
Most people fail CCS time management long before they fail medical knowledge.
You can know the guideline cold and still bleed points if you do the right thing 20 simulated minutes too late. Step 3 CCS is less “What is the diagnosis?” and more “Did you act like a real doctor who understands urgency and sequencing?”
Let me break this down specifically. We will focus on acute scenarios and exactly what to order, when to order it, and in what environment. This is what actually moves your CCS score.
The Core CCS Mindset: Time, Location, and Stabilization
Before we get into individual emergencies, you need the framework the exam is secretly grading.
1. Time is a second scoring dimension
CCS cases score you on two parallel tracks:
- Did you order the right things?
- How quickly did you order them relative to clinical urgency?
You can:
- Lose huge points for “right order, wrong time”
- Lose points for managing outpatient what should be in the ICU
- Lose points for not moving the clock when appropriate (e.g., just sitting in the ED for 8 hours without disposition)

| Category | Value |
|---|---|
| Timing of critical actions | 45 |
| Completeness of workup | 35 |
| Disposition/location choices | 20 |
Interpret that as a reminder: timing of critical moves matters more than whether you remembered every last vitamin.
2. Location is part of management
On CCS, “where” you place the patient is as important as “what” you order.
Very rough rule:
- Unstable → ICU
- Potentially unstable / needing frequent reassessment → ED or step-down / monitored bed
- Stable, no red flags → ward or clinic
Admit/disposition is not an afterthought. It is part of the treatment plan.
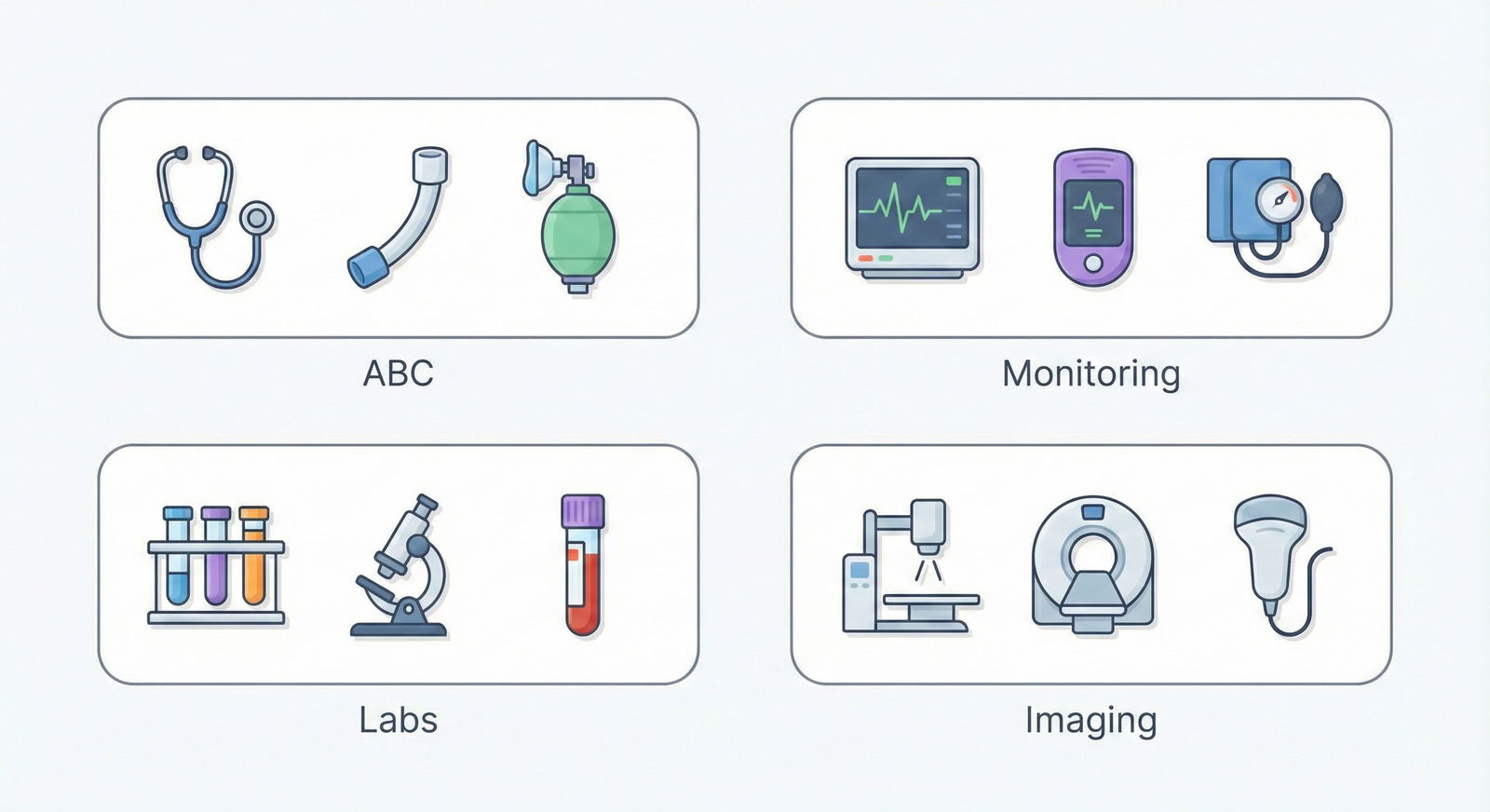
3. First moves: Airway–Breathing–Circulation (ABC) plus monitors
For any acute or crashing case, your reflex should be:
Immediate orders (often all at once):
- Oxygen (nasal cannula or non-rebreather depending on distress)
- IV access (two large-bore peripheral IVs)
- Cardiac monitor
- Pulse oximetry
- Blood pressure monitoring (and frequent vitals)
- EKG
- Fingerstick glucose (POC)
You can “batch” these orders. The interface allows multiple simultaneous orders. Use that.
High-Yield Global Order Sets for Acute CCS Cases
You will not have time during the exam to reinvent order bundles. Build a mental library.
Think of these as “macro” sets you trigger when you recognize the pattern.
Universal Acute Stabilization Orders (for almost any ED/ICU acute case)
If patient looks sick, you should almost certainly fire:
- Location: “Emergency Department” or “ICU” depending on vitals.
- ABC + Monitoring:
- Oxygen
- Cardiac monitor
- Pulse oximetry
- Continuous BP / vitals q1h or q15min if crashing
- IV access (2 large-bore)
- Labs:
- CBC with diff
- BMP or CMP
- Serum glucose
- Troponin (if any chest pain, SOB, or unclear picture in adult)
- Coags (PT/INR, aPTT)
- Type and screen (any possibility of surgery/bleeding)
- ABG if respiratory compromise or metabolic acidosis likely
- Others:
- EKG
- CXR (acute chest, dyspnea, fever, or unclear)
You will not get penalized for reasonable “over-ordering” in acute scenarios. You will get penalized for under-ordering or for missing time-critical stuff.
Acute Coronary Syndrome (ACS): Orders and Timing
Acute chest pain is bread-and-butter CCS. The exam expects automation-level speed here.
Stepwise approach: what to order and when
Initial 0–5 real-time minutes:
- Set location: Emergency Department.
- ABC + monitors (oxygen, IV, cardiac monitor, pulse ox, EKG).
- Focused medications (if not hypotensive, not allergic):
- Aspirin: 325 mg chewable, immediately.
- Nitroglycerin SL: q5min × 3 as needed, unless hypotensive, RV infarct suspected, or on PDE-5.
- Morphine IV for pain if still severe after nitro and hemodynamically stable.
- Orders:
- EKG (stat)
- CXR
- Troponin I/T
- CBC, BMP, coags, lipid panel
- Type and screen
- Fingerstick glucose
As soon as ST-elevation MI (STEMI) is confirmed:
Activate reperfusion:
- If PCI-capable hospital: “Cardiology consult,” “Prepare for emergent PCI,” “NPO”, “Consent for cardiac cath.”
- If no PCI available within 120 minutes: initiate thrombolysis (alteplase) after ruling out absolute contraindications.
Additional medications:
- High-intensity statin (atorvastatin 80 mg PO now)
- Beta-blocker (metoprolol) if no signs of acute heart failure, hypotension, or heart block
- Anticoagulation:
- IV heparin (unfractionated) or LMWH unless contraindicated
- P2Y12 inhibitor (clopidogrel or ticagrelor) if heading to PCI or thrombolysis
Key timing concept: Do not “wait” on troponin to treat a classic STEMI with diagnostic EKG. Treatment starts off the EKG, not the lab.
Disposition
- STEMI: ICU or CCU admission after reperfusion initiation.
- NSTEMI/Unstable angina:
- Admit to telemetry/step-down.
- Serial troponins, repeat EKGs.
- Start aspirin, statin, beta-blocker, anticoagulation, +/- early cardiology consult.
Common CCS mistakes:
- Managing clear ACS in clinic instead of ED.
- Forgetting aspirin early.
- Forgetting to advance time after stabilization (for serial enzymes or post-PCI course).
- Discharging too early without appropriate meds: ACEi, statin, beta-blocker, DAPT.
Acute Pulmonary Embolism: High-Yield Actions
PE cases test whether you recognize risk factors, order the right imaging, and anticoagulate promptly.
First steps (suspected PE in ED)
0–5 minutes:
- ED location.
- ABC + monitors, oxygen.
- If hemodynamically unstable (hypotension, syncope, shock):
- Consider massive PE.
- Bolus IV fluids.
- Vasopressors if needed.
- Echo (bedside) if CT not immediately feasible.
Testing:
- D-dimer only if low pretest probability and stable. CCS often skips this and expects you to go straight to imaging.
- Preferred imaging:
- CT pulmonary angiography (CTPA) if not contraindicated.
- V/Q scan if pregnancy, severe contrast allergy, or very high creatinine.
Labs:
- CBC, BMP, coags, troponin (risk stratification), ABG.
Treatment and timing
Do not wait for PE to “kill them” before starting anticoagulation.
- If moderate/high suspicion and no major contraindications:
- Start anticoagulation (IV unfractionated heparin or LMWH) as soon as imaging is ordered, especially if imaging will take time.
- If massive PE with hemodynamic instability:
- Systemic thrombolysis (alteplase) is high-yield.
- ICU admission.
Disposition:
- Stable PE: admit to ward or telemetry.
- Massive or submassive with RV strain: ICU.
Common CCS trap:
- Waiting for imaging, then ordering anticoagulation 2 simulated hours later. That delay costs points.
Sepsis and Septic Shock: The 1-Hour Bundle Mindset
If there is one scenario where timing is mercilessly graded, it is sepsis.

| Category | Value |
|---|---|
| Fluids | 10 |
| Antibiotics | 9 |
| Cultures | 7 |
| Lactate | 6 |
| Vasopressors | 8 |
Interpretation: Fluids and early antibiotics are the big-ticket items.
Recognizing the sepsis pattern
Typical CCS pattern:
- Febrile, tachycardic, hypotensive or borderline BP.
- Altered mental status or RR > 20.
- Source: pneumonia, UTI, abdominal infection, cellulitis.
Immediate management steps (0–10 minutes)
Orders to place simultaneously, ED or ICU depending on hypotension:
- ABC + monitors, oxygen.
- Two large-bore IVs.
- Labs:
- CBC, CMP, lactate, ABG if needed.
- Blood cultures × 2 from different sites.
- Urinalysis and urine culture.
- Site-specific cultures (sputum, wound, CSF if meningitis suspected).
- Imaging:
- CXR if respiratory symptoms.
- CT abdomen/pelvis if abdominal focus is suspected and patient stable enough.
Crucial timing:
- Broad-spectrum IV antibiotics within the first simulated hour. Without waiting on cultures.
- Fluid resuscitation:
- 30 mL/kg IV crystalloid bolus for hypotension or lactate ≥ 4.
If after fluids MAP < 65 mm Hg:
- Start vasopressors:
- Norepinephrine is first-line.
- Central line if needed (but on CCS, you can start norepi with “central venous catheter placement” order and then vasopressor).
Advanced moves
- ICU admission for septic shock.
- Order:
- Foley catheter for strict I&Os.
- Consider arterial line for continuous BP monitoring.
- Repeat lactate in 2–4 hours.
Time management: You must advance the clock in controlled increments:
- After initial orders: advance 30–60 minutes, reassess vitals, adjust fluids/pressors.
- After stabilization: advance 4–6 hours, reassess labs, cultures, mental status.
Common scoring killers:
- Delaying antibiotics for imaging.
- Under-resuscitating (e.g., 500 mL bolus in a 70 kg hypotensive patient and then stopping).
- Not escalating to ICU with persistent hypotension.
Stroke: Time-Sensitive Neurologic Emergencies
Stroke cases on CCS test your ability to:
- Rapidly identify stroke.
- Differentiate ischemic vs hemorrhagic.
- Hit or withhold thrombolysis correctly.
- Manage BP and secondary prevention.
First 10 minutes
Location: Emergency Department.
Simultaneous orders:
- ABC + monitors, IV access, oxygen.
- Fingerstick glucose (hypoglycemia can mimic stroke; correct immediately if low).
- Non-contrast CT head (stat).
- EKG, CBC, BMP, PT/INR, PTT.
- NPO status.
- Neurology consult.
Do not waste time ordering MRI before CT. Non-contrast CT is the first step to exclude hemorrhage.
Thrombolysis decision
Once CT confirms no hemorrhage and onset < 4.5 hours (for most patients):
- Evaluate contraindications:
- Recent surgery, active bleeding, very high BP uncontrolled, known intracranial pathology, etc.
- If eligible:
- Order IV alteplase (tPA) with appropriate weight-based dosing.
- Admit to ICU or stroke unit.
Blood pressure nuances:
- For tPA-eligible patients: lower BP below 185/110 before thrombolysis using IV labetalol or nicardipine.
- For ischemic stroke not getting tPA: permissive hypertension. Do not aggressively lower unless > 220/120 or specific comorbidities.
Post-tPA:
- No antiplatelet or anticoagulation for 24 hours.
- Repeat CT head if any neuro worsening.
If not tPA-eligible:
- Start aspirin.
- Admit to stroke unit/ward.
- Start workup: carotid ultrasound, echocardiogram, lipid panel, HbA1c, etc. (You can advance time to next day for these.)
Common CCS mistakes:
- Giving aspirin before head CT.
- Giving tPA despite unclear onset time (e.g., woke up with stroke).
- Dropping BP too aggressively and too quickly in ischemic stroke.
Acute Asthma and COPD Exacerbation
These cases are about rapid bronchodilation, steroids, oxygen, and disposition.
Asthma exacerbation
Initial ED orders:
- Oxygen, pulse ox, cardiac monitor.
- Nebulized albuterol + ipratropium (continuous or q20min).
- IV or PO steroids: methylprednisolone IV or prednisone PO.
- Peak expiratory flow or spirometry (if able).
- CXR if concern for pneumonia or pneumothorax.
- ABG if severe distress, exhaustion, or altered mental status.
Reassess after 30–60 minutes (advance the clock).
If improvement:
- Space out nebs.
- Continue steroids.
- Observe, then discharge with:
- Short steroid taper.
- SABA inhaler.
- Outpatient follow-up.
If not improving / impending respiratory failure:
- Admit to ICU.
- Consider magnesium sulfate IV.
- Oxygen, possible noninvasive ventilation.
- Intubation if:
- Rising CO2, altered mental status, silent chest.
COPD exacerbation is similar, with additional:
- Antibiotics (e.g., azithromycin or doxycycline) if infectious trigger likely.
- Noninvasive ventilation earlier for hypercapnic respiratory failure.
Common CCS traps:
- Managing moderate/severe exacerbations as an outpatient.
- Not escalating to ICU when CO2 climbing and mental status worsening.
Anaphylaxis: Seconds Matter
Anaphylaxis is one of the easiest high-yield CCS cases if you move fast.
Immediate orders (no delay)
Location: ED.
Simultaneous:
- IM epinephrine (0.3–0.5 mg of 1:1000) into lateral thigh. Repeat q5–15 min as needed.
- Oxygen, pulse ox, cardiac monitor.
- IV access, normal saline bolus.
- Adjuncts (after epi, not instead of):
- H1 blocker (diphenhydramine IV).
- H2 blocker (ranitidine or famotidine IV).
- Steroids (methylprednisolone IV).
If airway compromise:
- Prepare for intubation.
- Consider racemic epinephrine neb.
- Call anesthesia/ENT if difficult airway suspected.
After stabilization:
- Observe (4–24 hours depending on severity).
- Discharge with:
- Epi auto-injector prescription.
- Education about trigger avoidance.
- Referral to allergist.
Huge CCS mistake:
- Treating “anaphylaxis” with just steroids and antihistamines, forgetting epinephrine or delaying it.
Acute GI Bleed: Upper vs Lower, Orders and Timing
GI bleed cases test:
- Resuscitation.
- Early endoscopy/colonoscopy.
- Correct use of PPIs, octreotide, antibiotics in variceal bleed.
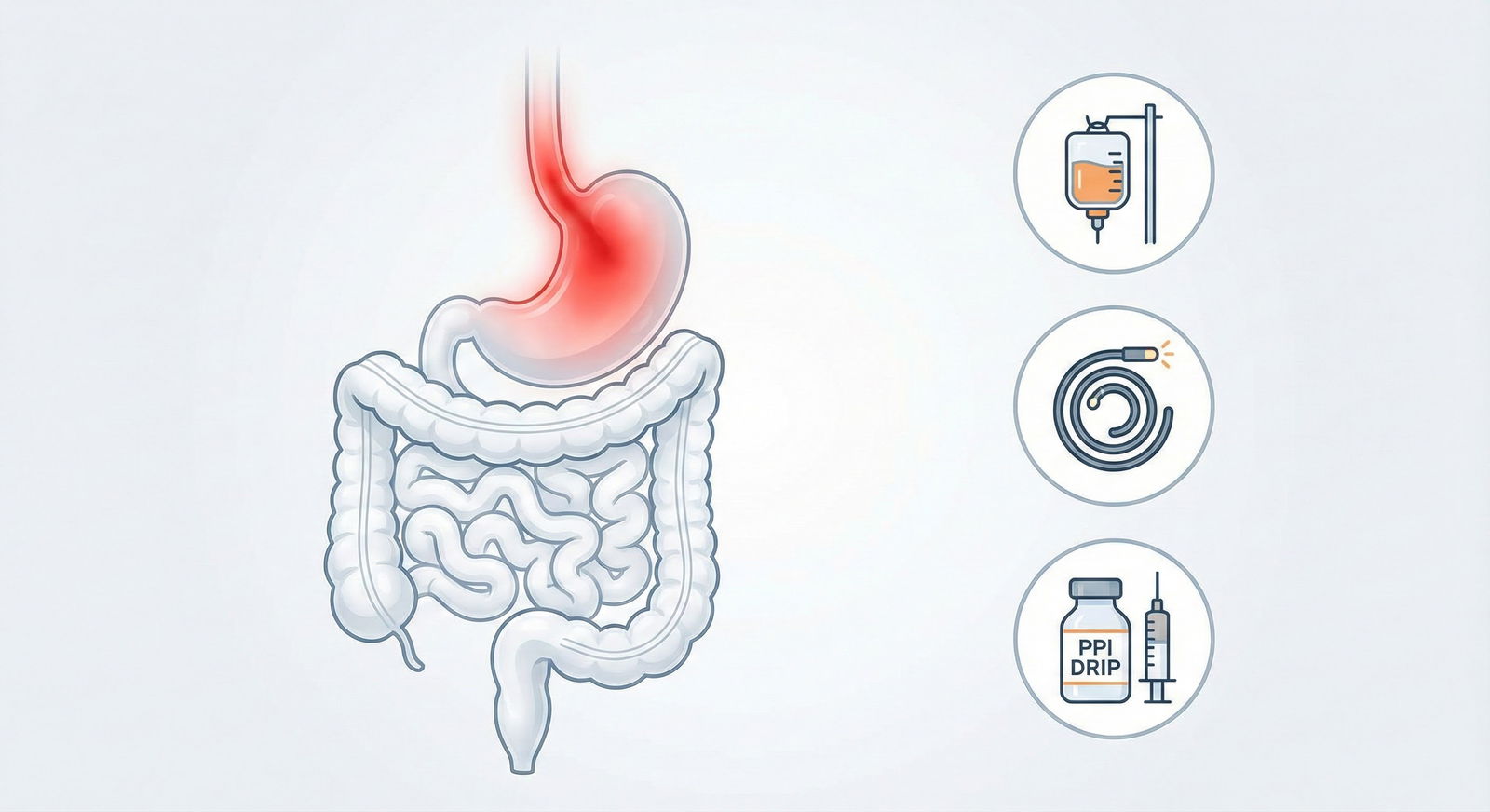
First steps (hematemesis or melena)
Location: ED.
Immediate:
- ABC + monitors, oxygen.
- 2 large-bore IVs.
- Type and crossmatch.
- CBC, BMP, LFTs, coags.
- IVF bolus if hypotensive.
- NPO.
- Proton pump inhibitor:
- IV PPI bolus and continuous infusion (e.g., pantoprazole).
If cirrhosis or variceal bleed suspected (history of liver disease, stigmata):
- Add:
- Octreotide IV bolus then infusion.
- Prophylactic antibiotics (e.g., ceftriaxone).
- Consider lactulose if encephalopathy.
Transfusion:
- PRBCs if Hgb < 7 (or < 8 with cardiovascular disease/symptoms).
- Platelets if very low or active bleeding with thrombocytopenia.
Consult:
- Gastroenterology.
- Order “Upper endoscopy (EGD)” once stabilized.
Timing:
- Stabilize first, then scope.
- Advance time a few hours to endoscopy, then act on findings (ligation, banding, etc.)
Disposition:
- Admit to ICU or monitored bed for significant bleed.
Lower GI bleed:
- Similar resuscitation.
- Colonoscopy once stable and prepped.
- If massive bleeding and unstable: consider surgery consult, tagged RBC scan / angiography.
Trauma and Head Injury
Trauma scenarios combine ABCs, imaging, and surgical consults.
Blunt trauma with hypotension
Location: ED.
Immediate:
- Trauma ABCs with cervical collar.
- Oxygen, cardiac monitor, IV access.
- IV crystalloids; if poor response, early PRBCs (massive transfusion protocol).
- FAST exam (Focused Assessment with Sonography in Trauma).
- Type and cross, CBC, BMP, coags.
- If unstable with positive FAST:
- Immediate surgical consult.
- Likely laparotomy.
CT scans:
- Only after hemodynamic stabilization.
- CT head, C-spine, chest/abdomen/pelvis with contrast if stable.
Head trauma specifics:
- GCS score, neuro checks.
- Non-contrast CT head for any LOC, neuro deficit, or anticoagulant use.
- Avoid hypotension and hypoxia aggressively.
If signs of increased ICP:
- Elevate head of bed.
- Mannitol (if herniation signs).
- Neurosurgery consult.
- Intubation with controlled ventilation; avoid hyperventilation except as a short bridge.
Common CCS trap:
- Sending an unstable trauma patient to CT instead of the OR.
Practical Time and Interface Management Tips
This is where strong students still leak points.

| Step | Description |
|---|---|
| Step 1 | Recognize emergency |
| Step 2 | Set location: ED/ICU |
| Step 3 | Order ABC + monitors |
| Step 4 | Order key labs/imaging |
| Step 5 | Immediate life-saving treatments |
| Step 6 | Set disposition/admit level |
| Step 7 | Advance clock and reassess |
| Step 8 | Refine treatment based on results |
| Step 9 | Stabilize and start long-term plan |
1. Batch orders
Do not:
- Order oxygen.
- Wait.
- Then order EKG.
- Wait.
- Then order labs.
On CCS, you can enter a whole stabilization package at once. Do it.
2. Advance time deliberately
After your first big batch:
- Advance 15–30 minutes in acute scenarios to see vitals respond.
- Then another 1–2 hours for imaging/labs.
- Do not jump 1–2 days forward from the ED in a crashing patient.
3. Disposition early
As soon as you have enough data:
- Click “Admit to ICU/ward” or “Discharge home.”
- For ED cases, the exam expects you to admit stable but serious diagnoses (MI, PE, pneumonia with hypoxia, DKA, sepsis). Do not leave them “floating” in ED for 24 simulated hours.
4. Don’t forget pain, DVT prophylaxis, and supportive care
After acute stabilization:
- Analgesia (within reason).
- DVT prophylaxis (heparin, LMWH, or SCDs) for admitted patients unless contraindicated.
- GI prophylaxis in ICU.
- Diet, activity level, nursing orders, and follow-up labs.
These do not carry the weight of tPA or epinephrine, but they matter at the margins.
Fast Reference: High-Yield Acute Orders by Scenario
| Scenario | Critical Early Orders |
|---|---|
| STEMI | ED, O2, EKG, ASA, nitro, morphine, troponin, heparin, statin, beta-blocker, PCI/tPA |
| Sepsis | ED/ICU, cultures, lactate, broad IV abx, 30 mL/kg fluids, pressors if needed |
| Stroke | ED, CT head (non-contrast), glucose, tPA if eligible, BP control, NPO, neuro consult |
| PE | ED/ICU, O2, CTPA or V/Q, anticoagulation, thrombolysis if massive, IVF, ICU if shock |
| Anaphylaxis | ED, IM epi, O2, IVF, H1/H2 blockers, steroids, airway prep |
| GI Bleed | ED, 2 large-bore IVs, type & cross, CBC, PPI, octreotide+abx if variceal, GI consult |
FAQs
1. How “aggressive” can I be with ordering tests in acute CCS cases without being penalized?
In acute, high-risk scenarios, the exam heavily favors being slightly over-aggressive rather than conservative. Ordering CT head + CXR + labs in a stroke with unclear onset is fine. You are penalized for missing time-sensitive imaging (like CT head in stroke or CTPA in suspected PE), not for a reasonable, guideline-consistent workup. What will hurt you is ordering low-yield outpatient stuff (like screening lipid panel) before stabilizing a crashing patient.
2. Should I always start with ABC and monitoring, even in cases that seem minor?
If the case looks clearly stable and outpatient (e.g., mild rash, chronic knee pain in clinic), you do not need full emergency ABC orders. But any case presented in ED, or any patient who has chest pain, dyspnea, fever with hypotension/tachycardia, altered mental status, trauma, or acute neurologic deficits deserves ABC + monitors immediately. The safest mental shortcut: if you would room this patient urgently in a real ED, do ABC + monitors.
3. How often should I advance the clock in acute scenarios?
General pattern:
- After your first stabilization orders: advance 15–30 minutes to see initial vitals/lab responses.
- After ordering imaging or major labs: advance 1–2 hours (enough time for results).
- Once patient is more stable on the ward/ICU: advance 4–8 hours or even to the next day for follow-up labs, imaging, and consult results. Avoid jumping many hours without any reassessment in a still-unstable patient.
4. Do I need to explicitly document diagnoses or just treat them?
You should use the “Diagnosis” or “Problem list” feature when it is available and the diagnosis is reasonably clear (e.g., STEMI, sepsis due to pneumonia, ischemic stroke). Scoring does give some credit for correctly naming the condition. However, treatment timing and appropriateness carry more weight. If forced to choose in time-pressured moments, prioritize ordering critical treatments over perfectly curating the problem list.
5. How exact do medication doses and routes need to be?
The CCS interface is fairly forgiving if you choose the correct drug, route, and general intent. It is not a pharmacology exam in the sense of precise mg/kg every time. For example, “IV ceftriaxone” vs “IV piperacillin-tazobactam” for severe sepsis is more about spectrum and route than the exact dosing interval. Wrong route (PO instead of IV in shock) or wrong class (metoprolol IV in acute decompensated HF with shock) will hurt you more than slight dose differences.
6. What is the single most common timing mistake strong test-takers make on CCS?
They treat ED cases too much like written vignettes: they make the right diagnosis but forget that time passes. They order the right antibiotics for sepsis but do not give fluids promptly. They wait to see CT results before starting anticoagulation in a patient with classic, high-probability PE. Or they leave a patient marooned in ED for 18 simulated hours instead of admitting to ICU/ward once enough data is in. If you fix your timing for antibiotics, reperfusion (MI, stroke), fluids/pressors, and epinephrine, your CCS score usually jumps.
Key takeaways:
- CCS rewards fast, bundled stabilization (ABC + monitors + key labs/imaging) tailored to the scenario, not piecemeal ordering.
- Life-saving interventions—aspirin and reperfusion for STEMI, tPA for stroke, antibiotics and fluids for sepsis, anticoagulation for PE, epi for anaphylaxis—must be early, not “eventually correct.”
- Treat location and time as active management tools: move patients to ED/ICU/ward appropriately and advance the clock in deliberate, small steps while reassessing and escalating when needed.






















