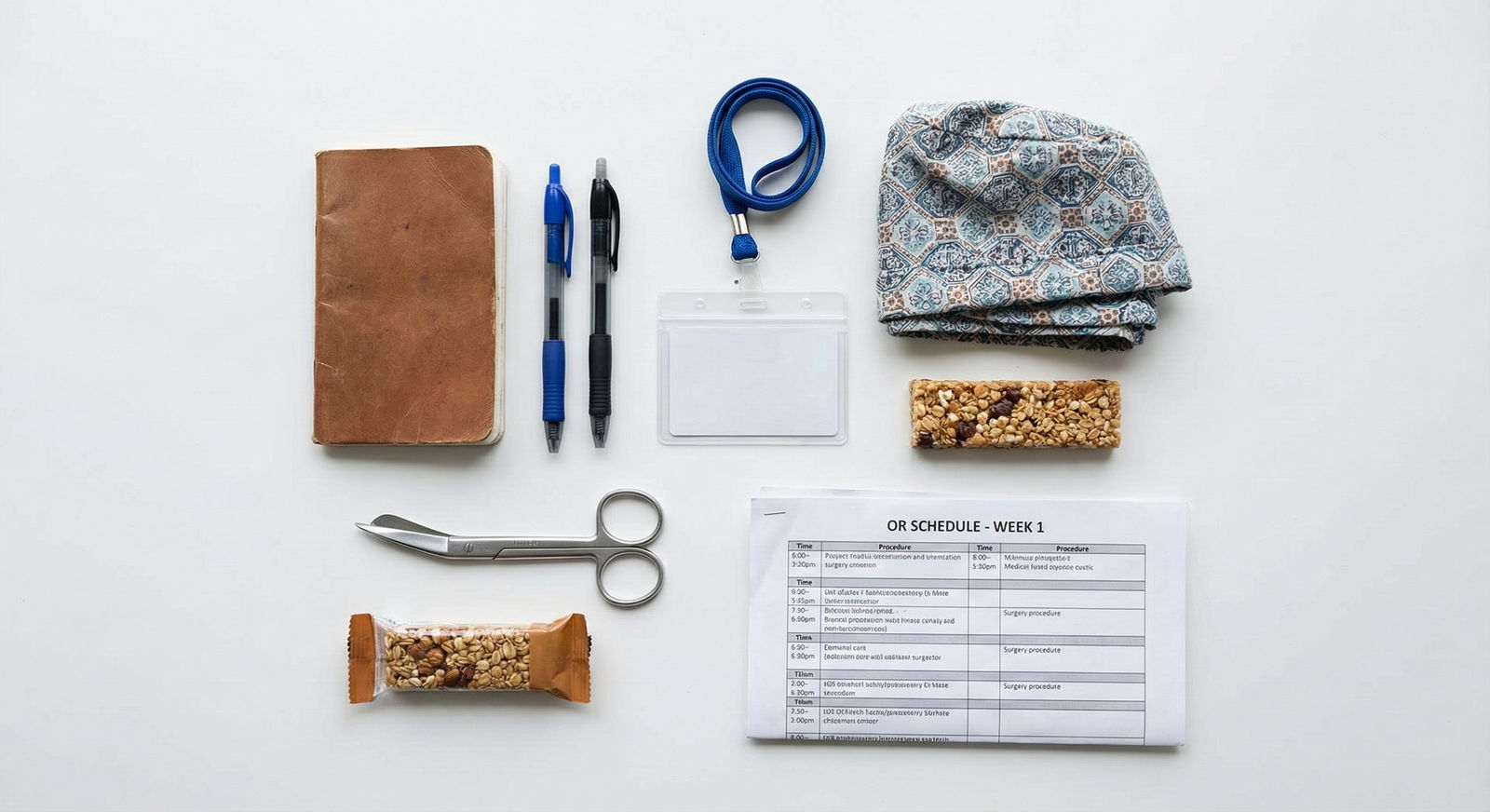
Assemble your “OR kit”:
- Small notebook or folded index cards
- 2 pens (one will disappear mid-case)
- Black fine-tip marker (for marking if you ever get to)
- Bandage scissors or trauma shears
- Snacks that live in your white coat / locker (nuts, granola, etc.)
Clarify expectations
Ask the clerkship director or residents:
- “What is the expected arrival time for students?”
- “How are students assigned to cases—by service, by attending, or do we self-assign?”
- “Is there a case log requirement?”
You don’t want to burn emotional energy on guessing basic norms. Get them in writing or in your notes.
Week 0 (Orientation Week): Position Yourself Early
At this point you should be moving from prep to strategy.
Day 1–2: Meet the power players
You want three sets of people on your side:
- Chief residents
- Mid-level residents (PGY2–3)
- OR charge nurse / board runner
Script that works with residents:
“I’m really hoping to maximize my OR time and get hands-on. Can you show me how the team usually decides which cases students scrub in on?”
Script with OR charge nurse:
“I’m the new med student on general surgery. I’d really like to help wherever there’s a case that needs an extra set of hands. Is there a way for me to check in with you about add-ons or open rooms during the day?”
Do this once. Not every morning. Don’t become the “needy student.”
Start your “case radar” habit
Every afternoon, do a 5-minute routine:
- Pull the next day’s OR schedule in the EMR
- Identify:
- Your team’s cases
- Any high-yield interesting cases (trauma, Whipple, transplant, big vascular)
- Write in your notebook:
- Patient name / MRN initials
- Procedure
- Attending
Then spend 3–5 minutes reading one short resource:
- UpToDate / pocket note / textbook section on:
- Indication
- Basic steps
- Major risks
Week 1: Learn the Game, Don’t Chase Every Case Yet
First week is reconnaissance. Your main goal:
Understand how your specific hospital manages OR flow.
At this point you should:
- Show up early enough to not be the last one
- Always know where your patients are and what they’re having done
- Watch how residents pick cases
Morning structure
Pre-round fast but not sloppy. Focus on:
- Vitals trends
- Overnight events
- Output (JP drains, Foley, NGT)
- Labs that matter: Hgb, WBC, lactate, Cr
After rounds, before you run to the OR:
- Ask your senior/PGY2:
“Which cases do you want me to scrub today? Any you’d prefer I prioritize?”
- Ask your senior/PGY2:
This single question is how you avoid stepping on toes and getting stuck in the world’s longest lap chole while a cool trauma is happening next door.
In the OR: do 3 things relentlessly
Be set up early
- Help move patient
- Place foley (if allowed)
- Help put on SCDs
- Introduce yourself to scrub and circulator quickly:
“Hi, I’m [Name], the med student. Where would you like me to stand and what can I do to help?”
Learn one reproducible maneuver per case
Examples:- How to use Army-Navy retractors correctly
- How to cut sutures the way your attending likes
- How to load a needle driver efficiently
-
- Do not trust yourself to “catch up this weekend”
- 30 cases later, they blur together shockingly fast
Week 2–3: Now You Start Pushing for Volume
You’ve shown reliability. Now you turn up the volume.
At this point you should:
- Know which services/attendings give you hands-on time
- Be trusted not to contaminate the field
- Feel comfortable asking for more
Daily pre-OR routine (10–15 minutes)
- Check tomorrow’s OR schedule again at lunch
- For each patient you might scrub:
- Read the H&P
- Know the indication: “Why is this patient getting this operation?”
- Be ready with:
- 2–3 complications
- Rough outline of the operation (“incision, exposure, critical step, reconstruction, closure”)
You’re not doing a PhD on each case. You’re arming yourself to look like you care.

| Category | Value |
|---|---|
| Rounds/Notes | 20 |
| In OR | 50 |
| Reading/Prep | 20 |
| Call/Admin | 10 |
How to get into more cases without being annoying
You will often have “dead time”:
- Patient delayed in PACU
- Attending stuck in clinic
- Case cancelled last minute
In those moments:
- Check the live OR board
- Look for:
- Trauma / acute care
- Any case with your service name on it
- Cases with your “friendly attendings”
Then either:
- Ask your senior:
“My case is delayed. Is it ok if I scrub into [Room 12] for the appy with Dr. X?”
Or if your team is fine with it and busy:
- Ask the OR charge nurse:
“My assigned case is delayed; can I help as an extra pair of hands in any general surgery room?”
If you do this once a day, you’ll accumulate significantly more cases than the student who just sits on their phone in the lounge.
Week 4: Mid-Block Adjustment and Targeting Gaps
By the midpoint of the rotation, sit down and review your case log.
At this point you should know:
- What you’ve seen a lot of
- What you’ve barely touched
- How often you’ve actually done something

Quick mid-rotation audit
Open your log and count:
- Total cases
- Number by category:
- General (chole, appy, hernia)
- Colorectal
- Vascular
- Trauma
- Breast / endocrine
- Other
Then ask:
- “Where are my obvious gaps?”
- “Where do I want more hands-on practice?”
For example:
- 14 choles, 0 hernias → you start asking to be on hernia days
- Tons of outpatient breast biopsies, no big cases → look for longer general/trauma OR days
Share that with your senior:
“I’ve seen a lot of lap choles but almost no hernias or trauma cases. Is there a good day or attending you’d recommend so I can fill those gaps?”
Seniors who like teaching will route you to the right rooms. Let them.
Second Month: Turn Volume into Skill
If your clerkship is 8 weeks, the second month is where you stop just “being present” and start deliberately practicing.
At this point you should:
- Be comfortable closing simple skin incisions
- Anticipate steps in basic cases
- Have a reputation as dependable
Week 5–6: Ask for specific roles
You’re no longer the anonymous extra set of hands. Start asking very targeted, low-friction questions:
Before the case:
- “Dr. X, is there a part of this case you’d like me to focus on today?”
- “If there’s a straightforward part to close, may I try it under your guidance?”
During the case (picked moments, not constant talking):
- “Would you like me to retract more cephalad?”
- “May I try placing the next staple / clip / stitch?”
After the case:
- “What’s one technical thing I can work on for next time?”
You’re proving you care about getting better, not just collecting names for your log.
Week 7–8: Maximize final impressions and last chances
End of the rotation, people are deciding:
- Do they want to write you a letter?
- Are you “a surgery person” or just passing through?
At this point you should:
- Know which attendings you clicked with
- Have at least one day per week where you stack multiple cases
Proactively ask to spend full days with your best surgeons:
- “I’ve really enjoyed working with you, Dr. Y. Would it be ok if I joined your OR list again on Thursday?”
Choose 1–2 operations as your “home base” of competence:
- For example, appendectomy and open inguinal hernia
- Know:
- Indications cold
- Steps in sequence
- Every complication you’d be embarrassed not to mention
When you see those on the schedule, you make a point to be in that room, early, and prepared.
Nights, Weekends, and Call: Hidden Case Volume
This is where you can quietly lap your classmates without ever bragging.

| Period | Event |
|---|---|
| Pre-Rotation - 3-4 months before | Light reading, build log |
| Pre-Rotation - 1 month before | Map services, logistics |
| First Month - Week 1 | Learn OR flow |
| First Month - Week 2-3 | Increase daily cases |
| First Month - Week 4 | Mid-rotation audit |
| Second Month - Week 5-6 | Focus on technical skills |
| Second Month - Week 7-8 | Maximize impressions, fill gaps |
Call strategy
If your rotation has call:
- Choose call nights that are high-yield:
- Trauma-heavy days
- Not the night before major shelf exam days
On call, you should:
- Live near the OR board and ED
- Tell the senior:
- “I’d really like to be in on any emergent cases tonight if possible—appy, laparoscopy, trauma, whatever comes.”
Trauma and acute care at 2 a.m.:
- Fewer competing learners
- Residents more likely to let you:
- Place trocars
- Close incisions
- Do small parts independently
Don’t be stupid about sleep, but don’t skip this either. Two good call nights can add 8–10 cases easily.
Weekends
If weekends are optional, be selective:
- Trade one dead weekday afternoon for a weekend morning full of cases
- Ask:
- “Is there a particular Saturday when there will be several add-on general surgery cases? I’d be willing to come in for more OR experience.”
You’re not trying to be a martyr. You’re making targeted trades: a little weekend time for concentrated case volume.
How to Not Burn Out While Doing All This
You can chase every case and be useless by week 3. Or you can be strategic.
At this point you should accept:
- You can’t scrub every case
- You don’t need to be in the OR 14 hours every single day to get strong volume
Set some personal rules:
Hard cutoff for “point of diminishing returns”:
- Example: If it’s after 8 p.m. and tomorrow is heavy rounds + long OR day, and there’s only a minor procedure left, you go home.
Minimum non-negotiables per day:
- 1 meaningful OR case or 1 high-value clinic experience
- 20–30 minutes of reading tied directly to patients you saw
- 6 hours of sleep whenever humanly possible

| Category | Target Cases per Week | Burnout Risk (0-10) |
|---|---|---|
| Week 1 | 6 | 2 |
| Week 2 | 8 | 3 |
| Week 3 | 10 | 5 |
| Week 4 | 10 | 6 |
| Week 5 | 10 | 7 |
| Week 6 | 10 | 7 |
| Week 7 | 8 | 6 |
| Week 8 | 8 | 5 |
After the Rotation: Lock In the Value of Your Cases
Most people finish surgery, pass the shelf, and move on. They leave a lot of value on the table.
At this point you should:
- Clean and finalize your case log
- Extract what’s useful for future applications
Within 1 week of finishing
Go through your log and:
- Flag your top 5–10 “story” cases:
- Interesting complication
- Great attending teaching moment
- The first time you really contributed
- Note who you might ask for letters:
- Attendings who saw you multiple times
- Residents who consistently pulled you into cases
- Flag your top 5–10 “story” cases:
Summarize your volume:
- “Over an 8-week clerkship, I scrubbed into ~70 operative cases across general, trauma, vascular, breast, and colorectal surgery, and performed parts of the operation including [closing incisions, placing trocars, basic suturing].”
This is the line that ends up in your CV, personal statement, or letters.

If Your Rotation Is Only 4 Weeks
Compress everything:
- Week 1: Learn flow + OR basics
- Week 2: Push for more cases, start logging aggressively
- Week 3: Mid-rotation audit + targeted case selection
- Week 4: Focus on technical skills and final impressions
Short rotation = no time for drifting. You need to be intentional from day 2.
Your Next Step Today
You don’t need to be on surgery right now to start this.
Do this today:
- Open a new document or spreadsheet.
- Title it: “Surgery Clerkship Case Log.”
- Add columns: Date, Service, Attending, Procedure, Your Role, Key Steps, One Lesson.
Then, write down 3 attendings or residents you’ve heard are good to work with on surgery at your school. Email or message one senior student and ask:
“Who are the best people for med students to work with on surgery if I want a lot of OR time?”
That’s your first move. The cases start from there.




















