One strong US clinical rotation can be stretched into three or four high-impact, specialty-specific letters of recommendation. Most IMGs waste that opportunity.
You are not going to pick up five different USCE blocks in your dream specialties at big-name hospitals. The system is stacked against you: limited spots, high fees, visa issues, and programs quietly prioritizing “their own” students. So if you have one solid USCE rotation, you need to treat it like a multi-use asset—not a one-off experience.
Let me break this down specifically: how to turn one rotation into multiple tailored LORs that actually move the needle for different specialties and program types.
1. The Core Concept: One Rotation, Many Versions
Everyone focuses on “getting more USCE.” That is not always realistic. For many IMGs, what they actually need is:
- One high-quality USCE block (preferably in the US, hands-on, with patient interaction), and
- The skill to extract multiple strategically targeted LORs from that single experience.
You are not forging anything. You are not lying. You are leveraging the fact that:
- You show different strengths to different attendings.
- Different attendings see you in different clinical contexts.
- The same faculty member can comment credibly on different strengths if you guide them well.
- ERAS does not require a separate rotation for each letter’s specialty label.
What you do is:
- Build deliberately different profiles with each attending (or with the same attending across different weeks/activities).
- Provide different letter packets (CV + personal statement + talking points) for each target specialty.
- Ask for differently focused letters, each emphasizing the angle you need: primary care, hospitalist, surgical, academic, etc.
That is the thesis. The rest of this article is how to execute that without being awkward, pushy, or transparent.
2. Choose the Right Rotation to “Split”
If you want to convert one USCE into multiple specialty-specific LORs, not all rotations are equal.
2.1 Best rotation types for multi-use LORs
The ideal rotation type has:
Cross-cutting clinical skills
Internal medicine, family medicine, inpatient sub-internships, and ICU rotations are perfect. Why? Because you touch:- Acute care
- Chronic disease management
- Procedures or at least procedural planning
- Interactions with multiple specialties (cards, nephro, pulm, surgery)
Multiple attendings or multidisciplinary staff
Rotations where you work with:- One core attending + multiple consultants
- Ward teams + specialist services (e.g., hospitalist + cardiology)
- Outpatient + inpatient mix
These naturally create different perspectives of you.
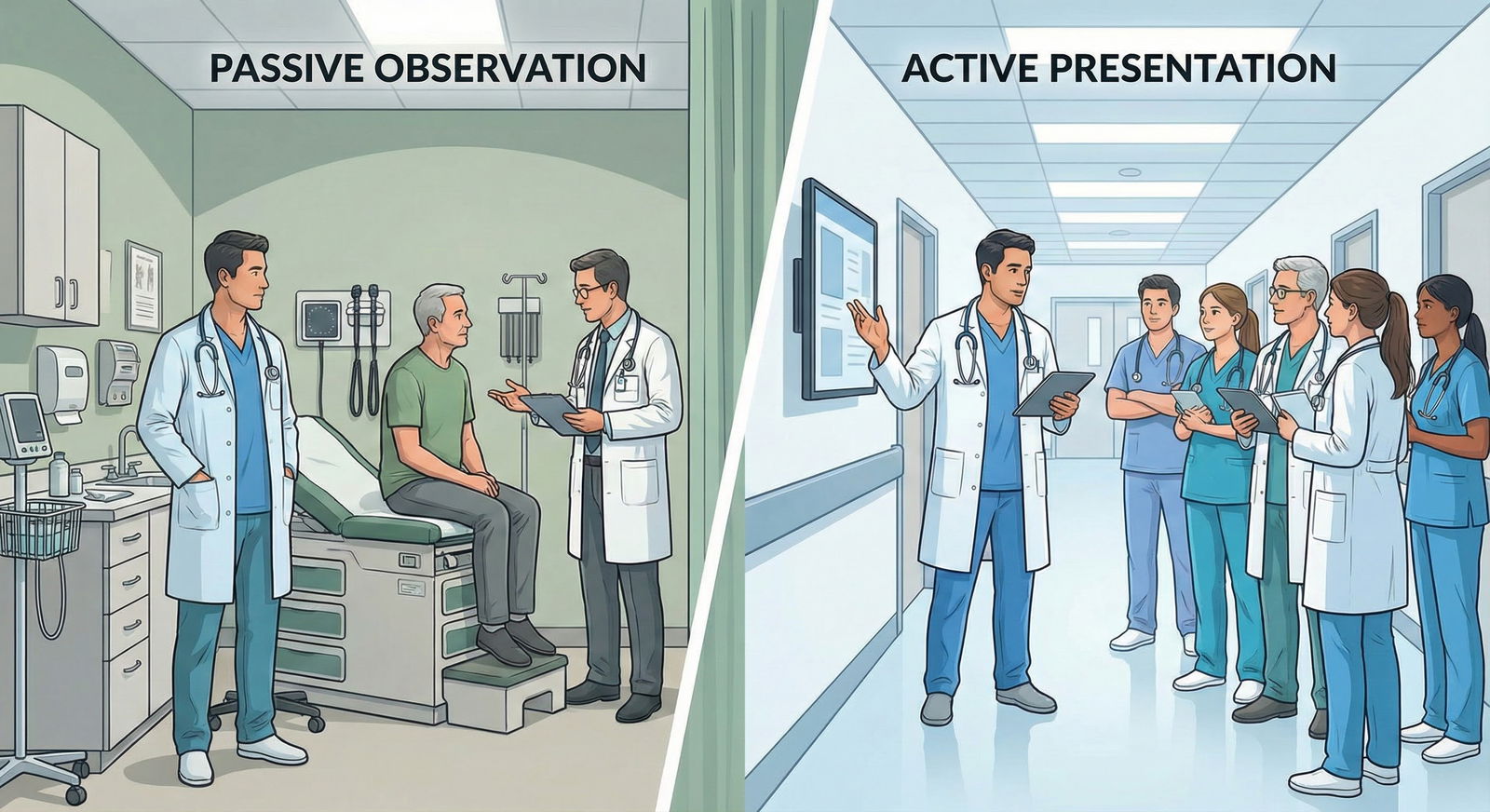
Hands-on structure
Observerships are much harder for this, but still possible. The more you:- Present cases
- Write notes (even if unofficial shadow charting)
- Call consults with supervision
- Participate in family meetings
…the more credible the letter gets.
2.2 Rotations that are harder to repurpose
Hyper-narrow subspecialty rotations (e.g., sleep medicine, allergy clinic only)
You can sometimes spin these toward IM/FM, but less easily toward surgery, EM, etc.Very short rotations (1 week “exposures”)
You cannot ask three different people for strong letters off a 5-day shadow. One decent generic LOR is the ceiling.
So if you have a choice between a 4-week internal medicine inpatient elective vs a 4-week limited specialty clinic as your only USCE, and you are unsure of exact specialty or want flexibility across IM/FM/Neuro/EM—pick the general one every time.
3. The Strategy: Creating Multiple “You”s on One Team
This is the part IMGs usually get wrong. They act exactly the same for every attending and hope for a “strong” generic letter.
What you actually want is targeted variation in how you show up.
3.1 Build different “tracks” within one rotation
Let’s say your 4-week USCE is in Internal Medicine at a mid-tier academic hospital. You are rotating with:
- Dr. K: hospitalist, known for meticulous notes and evidence-based medicine
- Dr. R: cardiologist consultant, high volume, fast-paced, procedure-oriented
- Dr. S: clinic preceptor, continuity/primary care focus
You can cultivate three different narratives:
Primary care / FM / outpatient IM narrative
With Dr. S (clinic):- Lean harder into communication, preventive care, social determinants, follow-up, continuity.
- Volunteer to call patients with results (under supervision).
- Be the person who remembers long-term medication histories and follow-up plans.
Inpatient IM / hospitalist / transitional year narrative
With Dr. K (wards):- Focus on differential diagnosis, inpatient management, progress notes, discharge planning.
- Speak the “hospitalist language”: productivity, safety, handoff quality, multi-morbidity management.
Acute / procedure-friendly / cross-specialty narrative
With Dr. R (cards):- Show interest in acute care, ICU, peri-op issues, procedures, ECG interpretation, stress testing.
- Ask high-yield questions that signal you see the tie to EM, anesthesia, or neuro (stroke/cardiac risk).
You are not faking interests. You are emphasizing different real aspects of your performance depending on the setting.
3.2 Be explicit about your interests—but segment them
You do not tell every attending “I am applying to twelve specialties.” That sounds scattered.
What you do instead:
- To Dr. S (clinic): “I am very interested in family medicine and primary-care–oriented internal medicine. I like continuity and long-term patient relationships.”
- To Dr. K (wards): “I am leaning toward internal medicine or a hospitalist pathway; I enjoy complex inpatient management.”
- To Dr. R (cards): “I am applying to internal medicine and also looking closely at cardiology-focused and hospitalist-heavy programs.”
You can be more transparent once trust is established, but early on you tailor your expressed interests to the context.
4. Timeline: Week-by-Week Execution
You have 4 weeks. You want 2–4 distinct LOR options out of it. That is actually feasible.

| Period | Event |
|---|---|
| Week 1 - Learn system & expectations | 1 |
| Week 1 - Identify key faculty | 1 |
| Week 2 - Differentiate roles with each attending | 2 |
| Week 2 - Ask for feedback | 2 |
| Week 3 - Signal specialty interests to specific attendings | 3 |
| Week 3 - Request letters from 1-2 strongest supporters | 3 |
| Week 4 - Request remaining letters | 4 |
| Week 4 - Send tailored packets CV, PS, bullets | 4 |
Week 1: Intelligence gathering
Your job:
- Figure out who actually observes you enough to later write something meaningful.
- Identify which attendings are:
- Detail-oriented and generous teachers
- Title-heavy (Program Director, Clerkship Director, Division Chief)
- Open to IMGs (you will feel this quickly—who engages vs ignores you)
You do not ask for any letters in week 1. You spend this week becoming:
Competent, low-maintenance, visibly hardworking, and a pleasant presence on the team.
Week 2: Deliberate differentiation
Now you start applying the “multiple yous” idea.
Examples:
- With the clinic preceptor: You prepare one or two brief patient-education handouts; you summarize chronic care guidelines.
- With the inpatient attending: You offer to draft detailed daily plans; you read guideline PDF and reference it on rounds.
- With the consultant: You show up early, pre-read upcoming consults, and prep relevant Qs about their specialty’s evidence base.
You also ask for formative feedback:
“Dr. K, I am hoping to apply for internal medicine and would like to become stronger this month. Are there 1 or 2 specific things I can improve on during this rotation?”
This does two things.
- Shows maturity.
- Signals you are serious about IM—planting the seed for a future IM-focused letter.
Week 3: Early asks for the strongest letters
By week 3, you typically know:
- Who likes your work.
- Who is willing to teach.
- Who has the authority or name that matters.
You can already secure 1–2 letter commitments this week.
Script (adjusted to specialty):
“Dr. K, I am applying to internal medicine residency and this has been my most meaningful US clinical experience. If you feel you know my work well enough, I would be very grateful if you could support my application with a letter that focuses on my inpatient IM performance.”
Notice:
- “If you feel you know my work well enough” gives them an out.
- “Focuses on my inpatient IM performance” quietly shapes the letter’s content.
For a clinic/primary-care letter:
“Dr. S, I am also targeting family medicine and primary-care–oriented programs. Would you feel comfortable writing a letter that highlights my work in clinic, especially around patient communication and continuity-minded care?”
Week 4: Additional tailored requests
During the final week:
- You confirm prior commitments.
- You approach any additional potential letter writers: E.g., a cardiologist for an acute-care–oriented letter that can serve you for IM, EM-leaning IM programs, or even neuro-heavy services.
You do not ask five people for five letters in a 4-week rotation. That looks unserious.
Three is usually the upper safe limit from a single 4-week block. Four only if the rotation truly had separate, sustained interactions (e.g., 2 weeks wards, 2 weeks ICU with different leaders).
5. How to “Specialty-Tune” Each Letter Without Being Obvious
The attending is not going to sit and reverse engineer your needs. You have to feed them material that biases what ends up in the letter.
This is where your supporting packet matters.
For each attending, you create a mini-packet assembled for the specific specialty angle you want.
5.1 Anatomy of a specialty-specific LOR packet
Each packet includes:
- Updated CV – same for all, but you can reorder sections slightly based on emphasis (e.g., primary-care projects near the top for FM).
- Targeted personal statement draft – the appropriate version for that specialty.
- One-page “Talking Points” document – this is the key trick.
That one-pager should have:
- 3–5 bullet points of specific things you did on their service.
- 2–3 traits you would like them to highlight (with context).
- A short sentence reminding them of your target specialty and how their letter will be used.
Example for Internal Medicine (inpatient-focused):
- “Led daily presentations of complex patients with multiple comorbidities; incorporated evidence from recent ACC/AHA heart failure guidelines into management plans.”
- “Volunteered to write comprehensive discharge summaries, focusing on medication reconciliation and follow-up clarity.”
- “Took initiative to discuss code status and goals of care in collaboration with the team, demonstrating maturity with difficult conversations.”
Traits to mention on that sheet:
- Clinical reasoning, thoroughness, reliability, maturity, team communication.
For a Family Medicine–oriented letter, same rotation but different one-pager:
- “Showed strong rapport with patients during continuity clinic visits; remembered social context and family details, which improved adherence.”
- “Created brief medication list summaries for patients with low health literacy and reviewed them using teach-back technique.”
- “Displayed consistent interest in preventive care, including screening schedules and vaccinations.”
Traits now:
- Communication, empathy, patient education, interest in community/primary care.
You are not demanding they copy-paste your language. You are giving them options. Most busy faculty will genuinely appreciate it.
6. Examples: Turning One IM USCE into Multiple Real Letters
Let me give you concrete combinations I have seen work.
Scenario A: Applying mainly to Internal Medicine, but also some Family Medicine
Rotation: 4-week inpatient IM with one half-day per week in clinic.
Potential LORs:
IM Inpatient Letter – “Core”
Writer: Hospitalist attending
Angle: Complex inpatient medicine, solid differential, reliable on call, good with handoffs.
Usage: Main letter for community and academic IM programs.Primary Care/Family Medicine Letter
Writer: Clinic preceptor
Angle: Communication, continuity mindset, preventive care, social determinants.
Usage: FM programs, IM primary-care–track programs.Flexible “Bridge” Letter (optional third)
Writer: Same hospitalist or a subspecialist with continuity exposure
Angle: Emphasizes both chronic disease management and patient-centeredness.
Usage: Can be used for either IM or FM depending on how he/she phrases specialty in intro.
Scenario B: Applying to Internal Medicine + a few EM or Anesthesia-prelim programs
Rotation: 4-week IM at a hospital with strong cardiology and ICU presence.
Potential LORs:
IM Core Letter
Focus: Bread-and-butter IM, team player, responsible, notes + work ethic.Acute Care / Procedures–Friendly Letter
Writer: Cardiology or ICU attending.
Focus: Rapid assessment, comfort with unstable patients, ECG interpretation, response during rapid responses or codes (as allowed), interest in procedure-related fields.
This letter can “read” as attractive to EM and anesthesia prelim programs even though writer is IM.Neutral Generic Academic Letter
Writer: Clerkship director or associate PD.
Focus: Professionalism, teachability, academic potential (for fellowship-minded IM apps).
Programs know you did not have twelve US electives. What matters is that each letter seems credible, specific, and aligned with the program’s culture.
7. Core vs Specialty-Specific: How Programs Actually Read These
Programs see hundreds of letters. They categorize them quickly:
- Is this a US letter?
- Is this from a core specialty (IM letter for IM, FM letter for FM)?
- Does the writer actually know the applicant or is this boilerplate?
- Is there anything in this letter that makes me picture this person functioning on my service?
| LOR Type | Source | Best Used For |
|---|---|---|
| Core Specialty LOR | Attending in target specialty | Main programs in chosen specialty |
| Primary Care–oriented LOR | Clinic/FM/PCP preceptor | FM, primary-care IM, community programs |
| Acute Care LOR | ICU/EM/cards/surgery consult | EM-leaning IM, prelims, anesthesia, neuro |
| Generic Academic LOR | PD, clerkship director | Academic programs, fellowship-leaning IM |
Your job with one rotation is to cover multiple boxes using different faculty, or different emphases from the same faculty.
Example: For an IMG applying to IM, what I want in the file:
- At least two letters clearly from IM attendings comfortable with internal medicine training culture.
- Optionally:
- One letter leaning toward primary care or outpatient for community-heavy programs, and
- One letter leaning toward acute/severity/procedures for academic or ICU-heavy programs.
You can produce these flavors from one robust rotation if you plan during the month, not after.
8. Handling Logistics: How to Actually Request and Use Multiple Letters
People get stuck in logistics—ERAS, letter assignment, asking multiple times. This is simpler than you think if you are organized.

| Category | Value |
|---|---|
| Pure IM | 3 |
| IM + FM | 4 |
| IM + Prelim/Anes | 4 |
| FM Focused | 3 |
Interpretation:
- Pure IM applicant: 3 strong IM-focused LORs.
- Mixed IM + FM: 2 IM-focused, 2 primary-care–leaning LORs total (you choose which to assign to which programs).
- IM + prelim/Anesthesia: 2 core IM, 1 acute-care, possibly 1 generic academic.
- FM-focused: 2 FM-oriented, 1 IM that can pass as primary-care–friendly.
8.1 Asking for different versions from the same attending
Yes, you can sometimes get two differently slanted letters from the same attending, but you must be subtle. The simplest form is:
- One attending writes one letter, but the content is broad enough to be used for multiple specialties.
- You then assign that letter either to IM or FM depending on how they mention your interests.
However, if you truly need two distinct angles from the same person (less common but occasionally done), the cleaner approach is:
“Dr. K, I am mainly applying for internal medicine, but I will also apply to a small number of family medicine programs. Would you be comfortable writing one letter that focuses on my inpatient internal medicine performance, and a second version that emphasizes my interest in longitudinal, primary-care–oriented work? I can provide separate brief talking points for each if helpful.”
Most will say no or prefer to write a single letter usable for both. Accept that.
Your main multi-letter leverage should be across different attendings, not forcing one person to rewrite your life twice.
8.2 Timing and uploading
You never carry letters yourself. You:
- Register the attending in ERAS (or CaRMS/NRMP equivalent).
- They upload directly.
- You then tag/assign letters to specific programs.
For specialty targeting:
- Assign the most inpatient IM–heavy letters to university IM programs, hospitalist tracks.
- Assign primary-care–heavy letters to FM programs, community IM with strong outpatient presence.
- Assign acute-care–tilted letters to EM-leaning prelims, anesthesia prelims, or IM programs at larger trauma/ICU centers.
9. Common Mistakes That Ruin This Strategy
Let me be blunt about the things I repeatedly see IMGs do that waste their only good USCE.
9.1 Asking at the last minute with no guidance
You vanish during week 4, then send a random email 2 months later: “Dear Dr. X, can you write a strong letter for my application?”
That is how you get:
- Generic “hardworking and pleasant” letters
- No specialty focus
- Minimal detail
You fix this by:
- Establishing intention in weeks 2–3
- Asking in person when possible
- Following up with a tailored packet immediately
9.2 Requesting too many letters from a single short exposure
If you spent:
- 2 weeks with Dr. A
- 2 half-days with Dr. B
Only Dr. A has any business writing a strong, content-rich letter. Dr. B might produce a weak “met this student twice” letter. Three weak letters do not equal one strong one.
Aim for 2–3 strong letters off a 4-week rotation with continuous or near-continuous exposure.
9.3 Being inconsistent in your narrative across letters
If one letter says:
- “She is deeply committed to a career in family medicine and has talked extensively about her interest in community primary care.”
And another says:
- “He has expressed a clear and long-standing intention to become an emergency physician.”
Programs will smell confusion. Or worse, dishonesty.
You can have adjacent interests (IM + FM, IM + cards). But do not manufacture extreme swings in your story across letters. Subtle re-weighting of the same core identity is what you want.
9.4 Ignoring titles and institutional value completely
A letter from a well-known academic attending at a mid-tier US university hospital will almost always outrank a glowing letter from a private clinic with no teaching affiliation.
If you have to prioritize:
- 1–2 letters from attendings with academic titles (PD, APD, Clerkship Director, Associate Professor)
- Then 1 from a community clinician who knows you extremely well and can tell richer stories
You still want specificity and person-level knowledge. But do not pretend all signatures carry equal weight.
10. Special Case: Observerships and Limited Hands-on Roles
Many IMGs are stuck with observerships where they cannot write in charts or formally present. It is harder, but not impossible, to execute this strategy.

What you can do:
- Become the unofficial historian: you know the full timeline of key patients, their meds, their labs.
- Offer to prepare mini literature reviews or 1-slide teaching presentations during downtime.
- Regularly ask: “Would it be helpful if I summarize this case for the team?” even if it is informal.
Then your talking points for letters will emphasize:
- Initiative in learning without direct responsibility
- Rapid understanding of the US system, EMR, and team structure
- Communication skills with patients even without independent orders
You may end up with fewer usable targeted letters from an observership (often 1–2). But you can still nudge them toward:
- Primary-care–leaning vs
- Inpatient/acute-care–leaning based on which aspect of your behavior you highlight.
11. Putting It Together: A Concrete Sample Plan
Let us build a real plan for a hypothetical IMG.
Profile:
- IMG, 2 years post-graduation, aiming for Internal Medicine but also applying to some Family Medicine.
- Has exactly one 4-week USCE IM inpatient rotation with half-day clinic.
Goal: 3–4 letters with specialty-adjusted impact.
Plan:
Week 1
- Identify 2 main attendings: Dr. K (inpatient), Dr. S (clinic).
- Possibly one subspecialist (cards or pulm) who sees you repeatedly.
Week 2
- Lean into hospital medicine identity with Dr. K (differentials, guidelines, notes).
- Lean into primary care identity with Dr. S (communication, patient education, continuity).
- Ask each for formative feedback.
Week 3
- Ask Dr. K: Letter for Internal Medicine with inpatient focus.
- Ask Dr. S: Letter for Family Medicine / primary-care–oriented programs.
- If a subspecialist has seen enough of you, ask for a third letter emphasizing acute care and complex medical decision-making.
Week 4
- Deliver two tailored packets: one IM-focused, one FM-focused.
- Add a “bridge” one-pager for the subspecialist: IM + acute care strengths.
- Confirm they understand your deadlines and ERAS upload process.
Application phase
- Assign 2 IM letters + 1 acute-care letter to IM programs.
- Assign 1 IM letter (still OK) + 1 primary-care letter + 1 optional acute-care or generic academic letter to FM programs.
That is how one rotation becomes 3 aligned, not contradictory, recommendation voices.
12. Final Takeaways
- One well-chosen USCE rotation can be engineered into multiple specialty-specific LORs if you differentiate how you show up to each attending and give them tailored talking points.
- Timing and structure matter: start building specialty narratives by week 2, ask for letters by weeks 3–4, and support your attendings with clear, concise packets (CV, PS, bullet points).
- Your letters must sound consistent with a coherent career story—different emphasis is fine, but wild specialty swings across letters make you look unfocused rather than versatile.





















