
Most people miss OB and newborn questions on Step 3 not because they “do not know OB,” but because they do not think in algorithms. That is the mistake.
Step 3 loves algorithmic, guideline-based care. Especially for obstetrics and newborns, where every decision has a clear sequence: assess, categorize, act. If you know those sequences cold, you turn a weak area into easy points.
Let me walk you through the specific algorithms you must have in your head. Not vague “concepts.” Actual if‑then steps.
1. First‑Trimester Vaginal Bleeding: The Miscarriage Algorithm
You will see this. A pregnant woman with bleeding and maybe pain. Your job is to classify the pregnancy status and act accordingly.
Step 1: Stabilize and Confirm Pregnancy
If she is hemodynamically unstable (hypotensive, tachycardic, heavy bleeding) → IV access, fluids, type and cross, prepare for possible D&C and call OB. On CCS, you need to do this immediately.
Then:
- Confirm pregnancy: serum β‑hCG (not just urine)
- Pelvic exam: amount of bleeding, cervical os open/closed, products of conception visible?
- Transvaginal ultrasound
Step 2: Interpret β‑hCG + Ultrasound
You need the discriminatory zone concept:
- β‑hCG ≥ ~1500–2000 and no intrauterine pregnancy on TVUS → think ectopic pregnancy
- β‑hCG below discriminatory zone and indeterminate ultrasound → repeat β‑hCG in 48 hours
Pattern of β‑hCG:
- Viable IUP: β‑hCG increases by ≥ 35% in 48 hours
- Failing pregnancy: β‑hCG plateaus or falls
Now the Step 3 classifications.
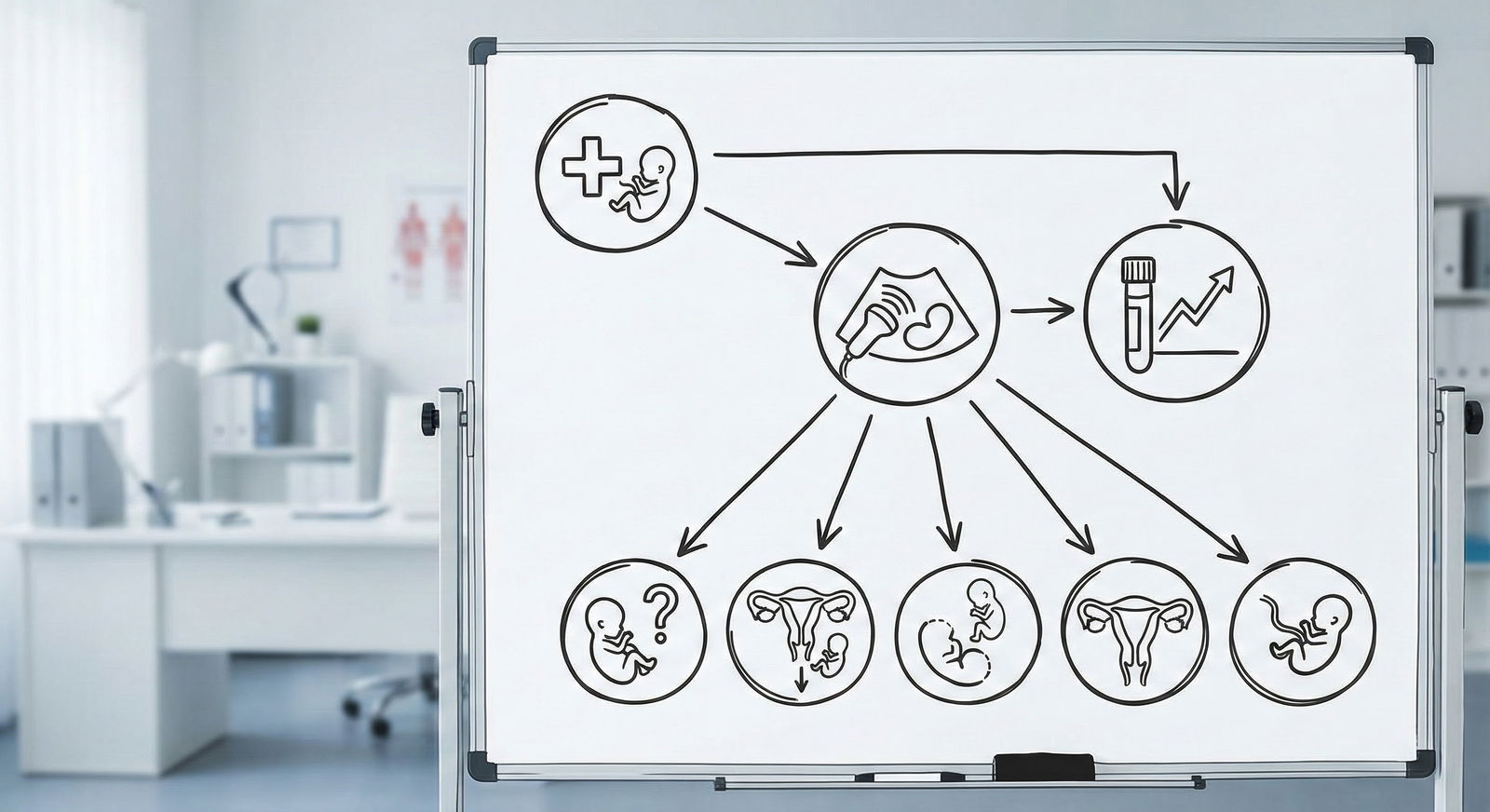
Step 3: Classify the Pregnancy
The exam will give you clues. Memorize this table:
| Type | Cervical Os | Ultrasound Finding | Bleeding/Pain |
|---|---|---|---|
| Threatened abortion | Closed | Live IUP, fetal cardiac activity present | Bleeding ± mild cramping |
| Inevitable abortion | Open | IUP; no passage of tissue yet | Bleeding + cramping |
| Incomplete abortion | Open | Some tissue expelled; tissue in uterus | Heavy bleeding, cramping |
| Complete abortion | Closed | Empty uterus; β-hCG declining | Bleeding resolved |
| Missed abortion | Closed | Nonviable IUP retained in uterus | Minimal/no bleeding |
Ectopic pregnancy sits aside this table: usually adnexal mass, no IUP on TVUS + β‑hCG above discriminatory zone, abdominal pain, sometimes bleeding.
Step 4: Management – What Step 3 Wants
Threatened abortion
- Stable, closed os, live IUP → Expectant management. Pelvic rest, reassurance, follow-up. No bedrest orders, no progesterone “just because.”
Inevitable / incomplete abortion
- Hemodynamically stable → options:
- Medical management with misoprostol
- Surgical D&C or manual vacuum aspiration
- Heavy bleeding, unstable, or infection → surgical evacuation + IV fluids ± antibiotics
Complete abortion
- Observe, repeat β‑hCG to ensure it trends down
- Rho(D) immune globulin (Rhogam) for Rh‑negative mothers with any bleeding
Missed abortion
- Options:
- Expectant (if early and patient prefers)
- Misoprostol
- D&C (especially if prolonged retention, bleeding, or infection risk)
Ectopic pregnancy (you need this algorithm too):
Unstable, peritonitis, or signs of rupture → Immediate laparotomy / laparoscopy
Stable, unruptured, early, and criteria for methotrexate:
- No fetal cardiac activity
- β‑hCG usually < 5000 (Step 3 is not obsessed with exact cutoffs, but “low”)
- No contraindications: liver/renal disease, breastfeeding, immunodeficiency → Give single‑dose methotrexate and follow β‑hCG
Failed methotrexate or not a candidate → laparoscopic salpingostomy or salpingectomy
Core memory for Step 3: For any Rh‑negative patient with bleeding, trauma, procedures, or pregnancy loss → give Rho(D) immune globulin unless father and fetus are conclusively Rh‑negative (which you almost never know on test day).
2. Hypertensive Disorders of Pregnancy: The Triage Algorithm
Pre‑eclampsia, severe pre‑eclampsia, eclampsia, HELLP. Step 3 loves these because there is a very specific escalation.
Categories You Must Differentiate
Gestational hypertension
- New onset BP ≥ 140/90 after 20 weeks
- No proteinuria, no severe features
Pre‑eclampsia without severe features
- BP ≥ 140/90 after 20 weeks on 2 occasions, AND
- Proteinuria (≥ 300 mg/24 hr, or protein/creatinine ratio ≥ 0.3, or dipstick ≥ 1+)
- No severe features
Pre‑eclampsia with severe features
Any of these:
- BP ≥ 160 systolic or ≥ 110 diastolic (2 readings, 4 hours apart)
- Thrombocytopenia (< 100,000)
- Elevated AST/ALT (twice normal)
- Renal insufficiency (Cr > 1.1 or doubling baseline)
- Pulmonary edema
- New‑onset cerebral or visual symptoms (headache, scotomata)
Eclampsia
- Pre‑eclampsia + generalized tonic–clonic seizures
HELLP
- Hemolysis, Elevated Liver enzymes, Low Platelets

| Category | Value |
|---|---|
| Gest HTN | 1 |
| Pre-E w/o severe | 2 |
| Pre-E w/ severe | 3 |
| Eclampsia | 4 |
| HELLP | 4 |
The numbers here are not “real,” they just visually emphasize the escalation of severity.
The Management Algorithm
Is she seizing?
- If yes → eclampsia. Immediate magnesium sulfate IV (4–6 g loading dose, then infusion), secure airway, control BP with IV labetalol or hydralazine, then plan for delivery once stable. Magnesium is not optional. On CCS, order it early.
Does she have severe features?
- Yes → pre‑eclampsia with severe features.
- Management:
- Magnesium sulfate for seizure prophylaxis
- BP control: IV labetalol, hydralazine, or oral nifedipine
- Delivery at ≥ 34 weeks, or earlier if maternal/fetal instability
- At < 34 weeks but stable → short course of corticosteroids for fetal lung maturity, then plan delivery
No severe features, gestational age:
- ≥ 37 weeks
- Pre‑eclampsia (without severe features) or gestational HTN → deliver (usually induce labor).
- 34–36+6 weeks
- Usually still watchful waiting with close monitoring if no severe features, but this is the gray zone. Step 3 will often steer you toward delivery if blood pressures are persistent or labs are not reassuring.
- < 34 weeks
- Expectant management:
- Frequent BP checks
- Weekly labs: platelets, creatinine, AST/ALT
- Fetal monitoring: NSTs, BPPs, growth ultrasound
- Emphasize: strict follow‑up, patient education about headache, visual changes, RUQ pain
- Expectant management:
- ≥ 37 weeks
Key drug details (they like specifics):
- First‑line acute BP control in pregnancy:
- IV labetalol
- IV hydralazine
- Oral nifedipine
- Avoid ACE inhibitors and ARBs (teratogenic).
- Magnesium toxicity signs: hyporeflexia, respiratory depression. If present, stop magnesium and give calcium gluconate.
Bottom line: Any OB hypertensive case on Step 3 is “Does she need magnesium? Does she need delivery now or close monitoring?” Think that way and you will not get lost.
3. Third‑Trimester Bleeding: Placenta Previa vs Abruption vs Vasa Previa
Third‑trimester bleeding questions are basically a classification game plus a “how to deliver” decision.
Differentiate the Big Three
Placenta previa
- Placenta overlies or very near internal cervical os
- Classic: painless bright red vaginal bleeding in third trimester
- NO digital vaginal exam before ruling out placenta previa by ultrasound. That is a guaranteed test trap.
Placental abruption
- Premature separation of placenta from uterine wall
- Painful vaginal bleeding, uterine tenderness, hypertonic “board‑like” uterus
- May have fetal distress, DIC risk
Vasa previa
- Fetal vessels overlying the cervical os in membranes
- Painless bleeding after ROM; fetal tachycardia then bradycardia, sinusoidal tracing, rapid fetal exsanguination. Very high fetal mortality if not recognized.

| Step | Description |
|---|---|
| Step 1 | Third-trimester bleeding |
| Step 2 | Assess maternal vitals & fetal status |
| Step 3 | Resuscitate, prepare for emergency delivery |
| Step 4 | Transabdominal ultrasound |
| Step 5 | No vaginal exam, schedule C-section |
| Step 6 | Consider abruption vs other causes |
| Step 7 | Stable? |
| Step 8 | Placenta previa? |
Management Priorities
Stabilize mother first
- IV access, fluids, type and cross
- Fetal monitoring (continuous if possible)
Placenta previa
- Confirm via ultrasound (transabdominal then transvaginal if needed)
- No digital vaginal exams
- Management:
- If minimal bleeding, preterm, stable → pelvic rest, avoidance of intercourse, observation
- If term or heavy bleeding/instability → C‑section delivery
- Don’t try to induce vaginal delivery with placenta previa. That is wrong.
Placental abruption
- Clinical diagnosis: painful bleeding, uterine tenderness, maybe concealed bleeding with shock
- Management:
- Stabilize mother
- If severe abruption or fetal/maternal instability → immediate delivery (usually emergent C‑section)
- If mild abruption and fetus/mother stable near term → usually proceed to delivery but mode depends on circumstances; but Step 3 will usually push you toward C‑section if fetal distress
Vasa previa
- Sudden bleeding after ROM + fetal bradycardia
- Immediate C‑section. There is no time for messing around with amnioinfusion or tocolysis.
4. Fetal Heart Rate Tracing: Category I–III and What You Do
If you cannot read fetal heart tones, Step 3 will punish you. This is one place where algorithmic thinking is obvious.
Categories
Category I (normal)
- Baseline 110–160
- Moderate variability (6–25 bpm)
- No late or variable decelerations
- ± accelerations, ± early decels
Category II (indeterminate)
- Everything that is not I or III
Category III (abnormal) – memorize this:
- Absent variability AND any of:
- Recurrent late decelerations
- Recurrent variable decelerations
- Bradycardia
- Or, sinusoidal pattern
Deceleration Types
- Early decels: mirror contractions → head compression → benign
- Variable decels: abrupt, variable timing → cord compression
- Late decels: begin after contraction starts, nadir after peak → uteroplacental insufficiency → more concerning
The Intervention Algorithm
On Step 3, they want “intrauterine resuscitation” steps first, then C‑section if not improving.
For recurrent variable or late decels (Category II/III pattern):
- Maternal position change (left lateral)
- Oxygen via face mask
- Stop oxytocin (if running)
- IV fluid bolus
- Consider tocolysis if uterine tachysystole
- Amnioinfusion for recurrent variable decels due to cord compression (if intrauterine pressure catheter is in and no contraindications)
If Category III pattern persists despite interventions → emergent C‑section.
Do not order “reassure the patient and observe” when you have persistent late decelerations and absent variability. That is how you miss points.
5. Immediate Newborn Assessment: The Delivery Room Algorithm
Switch gears. Now the baby is out. What do you do in the first minute? If you know the steps, any CCS case with a newborn becomes automatic.
The Three‑Question Triage
Right after birth, ask:
- Term gestation?
- Good tone?
- Breathing or crying?
If the answer is “yes” to all three:
- Routine care: dry, warm (radiant warmer), clear airway PRN, ongoing evaluation.
- Delayed cord clamping if no contraindications (Step 3 sometimes nods to this, but it is background).
If “no” to any:
- Start the Neonatal Resuscitation Program (NRP) sequence.
Basic NRP Algorithm (simplified for Step 3)
- Provide warmth, position airway, clear secretions if needed, dry, stimulate
- Check respirations and heart rate
If apneic or HR < 100:
- Start positive pressure ventilation (PPV) with bag‑mask
- Target: HR > 100 and spontaneous breathing
After 30 seconds of effective PPV:
- HR ≥ 100: continue support as needed
- HR 60–99: continue PPV, correct technique
- HR < 60: start chest compressions + PPV; consider epinephrine if no improvement
On CCS, you will not be asked minutiae of ET tube depth, but you should:
- Order: “Oxygen by bag and mask,” “Intubation” if PPV is inadequate, “Cardiac monitor,” “Pulse oximetry”

| Category | Value |
|---|---|
| Birth | 140 |
| 30 sec | 80 |
| 60 sec | 60 |
| 90 sec | 120 |
This is conceptual: HR dropping, then rising after intervention.
APGAR Scores
APGAR is tested, but not as management‑determining as some students think. Basic points:
- Scored at 1 and 5 minutes
- 7–10: normal, routine care
- 4–6: moderate depression → resuscitation/observation
- 0–3: severe depression → immediate resuscitative efforts
The exam uses APGAR more as descriptive context than a rigid treatment guide. Focus more on HR, respirations, tone in the question stem.
6. Hyperbilirubinemia in the Newborn: Who Needs Phototherapy?
The jaundice algorithm is a classic Step 3 trap. They will give you a bilirubin value, an age in hours, and a baby that “looks well.”
Step 1: Conjugated vs Unconjugated
Conjugated (direct) hyperbilirubinemia is always pathologic
- Causes: biliary atresia, neonatal hepatitis, metabolic disorders
- Management: evaluate, do not give phototherapy “as the main fix”
Unconjugated (indirect) hyperbilirubinemia is extremely common
- Physiologic jaundice
- Breastfeeding failure jaundice
- Breast milk jaundice
- Hemolysis (ABO/Rh incompatibility, G6PD, spherocytosis)
Step 2: Age in Hours + Total Bilirubin
You are not going to memorize the entire AAP bilirubin nomogram, but you must know relative thresholds.
General patterns:
- Jaundice in first 24 hours of life is pathologic → think hemolysis or sepsis. That infant needs evaluation, not “reassurance.”
- Phototherapy thresholds are lower in:
- Premature infants
- Sick infants
- Very young age in hours
Step 3 will usually simplify with statements:
- “Total serum bilirubin 18 mg/dL at 36 hours in a term infant, Coombs positive” → Phototherapy now.
- “Total bilirubin 11 mg/dL at 3 days in a term infant who is feeding well” → Observation, ensure adequate feeding.
- “Total bilirubin 25 mg/dL in term infant” → Exchange transfusion due to risk of kernicterus.
Rough Decision Points for a Term, Otherwise Healthy Infant
These are not exact AAP lines, but Step‑3‑useful:
- TSB ≤ 12 at 48 hours, well infant → Usually observe
- TSB 15–20 range in first 48–72 hours → Phototherapy
- TSB ≥ 25 (or very high with neurologic symptoms) → Exchange transfusion
Risk factors raising concern:
- Hemolysis (positive Coombs, anemia, high retic)
- Prematurity
- Significant bruising/cephalohematoma
- Sibling with severe jaundice
Algorithm:
- Identify early onset (< 24 hours) vs later
- Check for hemolysis (Coombs, blood type, retic count)
- Determine conjugated vs unconjugated fraction
- Use age in hours + TSB to decide:
- Reassure ± ensure adequate feeding + follow‑up
- Start phototherapy
- Plan exchange transfusion for very high levels or signs of acute bilirubin encephalopathy
7. Neonatal Sepsis and Fever: The “Culture and Cover” Algorithm
Step 3 is unforgiving if you understimate a febrile neonate. The algorithm is simple: young = full workup.
Age Matters
0–28 days (neonate)
- Any fever ≥ 38°C (100.4°F) → full sepsis workup + empiric IV antibiotics + admission.
29–60 days
- Still high‑risk, but there is some nuance with “low‑risk” criteria. For Step 3, they usually still like a fairly aggressive workup, at least blood and urine cultures ± LP depending on how the question is written.
Workup in Neonate with Fever
For 0–28 days:
- Blood culture
- Urine culture (via catheterization or suprapubic tap, not bag)
- Lumbar puncture with CSF analysis and culture
- CBC, CRP ± procalcitonin
- Chest X‑ray if respiratory signs
Empiric antibiotics:
- Ampicillin + gentamicin OR
- Ampicillin + cefotaxime (avoid ceftriaxone in neonates due to risk of kernicterus / biliary sludging)
You treat first. You do not wait for cultures to come back.
For older infant (e.g., 2–3 months), Step 3 might reward you for using a risk stratification approach, but the principle is: any toxic‑appearing infant gets full workup and IV antibiotics.
8. Preterm Labor and Tocolysis: When to Stop the Uterus, When to Deliver
Another very Step‑3‑ish algorithm: pregnant patient with contractions before 37 weeks.
Step 1: Confirm Preterm Labor
Criteria:
- Regular uterine contractions AND
- Cervical change (dilation and/or effacement)
Random Braxton Hicks with a closed cervix is not preterm labor. No tocolysis, just reassurance and hydration.
Step 2: Gestational Age Drives Management
- < 34 weeks with true preterm labor:
- Antenatal corticosteroids (betamethasone) to mature fetal lungs
- Tocolysis for 48 hours to allow steroids to work, if no contraindications
- Magnesium sulfate for neuroprotection if < 32 weeks
- 34–36+6 weeks:
- Generally no tocolysis. Steroids may still be considered up to 36+6 in some guidelines, but the test often emphasizes steroids mostly < 34 weeks.
- Most often, allow labor to progress.
Common tocolytics:
- Nifedipine (calcium channel blocker)
- Indomethacin (NSAID; avoid after 32 weeks due to risk of premature PDA closure)
- Terbutaline (beta‑agonist, more side effects; Step 3 likes nifedipine/indomethacin more)
Contraindications to tocolysis (you are expected to recognize these):
- Intrauterine fetal demise
- Fetal anomaly incompatible with life
- Non‑reassuring fetal status
- Severe pre‑eclampsia/eclampsia
- Maternal hemodynamic instability or severe hemorrhage
- Chorioamnionitis (infection)
Group B Strep prophylaxis:
- At ≥ 37 weeks, standard based on GBS status
- At preterm labor with unknown GBS → give intrapartum penicillin
9. How to Actually Study These Algorithms for Step 3
Reading them once does nothing. You need to internalize them so that when a CCS case or MCQ drops a vague OB vignette, your brain auto‑runs the right sequence.
Here is how I have seen people do it effectively:
- Make 1–2‑page sheets of just algorithms: first‑trimester bleeding, hypertensive disorders, labor FHR management, neonatal jaundice, sepsis workup.
- Draw your own mini flowcharts. Not pretty, not color‑coded. Just boxes and arrows. The act of drawing solidifies it.
- When you do UWorld Step 3 questions:
- After each OB/newborn question, pause and ask: “What algorithm was this testing?”
- Write that algorithm title at the top of the explanation page.
- For CCS, practice entering orders in the correct order:
- OB bleeding: vitals, IV access, type & cross, CBC, β‑hCG, ultrasound
- Neonatal fever: blood culture, urine culture (catheter), LP, CBC, CRP, then ampicillin + gentamicin/cefotaxime, then admit
You are not memorizing hundreds of facts. You are memorizing maybe 10–12 decision trees.
Once those are in your head, OB and newborn questions become low‑stress points, not landmines.
FAQ (exactly 4 questions)
1. How heavily is OB/newborn content tested on Step 3 compared with other specialties?
OB and newborn content is not the majority of the exam, but it is overrepresented relative to how much time many residents spend on those services. You will see several MCQs and at least a couple of CCS cases where pregnancy, labor management, or newborn care is central. The problem is not volume; it is that the questions are clustered around algorithms many internal medicine–tracked residents never internalized. That makes OB feel harder than it should be.
2. Do I need to memorize gestational age cutoffs exactly (34 vs 37 weeks, etc.) for decisions like tocolysis and delivery?
You need the major cut points, not every micro‑nuance. The key ones: 20 weeks for viability, 34 weeks for most tocolysis and steroid decisions, 37 weeks for term, and 32 weeks for indomethacin avoidance and magnesium for neuroprotection. The question stems usually give contextual clues, but if you know those cutoffs, you will choose the right side 95% of the time.
3. How detailed do I need to be about bilirubin thresholds for phototherapy on Step 3?
You do not need the exact AAP nomogram saved in your head. You do need to know that jaundice in the first 24 hours is pathologic, that moderate levels during days 2–3 in a term well infant may be monitored, and that higher levels in the mid‑teens to twenties in the first few days, especially with hemolysis or prematurity, require phototherapy. Extremely high levels (around mid‑20s) or neurologic signs suggest exchange transfusion. Relative position on that scale is enough for the exam.
4. What is the single most high‑yield OB algorithm to master for Step 3 if my time is limited?
Pre‑eclampsia/eclampsia and severe features management. If you can look at a pregnant woman’s BP, labs, and symptoms and immediately decide: “she needs magnesium, she needs BP control, and she needs delivery now vs close monitoring,” you will capture a disproportionate number of OB points. Right behind that, I would put first‑trimester bleeding classification (threatened vs inevitable vs incomplete vs complete vs ectopic) as your second non‑negotiable algorithm.






















