The COMLEX Level 3 OMM section is not creative. It recycles the same manipulation set‑ups over and over—and if you learn these patterns, you stop bleeding points.
Let me break this down specifically.
The Real Game: Pattern Recognition, Not Fancy Techniques
Level 3 OMM is not trying to test whether you can run a full structural exam like you are on an osteopathic sports medicine rotation. It is testing whether you can:
- Recognize a classic lesion pattern from a short description
- Pick the correct set‑up (body position + operator forces)
- Avoid dangerous or contraindicated techniques in clinical context
Think: “I have 45 seconds to scan for the OMM buzzwords and choose the setup that matches the cookbook pattern.”
To do that, you need to have the standardized set‑ups in your head cold. They keep reusing:
- The same sacral dysfunctions (especially torsions and unilateral lesions)
- The same rib inhalation/exhalation patterns
- The same lumbar NSR/FRSR/FRSL problems
- The same common thoracic Type II dysfunction setups
- The same cervical HVLA traps
- The same Chapman reflex locations and “what to treat first” logic
We will walk through those “high‑yield repeat offenders,” show you the likely question framing, and give you the exact setup language COMLEX wants.
Sacrum: The Favorite Toy of COMLEX Writers
If you screw up sacrum, you hemorrhage easy points. And they love sacrum at Level 3, especially when paired with pregnancy, low back pain, or postural complaints.
1. Sacral Torsions: Forward vs Backward
First, the patterns they recycle:
- Forward torsions:
- Left on Left (LOL)
- Right on Right (ROR)
- Backward torsions:
- Left on Right (LOR)
- Right on Left (ROL)
You must know two things cold:
- Which side is the axis? (the second letter: LOL → left axis)
- Forward vs backward → flexed vs extended sacrum
Now the setups.
Muscle Energy for Forward Sacral Torsions (LOL, ROR)
Core pattern: patient lies on the side of the dysfunction (side of the axis), face down (prone or Sims), with the torso rotated toward the table, and you use the legs to engage the barrier.
Example: Left on Left (LOL) torsion
- Axis: left
- Rotation: left
- They will often describe: L5 neutral, rotated left, sidebent right, or flexed pattern consistent with a forward torsion.
Classic ME setup:
- Patient: lies on left side (side of axis), face down (Sims position)
- Hips and knees flexed to about 90°
- You rotate the torso so that the chest faces the table (promoting forward torsion)
- Lower legs off the table to induce left rotation of the sacrum on left axis
- Have the patient push ankles toward the floor while you resist (or vice versa depending on textbook variant)
COMLEX angle: They will give you the diagnosis “L sacral torsion on L axis” or describe findings like:
- Deep sulcus on right
- Inferior/posterior ILA on left
- Positive seated flexion on right
And then ask you: “Which of the following set‑ups is most appropriate for muscle energy treatment?”
Correct answer language:
“Patient in left lateral Sims position, torso rotated toward the table, hips and knees flexed, legs dropped off the table to engage the barrier, patient instructed to push ankles toward the ceiling against resistance.”
Mechanism: You are using lumbar and pelvic musculature (primarily piriformis/gluteals) to correct the torsion.
Muscle Energy for Backward Sacral Torsions (LOR, ROL)
Core pattern: patient on side of axis, face up (supine lateral recumbent), extend to engage backward torsion, then use legs.
Example: Left on Right (LOR) torsion
- Axis: right
- Rotation: left (backward)
Classic ME setup:
- Patient: on right side (side of axis), face up (lateral recumbent)
- Flex hips and knees to 90°, then extend the lower leg (or move knees back) until you feel motion at lumbosacral junction
- Rotate shoulders toward the ceiling (backward torsion)
- Drop legs off table to barrier
- Patient pushes ankles toward floor or ceiling against resistance
COMLEX wording:
“Patient in right lateral recumbent position, facing up, with the physician rotating the torso posteriorly (toward the ceiling) and extending the lumbosacral junction while using the legs to engage the barrier.”
If you remember:
- Forward torsion → face down
- Backward torsion → face up
- Side of axis is on the table
…you will nail 80% of sacral torsion set‑up questions.
2. Unilateral Sacral Flexion/Extension
Another repeat offender.
Unilateral sacral flexion (e.g., left unilateral flexion):
Classic findings:
- Deep sulcus on left
- Inferior/posterior ILA on left
- Negative spring test (spring present)
- Positive seated flexion on left
Common ME setup (for left unilateral flexion):
- Patient prone
- Physician stands on left
- Palpate sacral base and ILA
- Apply downward pressure on the left ILA to promote extension
- During inhalation, maintain pressure
- During exhalation, follow motion but maintain extension bias
COMLEX version:
“Patient is prone, physician contacts the ipsilateral ILA and applies an anterior and cephalad force while the patient breathes; physician emphasizes force during inhalation to improve sacral extension.”
Unilateral extension is the mirror:
Unilateral sacral extension (e.g., left unilateral extension):
- Shallow sulcus on left
- Superior/anterior ILA on left
- Positive spring test (poor springing)
Setup:
- Patient prone
- Physician stands on left
- Contact left sacral base
- Apply anterior and caudad force at base
- Emphasize during exhalation (improving flexion)
Key pattern COMLEX loves:
- Extension lesion → engage base
- Flexion lesion → engage ILA
- Exhalation emphasizes flexion, inhalation emphasizes extension
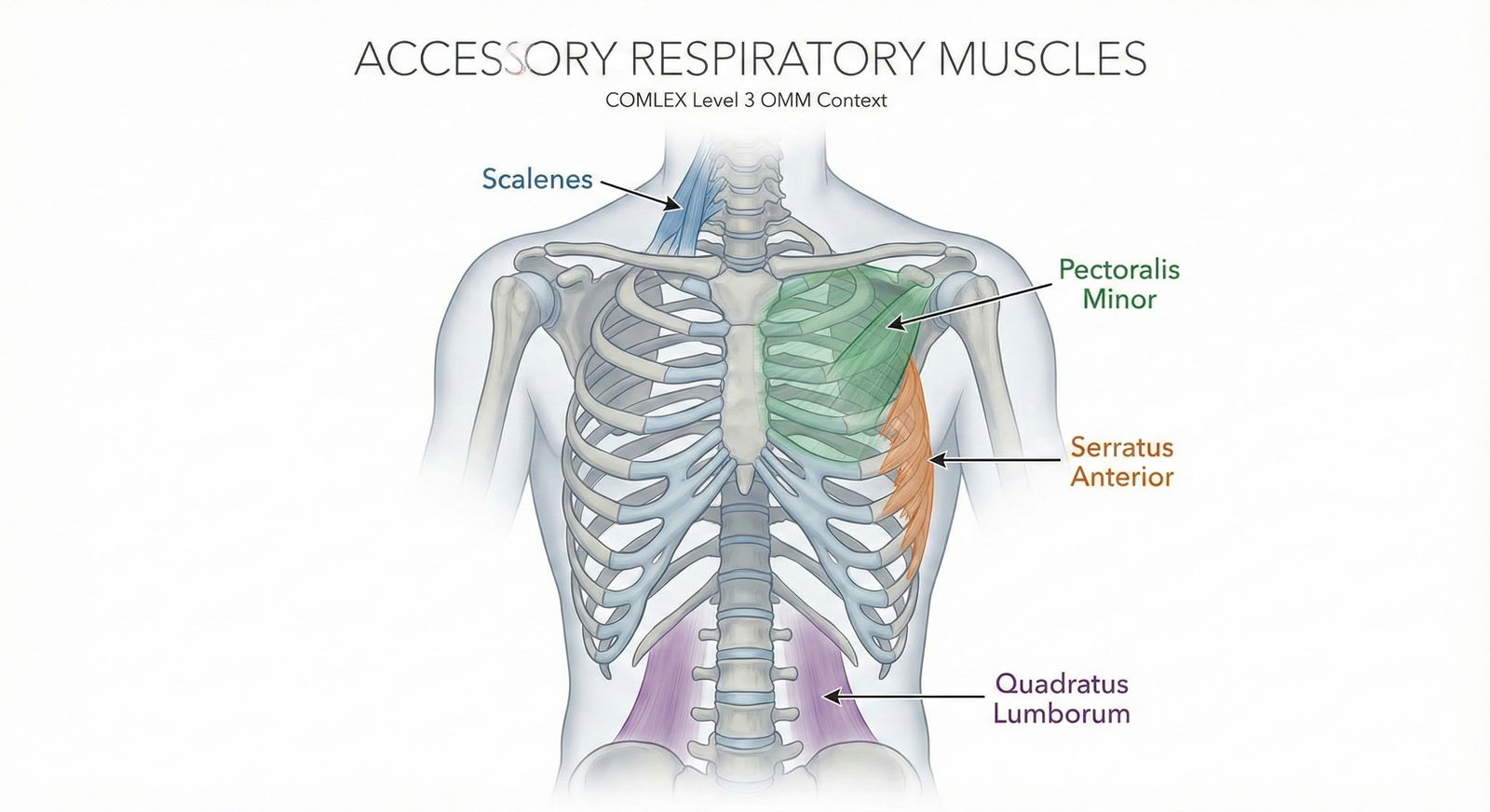
Ribs: The Same Inhalation/Exhalation Patterns on Repeat
If you get rib mechanics plus OMM, they are fishing for:
- Pump‑handle (ribs 1–5) vs bucket‑handle (ribs 6–10)
- Inhalation dysfunction (“key rib is lowest”)
- Exhalation dysfunction (“key rib is highest”)
- Correct muscle energy set‑up using proper muscles
1. Muscles They Keep Testing
Memorize this table. It gets reused constantly.
| Rib(s) | Dysfunction Focus | Primary Muscle Used |
|---|---|---|
| 1 | Exhalation | Anterior & Middle Scalene |
| 2 | Exhalation | Posterior Scalene |
| 3–5 | Exhalation | Pectoralis Minor |
| 6–9 | Exhalation | Serratus Anterior |
| 10–12 | Exhalation | Latissimus Dorsi / Quadratus Lumborum |
Level 3 pattern:
They give you an exhalation dysfunction of a group of ribs and ask:
“Which patient positioning and muscle contraction is most appropriate?”
Example: “Exhalation dysfunction of ribs 3–5 on the right.”
Correct set‑up:
- Treat key rib: highest rib stuck down (rib 3)
- Use pectoralis minor
- Patient supine, physician at side of table
- Grasp rib 3 at angle, flex patient’s arm and abduct to engage pec minor, ask patient to push elbow toward the ceiling (or down) against resistance while you hold the rib at its exhalation barrier.
2. Inhalation vs Exhalation Key Rib Logic
They are not going to make you diagnose every rib. They drop the diagnosis or give you group findings.
Quick rules:
- Inhalation dysfunction (“stuck up”): key rib is the lowest rib in the group
- Exhalation dysfunction (“stuck down”): key rib is the highest rib in the group
COMLEX phrasing:
“Group of ribs 3–7 on the left with an inhalation dysfunction. Which rib should be the focus of treatment?”
Answer: rib 7 (lowest, inhalation).
For exhalation 3–7, focus rib 3 (highest).
They recycle this logic across multiple forms.
Lumbar and Thoracic HVLA/ME: The Same Cookbook Phrases
You are not doing a hands‑on OMM practical. You are picking between 4–5 options like:
- “Physician stands on the right, patient in left lateral recumbent, rotate shoulders posteriorly, flex hips to L3, then apply an anterior thrust through the pelvis.”
This is just pure pattern matching.
1. Type II (FRSR/FRSL) Lumbar Dysfunction – Lateral Recumbent HVLA
Example diagnosis: L3 FRRSR (L3 flexed, rotated right, sidebent right).
Core concept:
- Sidebending toward the side on which the patient lies
- Rotation opposite the side the patient faces
Standard HVLA rule: “SIDEBEND them toward you, ROTATE them away from you.”
For L3 FRRSR:
- Rotation right, sidebent right
- You want to position patient to engage barrier in extension, sidebend left, rotate left.
Common setup:
- Patient: right lateral recumbent or left, depending on style, but COMLEX tends to follow Fryette patterns where:
- For L3 FRRSR, you often place patient on the right side (easy to sidebend left)
- Flex hips and knees until you localize at L3
- Rotate shoulders toward the ceiling (producing left rotation relative to pelvis)
- Drop patient’s upper leg forward over the table edge or into your lap, with your forearm stabilizing pelvis
- Apply a quick, small amplitude anterior thrust to the pelvis (toward table)
COMLEX answer often sounds like:
“Patient in right lateral recumbent position, physician standing facing the patient, flexes knees to localize at L3, rotates patient’s shoulders posteriorly, then delivers a quick anterior thrust to the pelvis to correct L3 FRS right.”
You do not need to be an OMM wizard. You just need to link:
- Flexed lesion → add extension
- Rotated right → rotate left
- Sidebent right → sidebend left
- Lateral recumbent → thrust through pelvis
2. Type I (NSRRL etc.) Thoracic/Lumbar Muscle Energy
Example diagnosis: T5–T9 NSRRL (neutral, sidebent right, rotated left).
Group curve. You treat with:
- Patient sitting or prone
- You sidebend toward the restricted barrier and rotate opposite
- Patient resists your positioning
Classic muscle energy wording:
“Patient seated, physician stands on right, places left hand over the patient’s head and neck, right hand monitoring over apex of group curve, sidebends the trunk left and rotates right to barrier, and instructs the patient to sidebend right against resistance.”
COMLEX loves the “patient seated, physician behind patient, physician sidebends opposite the side of sidebending, rotates opposite of dysfunction” pattern.
Cervical HVLA: The “Don’t Kill the Patient” Section
Level 3 is obsessed with safety. If they give you:
- RA,
- Down syndrome,
- Trauma,
- Vertebral artery issues,
- Severe OA, or
- Rheumatoid pannus at C1–C2
…and ask for treatment, the correct answer is almost never cervical HVLA. It points you to:
- Indirect
- Articulatory
- Soft tissue
- Muscle energy without high‑velocity thrust
1. Typical Type II Lower Cervical (C3–C7) HVLA Pattern
Example: C5 FRSR (flexed, rotated right, sidebent right).
Classic HVLA setup:
- Patient: supine
- Physician: seated at head of table
- Monitoring: contact articular pillar of C5 with index finger
- Position:
- Extend to the level of C5
- Sidebend left (opposite of lesion)
- Rotate left
- Thrust: small amplitude, high velocity in the rotational or sidebending arc at the barrier
COMLEX answer phrases:
“Patient supine with the head and neck extended, sidebent left and rotated left to localize at C5, with a short rotational thrust toward the left.”
You do not need to memorize every variety. Just know:
- Diagnosis FRS right → position into E, SL, RL
- Diagnosis ERS left → position into F, SR, RR
And again: RA or atlantoaxial instability? DO NOT choose HVLA.
Chapman Points: Tiny Nasty Favorites
These are a pain to memorize in school, but COMLEX reuses a small subset.
1. Classic Locations They Love
They will give you vague symptoms like “IBS,” “ulcer,” “pneumonia,” “otitis media,” and ask for:
- The anterior Chapman point
- OR which organ is associated with a given point
Core recurring ones:
- Middle ear: superior anterior aspect of clavicle, just lateral to where it crosses rib 1
- Sinuses: upper edge of rib 2, medial to midclavicular line
- Lungs (upper): 3rd ICS, near sternum
- Lungs (lower): 4th ICS, near sternum
- Heart: 2nd ICS, near sternum
- Stomach (acid): left 5th ICS, midclavicular
- Liver: right 5th and 6th ICS, midclavicular
- Gallbladder: right 6th ICS, midclavicular
- Appendix: tip of 12th rib on the right
- Colon: IT band (mirrors colon segments)

| Category | Value |
|---|---|
| Appendix | 10 |
| Lungs | 8 |
| Heart | 6 |
| Stomach | 7 |
| Liver/Gallbladder | 7 |
Numbers are illustrative, but the point is: they recycle these over more obscure ones.
2. How They Frame Questions
Two recurrent formats:
“Which of the following locations is most consistent with a Chapman's reflex for the appendix?”
- Correct: tip of the 12th rib on the right.
- Watch for distractors at McBurney’s point (that is tenderness, not Chapman).
“Treatment of which structure should be prioritized to address this patient’s referred pain?”
- You recognize the Chapman point → answer the organ.
The actual treatment description (gentle rotary pressure over the point for 20–30 seconds) may show up as a secondary step.
Rib Raising, Sympathetics, and Viscerosomatic Logic
Level 3 wants you to tie OMM to patient management. Rib raising questions are often buried in vignettes about:
- Post‑op ileus
- Hypertension and anxiety
- COPD or asthma exacerbations
- GERD, IBS, or dyspepsia
1. Rib Raising → Sympathetic Normalization
High‑yield association:
- T1–T4: head/neck, heart, lungs
- T5–T9: upper GI
- T10–L2: lower GI, GU, reproductive
Rib raising at a certain spinal level:
- Early, brief stimulation → can enhance sympathetic tone
- Sustained, gentle → tends to normalize/decrease hyperactivity
COMLEX uses that to test:
What OMM to support post‑op ileus?
- Gentle thoracolumbar soft tissue and rib raising to normalize T10–L2 sympathetics, plus stimulate sacral parasympathetics (sacral rocking).
What OMM for asthma exacerbation?
- Thoracic inlet, rib raising T1–T7 to optimize sympathetics and mechanics, treat diaphragmatic restrictions.
They will sneak OMM into management answer sets where you also must choose bronchodilators, steroids, etc. Choose both appropriate medical treatment and the logical OMM approach.
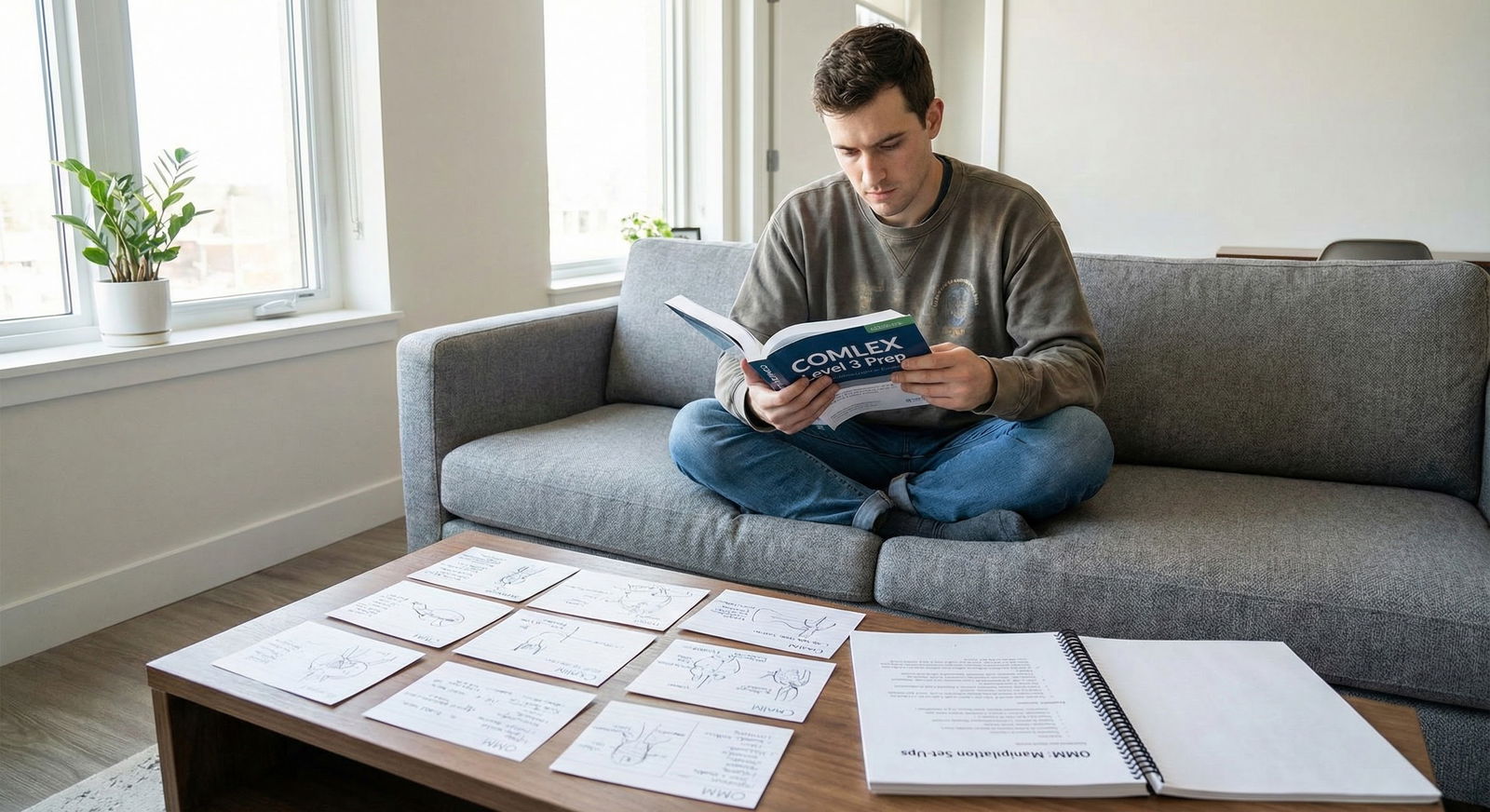
How to Practice These Patterns Efficiently
You do not need a month of OMM bootcamp for Level 3. You need targeted pattern drilling.

| Step | Description |
|---|---|
| Step 1 | Identify High-Yield Patterns |
| Step 2 | Review Set-Up Diagrams |
| Step 3 | Do 20-30 Pattern-Based Questions |
| Step 4 | Write Your Own 1-Line Set-Up Scripts |
| Step 5 | Rapid Daily 10-Min Flash Review |
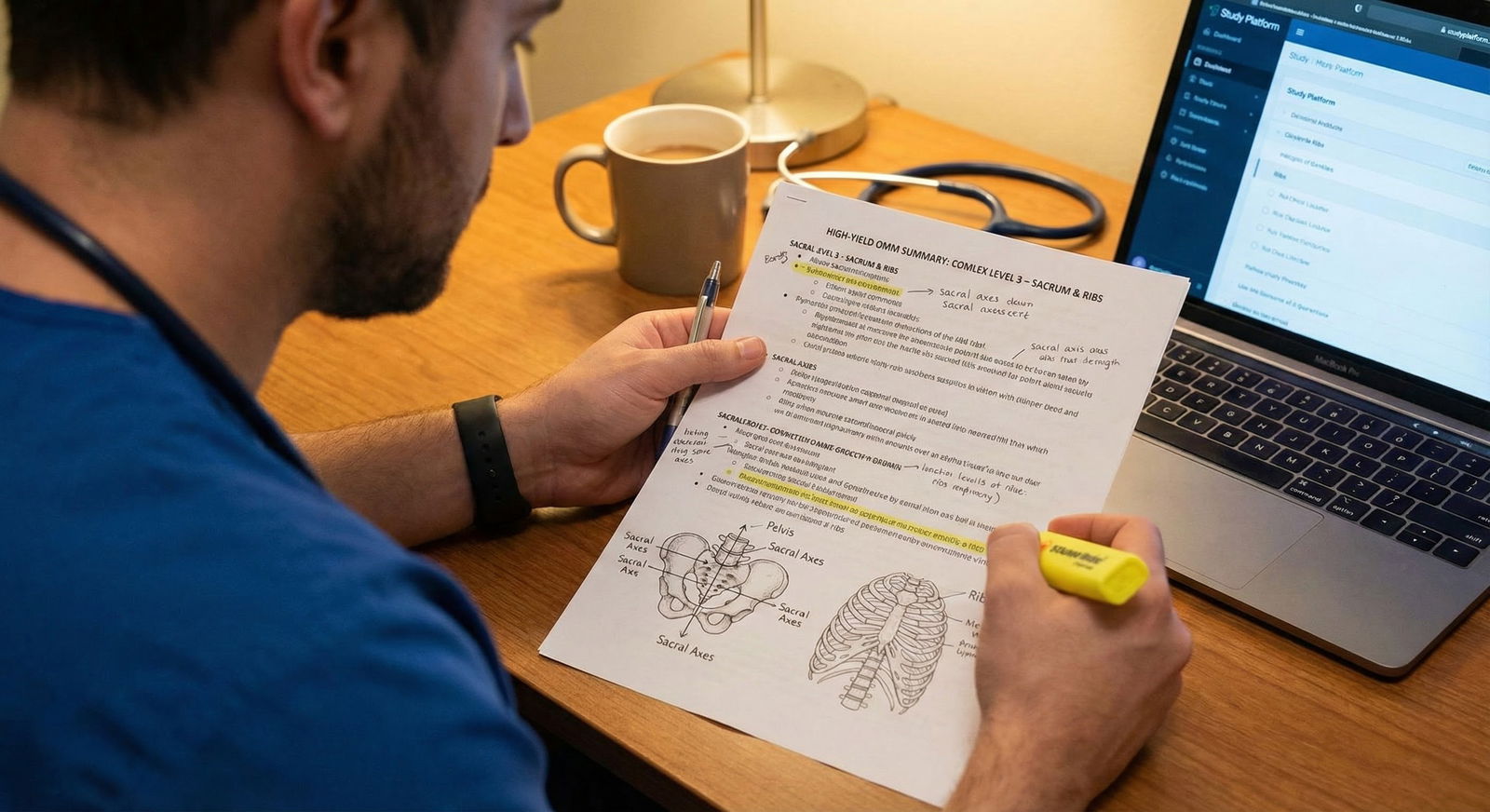
1. Build a One‑Page “Set‑Up Script Sheet”
For each of these categories:
- Sacral torsions (forward/backward)
- Unilateral sacral flexion/extension
- Rib inhalation/exhalation with muscle energy muscles
- Thoracic and lumbar FRS/ERS HVLA
- Cervical HVLA contraindications and patterns
- 10–12 key Chapman points
Write 1–2 line plain English descriptions of the set‑up.
Example:
- “LOL: patient on left side, face down, flex hips and rotate torso into table, drop legs off table, ME using legs.”
- “LOR: patient on right side, face up, extend lumbosacral, rotate torso posterior, drop legs, ME.”
- “Ribs 3–5 exhalation: treat rib 3 using pec minor, supine, push elbow against resistance.”
Put this on a single sheet. That sheet is your Level 3 OMM lifeline.
2. Practice With Purpose, Not Volume
You do not need 500 OMM questions. You need 30–50 that show:
- Set‑up recognition
- Contraindications
- Chapman logic
- Autonomic segments

| Category | Value |
|---|---|
| Pattern Review | 40 |
| Question Practice | 35 |
| Diagram Sketching | 15 |
| Flashcards | 10 |
Focus 1–2 weeks before your test, 15–20 minutes per day:
- Day 1–3: Sacrum + lumbar set‑ups
- Day 4–6: Ribs + thoracic + Chapman points
- Day 7–10: Mixed review with questions
Consistent short bursts beat a single mega‑cram session.
Clinical Vignettes: How These Actually Show Up
A few quick “this is exactly what they like to do” scenarios.
Scenario 1: Post‑partum Low Back Pain
32‑year‑old G1P1 woman, 2 days post‑vaginal delivery, sacral tenderness, positive seated flexion on right, deep sulcus on right, inferior ILA on left, spring test negative. Diagnosis: Left on Left forward sacral torsion.
Question: “Which of the following best describes the patient and physician positioning for appropriate OMT?”
Correct: description of LOL forward torsion ME (patient left side, face down, Sims, flex hips, rotate torso anteriorly, legs off table, patient pushes ankles up or down against resistance).
Scenario 2: COPD Exacerbation
65‑year‑old with COPD exacerbation admitted for hypoxia. You give appropriate meds. They ask: “Which OMM technique best improves thoracic cage mechanics and autonomic tone?”
Answer: Rib raising, balanced ligamentous tension for thoracic inlet, diaphragmatic release at appropriate levels (T1–T7, diaphragm).
They might offer nonsense like “HVLA at C1–C2” or “muscle energy to pubic symphysis.” Ignore the noise.
Scenario 3: Right‑Sided Chest Pain with Exhalation Dysfunction
45‑year‑old with right‑sided chest pain after coughing. Exhalation dysfunction ribs 3–5 on right.
Question: “Which muscle is most appropriate to engage during ME?”
Answer: Pectoralis minor.
Visual Memory Tricks That Actually Help
You are tired and busy. Use visual anchors.
1. Sacrum Picture in Your Head
Imagine:
- Forward torsion → patient hugging the table, face down, curled around axis.
- Backward torsion → patient looking at the ceiling, more extended.
Forward → face down. Backward → face up.
Axis side is on the table.
2. Ribs as a Ladder with Muscles
Picture a ladder:
- Step 1: scalenes
- Step 2: posterior scalene
- Steps 3–5: pec minor
- Steps 6–9: serratus anterior
- Steps 10–12: lats/QL
You climb from neck (scalenes) to lateral chest wall (serratus) to posterior abdomen (QL).
3. Chapman Points: Belt plus ICS
Think:
- ICS (2–6) near sternum for cardio‑pulm and upper GI.
- Tip of 12th rib → appendix.
- IT band → colon map.
You do not need every single point. You need the common clinical ones they reuse.
Putting It All Together the Week Before the Exam
If you are one week out:
- Print or write your 1‑page OMM setup sheet.
- Do 10–15 mixed OMM questions daily.
- Spend 10 minutes reading that sheet out loud once a day.

| Task | Details |
|---|---|
| Patterns: Sacrum & Lumbar | a1, 2026-01-01, 2d |
| Patterns: Ribs & Thoracic | a2, 2026-01-03, 2d |
| Patterns: Cervical & Safety | a3, 2026-01-05, 1d |
| Patterns: Chapman & Autonomics | a4, 2026-01-06, 1d |
| Patterns: Mixed Review | a5, 2026-01-07, 1d |
That is it. You are not trying to become an OMM fellow. You are trying to avoid missing the same recycled patterns 10 times.
FAQs
1. How much OMM is actually on COMLEX Level 3?
OMM is not the majority of the exam, but it is easily enough to swing your score if you ignore it. You will see OMM both as standalone technique questions and embedded in clinical vignettes (pain, autonomics, postop care, pregnancy). You can expect a noticeable chunk of questions where OMM is either the primary or a secondary component of the answer.
2. If I am weak in hands‑on skills, can I still get these questions right?
Yes. Level 3 is testing cognitive recognition, not your ability to perform a perfect HVLA thrust. If you memorize the standard set‑up phrases and patterns (sacral torsions, rib ME, lumbar/thoracic FRS/ERS setups, Chapman points), you can do very well without being manually gifted.
3. Should I avoid choosing HVLA answers because of safety concerns?
No. Choose HVLA when:
- There are no red‑flag contraindications (RA, Down syndrome, carotid or vertebral artery disease, severe osteoporosis, acute trauma), and
- The question clearly diagnoses a Type II dysfunction and asks for the most direct corrective technique.
They love using HVLA as the “most efficient” or “definitive” option when the patient is otherwise healthy.
4. Are the exact hand positions (e.g., which finger on which spinous process) tested in detail?
Rarely. Level 3 is more interested in global positioning (patient supine vs lateral, face up vs face down, side of axis, muscles used, flexion vs extension) than whether you remember index vs middle finger. If you can recognize the correct body position and direction of force, you will get the point even if hand‑position details differ slightly from your school’s style.
5. If I only have 2–3 days for OMM review, what should I prioritize?
In this order:
- Sacrum (torsions + unilateral lesions)
- Rib inhalation/exhalation ME patterns + muscles
- Lumbar/thoracic Type II HVLA setups
- 10–12 key Chapman points and autonomic segments
That short list captures the most frequently reused setups and patterns on COMLEX Level 3.
Key points:
- COMLEX Level 3 OMM reuses a small number of standardized set‑ups—learn those, and you win.
- Sacrum, ribs, Type II spine lesions, Chapman points, and autonomic segments are the core repeat offenders.
- You do not need more time; you need focused pattern drilling and a one‑page setup sheet you actually review.






















