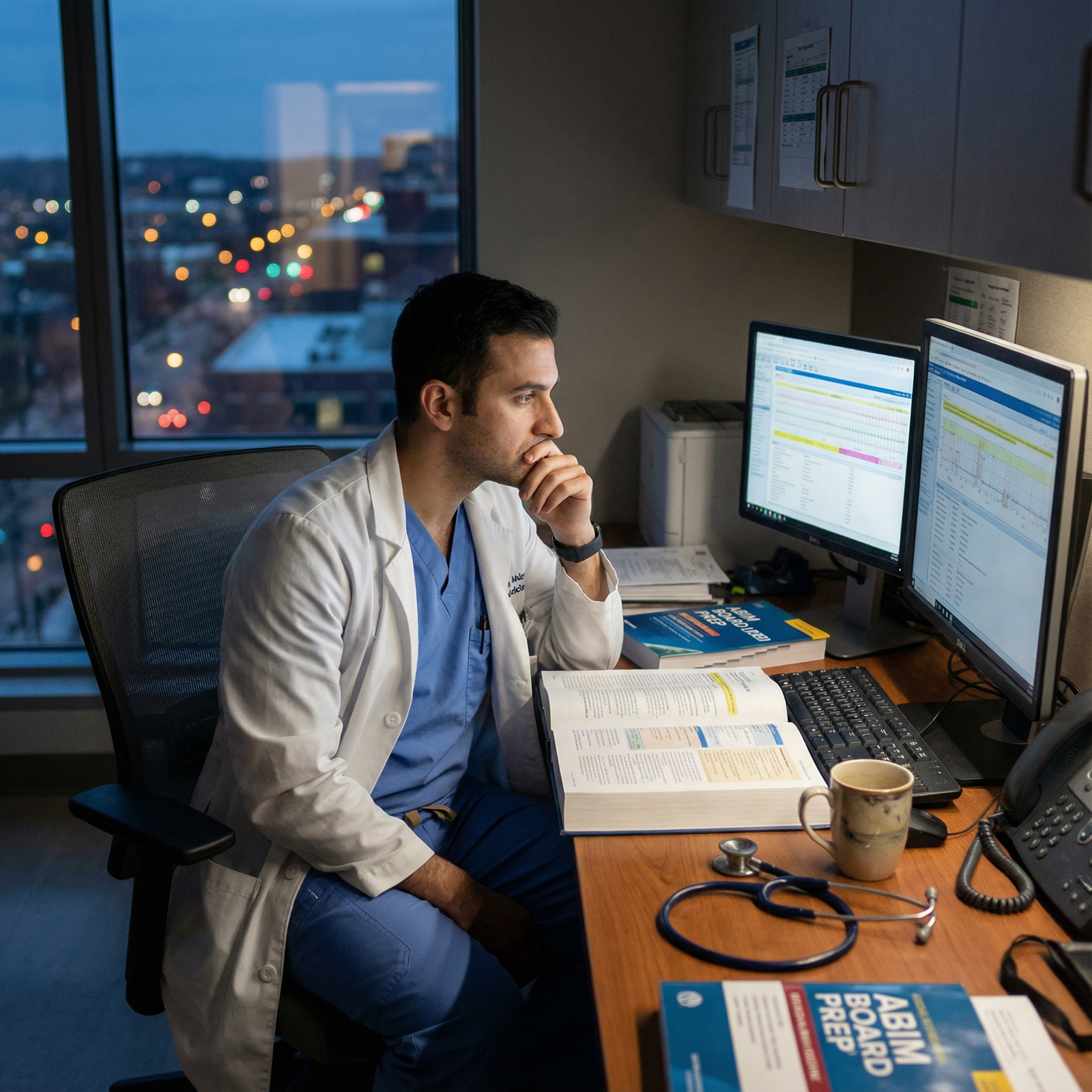
It is 2:17 a.m. You are on your “golden” internal medicine rotation, telling yourself this is fine, this is normal, this is temporary. You watched the night float resident click through 60 notes, chase three hypotensive calls, argue with radiology, and wolf down cold fries at 1:30 in the morning. And still, you are thinking, “Residency will be hard, but after that, IM has good lifestyle,” or “Neurology weekends look lighter; stroke call will be intense, but manageable.”
This is where people set themselves up for burnout.
Not because IM or neurology are “bad lifestyle” specialties. They are not. The problem is the stories applicants tell themselves. The blind spots. The assumptions. The “I’m sure I’ll be able to…” fantasies that fall apart six months into PGY-1 when you are crying in the stairwell over a non-urgent MyChart message.
Let me be direct: I have watched strong, motivated people burn out in both IM and neurology not because of the medicine, but because of lifestyle assumptions they never interrogated. They matched into the specialty they thought they understood. They did not.
This is the article where I try to stop you from making the same mistakes.
Blind Spot #1: Confusing “Flexible” with “Humane” in Internal Medicine
You will hear this phrase a lot:
“Internal medicine is flexible. You can make your own lifestyle.”
A lot of applicants stop listening after “flexible” and mentally translate it into “good lifestyle.” That is the first trap.
What “flexible” actually means in IM:
- You can end up as:
- A hospitalist on 7-on/7-off, 12–14 hour days
- A subspecialist with intense call (cards, GI, pulm/crit)
- A clinic-based general internist drowning in inbox messages
- The lifestyle spread is massive. From “pretty cushy” to “permanently tired.”
The mistake: choosing IM thinking “I will just pick a chill path later” without understanding:
- Which paths are actually chill (far fewer than you think).
- What you need (personally) to not burn out.
- How competitive those “cushier” options can be locally.
Here is the other part applicants miss: the baseline work culture you absorb during residency sets your expectation for “normal.” If you train in a malignant or just chronically overworked IM program, you may come out believing that:
- Working through lunch is standard.
- Charting at home most nights is expected.
- Saying no to extra shifts is selfish.
By the time you realize you are burning out, you have already normalized an unhealthy baseline.
The residency years themselves
Do not romanticize them. IM residency is:
- Rotations with:
- Q4 call or long-call systems
- 28-hour shifts (or “24+4”) at many places
- Night float blocks that wreck your circadian rhythm
- A culture where:
- Notes, documentation, and discharges are constant
- Patient volume is high
- You carry the “primary team” responsibility for complex, multi-problem patients
Your blind spot might be thinking: “Everyone suffers during residency, but then it gets better.” Sometimes true. Sometimes not.
The error is making a major life choice assuming future lifestyle will compensate for present misalignment. If you already dread:
- Prolonged computer work
- Continuous low-level cognitive strain
- Coordinating care and logistics more than “actual medicine”
then internal medicine may erode you faster than you expect.
Blind Spot #2: Underestimating Invisible Cognitive Load in Neurology
Neurology applicants often latch onto a seductive narrative:
- Fewer codes than IM.
- Less “all-the-things-all-the-time” chaos.
- “Interesting patients, fascinating localization, intellectually satisfying.”
Fine. But here is what people gloss over: neurology’s burnout often comes from cognitive and emotional load, not only hours.
Common naive assumption:
“As long as I read and understand the pathways, neurology will be intellectually demanding but emotionally lighter.”
Wrong. The emotional weight is different, not lighter.
Typical neurology realities that wear people down:
- Endless:
- Devastating prognostic conversations (massive stroke, ALS, severe anoxic injury)
- Family meetings about withdrawal of care or trach/PEG decisions
- Patients who do not improve, or do so minimally
- Chronic follow-up of:
- Progressive neurodegenerative disease you cannot “fix”
- Refractory epilepsy, chronic migraine, functional disorders
- A lot of patient interactions that end with:
- “We cannot cure this.”
- “We are managing symptoms and decline.”
Many neurology residents are blindsided by how much grief, frustration, and hopelessness they absorb. They came for the localization puzzles. They stayed up at 3 a.m. replaying their words to a daughter asking if her father will ever speak again. That is a different type of burnout.
Blind Spot #3: Misreading Schedules and FTEs
Applicants obsess over “hours per week” as if it is a single clean number.
They ask: “How many hours do your residents work?” “How many hours as an attending?” Then they nod at answers like “60–70 as a resident” or “45–55 as an attending” and move on.
You need to be smarter than that.
| Topic | Assumption | Typical Reality |
|---|---|---|
| Hospitalist schedule | 7-on/7-off = half-time | Actually closer to 1.0+ FTE in 7 days |
| Clinic IM | 8–5, predictable | Inbox + documentation outside clinic hours |
| Neuro call | Only stroke alerts, manageable | Frequent pages + night decision fatigue |
| Academic jobs | Protected time = less work | Clinical + admin + research bleed together |
| Outpatient neuro | “Clinic-based = easy lifestyle” | Chronic complex patients + long visits |
Here is what people ignore:
Seven-on/seven-off is not half-time.
Those 7 days can be 12–13 hours each, plus work at home. That is an 84–90+ hour week compressed into half the month. Your body and brain do not experience that as “50% job.”Clinic life is not 8–5.
I have watched outpatient internists and neurologists:- Log in at 6:30 a.m. to prep
- See patients 8–5
- Finish notes and inbox from 5–7 p.m.
- Then squeeze in portal messages “after kids are asleep”
FTE games.
A “0.8 FTE” contract may still feel like a full FTE job if:- Panel sizes are not adjusted
- Admin and meeting load does not scale down
- Call expectations stay the same
If you are basing your burnout risk calculation on naive “hours per week” numbers without investigating how those hours are structured, you are setting yourself up for a nasty surprise.
Blind Spot #4: Ignoring Call Culture (This One Breaks People)
Both IM and neurology applicants routinely fail to ask the only question that matters:
“What does call do to people here?”
Not “what is the schedule on paper?” but:
- How often are people:
- Crying after a run of bad nights?
- Falling asleep on public transport?
- Making real mistakes from fatigue?
- How many residents:
- Drop to 80% effort just to survive?
- Take anxiety meds or antidepressants mid-residency?
You know what I have seen?
Internal Medicine call patterns that crush people
- Night float blocks where:
- One resident cross-covers 80–100 patients
- Admissions keep coming past 2 a.m.
- “Protected sign-out time” is a joke
- Step-down / telemetry nights where:
- You are constantly paged for minor issues
- Your sleep is fragmented into 15-minute intervals
- “Short call” that somehow stretches into 10 p.m. regularly
Neurology call patterns that quietly erode people
Not always as physically brutal, but:
- Stroke neurology:
- Multiple stroke codes per night
- Constant decision-making under time pressure: tPA vs no tPA, thrombectomy vs no thrombectomy
- Documentation and phone calls around high-risk decisions
- General neuro call:
- Every weird symptom gets triaged to neuro
- You manage seizures, encephalopathy, headache, functional disorders, spinal issues
This is more dangerous than pure physical exhaustion: it is continuous decision fatigue. The kind that drops your empathy reserves to zero and makes every patient feel like an enemy of your sleep.

| Category | Value |
|---|---|
| Hours | 70 |
| Documentation | 85 |
| Call/Nights | 90 |
| Emotional Burden | 80 |
| System Issues | 75 |
The mistake is thinking, “I handled surgery call; I can handle anything.” IM and neurology call are different beasts. Less blood. More uncertainty. Endless decisions in gray zones. If you do not ask hard questions about call culture, you are gambling.
Blind Spot #5: Underestimating Inbox, Documentation, and “Soft Work”
Burnout in both IM and neurology is often death by a thousand clicks, not a single massive trauma.
Lifestyle expectations usually ignore “soft work”:
- MyChart messages
- Refill requests
- Prior auths
- “Review this MRI” messages
- Care coordination messages from other specialists
- Disability paperwork, FMLA, letters
Applicants fantasize about seeing fewer patients or “lighter clinics” without thinking about the shadow workload attached to each patient.
Typical pattern:
- During residency: most of this is shielded from you.
- As an attending: it hits you all at once.
I have watched new outpatient internists say, “I have 14–18 patients a day, this should be fine,” and then drown in:
- 40+ inbox messages daily
- Complex multi-morbidity that needs phone calls and coordination
- Patients who expect 24-hour response times because the portal makes them think this is texting
Neurology is no better. Actually worse in some subspecialties:
- Chronic migraine:
- Prior auth battles for CGRP inhibitors, Botox, triptans
- High volume of portal messages about incomplete relief
- Epilepsy:
- Repeated med adjustments
- Driving paperwork
- Ongoing safety counseling documentation
- MS / neuroimmunology:
- High-cost meds, insurance drama, labs, MRI scheduling, monitoring
The blind spot is thinking “clinic-based = easier lifestyle.” It can be. If the clinic is staffed properly. If the system respects physician time. Many do not.
Blind Spot #6: Misjudging Your Own Tolerance for Tragedy vs Chaos
Here is where IM and neurology differ in ways that actually matter for burnout.
Internal medicine:
- Daily chaos:
- High patient volume
- Discharges and admissions constantly shifting
- Cross-cover emergencies of all kinds
- Emotional load:
- Patients often older, multi-morbid, but many do improve
- More “we can manage this” conversations than “nothing left to do”
Neurology:
- Less raw volume usually, but:
- More truly devastating life events per patient
- More permanent disability, cognitive change, personality changes
- Often confronting “who is this person now?” with families
You need to be honest about which kills you faster:
- Constant multi-problem juggling and logistics chaos (IM)
- Sustained proximity to irreversible brain injury and suffering (Neuro)
The mistake is assuming “I like brain stuff on Step 1, so I will handle real-world neuro fine.” Or “I like variety, so IM will be energizing.”
No. You have to watch yourself on rotations:
- On IM wards:
- Do you feel alive or depleted after a busy call day?
- Does endless med rec + disposition planning frustrate you more than the sick patients themselves?
- On neurology:
- How do you actually feel after giving a family an ALS diagnosis?
- Do stroke alerts energize or drain you?
Your future burnout risk is written in your real-time reactions, not your personal statement.
Blind Spot #7: Ignoring Local Job Market Reality
Applicants love to say, “I will just pick a job that fits my lifestyle needs.”
As if that is always an option.
Reality check:
- In many regions, IM hospitalist jobs:
- Come with heavy night coverage
- Are built around 7-on/7-off, no real step-down model
- Pay well but expect constant throughput and RVUs
- Outpatient IM:
- Primary care panels are often overloaded
- Admin support is variable
- Neurology:
- Many groups are short-staffed and desperate, which can mean:
- Heavy call expectations
- Long waitlists = pressure to see more patients per day
- Subspecialty neurology jobs may cluster in academic centers, not where you want to live
- Many groups are short-staffed and desperate, which can mean:
You can match into “flexible” specialties and still end up trapped in jobs that do not match your lifestyle assumptions, because:
- Your family is geographically limited.
- Certain subspecialties are saturated in your area.
- The “dream job” requires academic output you do not have.
Burnout accelerates when reality corners you into “accept bad or uproot your entire life.”
Blind Spot #8: Treating Wellness as a Perk Instead of a Cultural Signal
You have seen the brochures: wellness committees, yoga sessions, free coffee, resident retreats.
Do not be fooled.
Look for more serious signals:
- Do residents:
- Actually take their PTO? Or are they guilted / blocked?
- Come in on days off for unfinished work or results?
- Do attendings:
- Talk openly about burnout and boundaries?
- Leave on time sometimes? Or are they permanent fixtures at the workstation?
- Does the program:
- Refuse to expand class size while workload explodes?
- Actually care how many patients are on each team?
A red flag I have seen repeatedly:
- Programs brag about:
- Moonlighting opportunities.
- Tons of procedures.
- Residents “so competent they can handle 20+ patients easily.”
Translation: you will probably be under-supported and overextended. Your “competence” is being weaponized against you.
If you pick IM or neurology training based purely on name, prestige, or fellowship pipeline without looking at how alumni actually live five years out, you are begging for trouble.
Practical Questions You Should Actually Be Asking
You want to avoid burnout blind spots? Then stop asking generic “How is your work-life balance?” nonsense and ask questions that force honesty.
For current residents and attendings:
- “What time do you usually log out of the EMR on a clinic day? Including work from home.”
- “How many nights a month are you up more than 2–3 times on call?”
- “How many of your co-residents have reduced FTE or left medicine entirely?”
- “What parts of your job would you change first if you had the power?”
- “If your own kid wanted to go into IM/Neuro, would you recommend it here?”
For program directors / leadership:
- “In the last five years, how many residents required mental health leave?”
- “What has changed structurally in your program to reduce burnout?”
- “How many faculty have left in the last 3 years, and why?”
- “What is your average patient load on wards / in clinic, and who decided that number?”
And crucially, for yourself:
- “Do I feel more drained by:
- Volume and administrative chaos? (leans against IM)
- Tragic, irreversible diagnoses and long-term suffering? (leans against Neuro)”
- “Do I need predictability, or can I tolerate spike-and-crash schedules like 7-on/7-off?”
- “Do I recover from stress quickly, or does each bad call week take me a month to get over?”
You cannot outsource these answers.
One More Subtle Trap: Over-Indexing on Prestige
I have watched this play out too many times:
- A student loves outpatient neurology but matches at a big-name, hyper-acute stroke-heavy program because “prestige.”
- Another loves relationship-based internal medicine but chooses a high-powered tertiary IM program with toxic volume because “fellowship options.”
Both burn out. Not because they were weak. Because they betrayed their own preferences to chase status.
If your actual day-to-day joy will come from:
- Slower clinics
- More time per patient
- Fewer beds, more brain space
then choosing a prestige-driven, volume-obsessed environment is a direct road to hating your life, whether the specialty is IM or Neuro.

| Step | Description |
|---|---|
| Step 1 | Choose Specialty |
| Step 2 | Better specialty fit |
| Step 3 | Misaligned expectations |
| Step 4 | High burnout risk |
| Step 5 | Lower burnout risk |
| Step 6 | Based on honest self assessment |
| Step 7 | Program culture healthy |
FAQ (Exactly 5 Questions)
1. Is internal medicine or neurology “better” for lifestyle long term?
Neither is inherently better. Internal medicine tends to have a wider spread of possible lifestyles (from intense ICU or hospitalist work to relatively reasonable outpatient roles), but the variability is huge and highly local. Neurology often has moderate clinic-based schedules but heavy emotional and cognitive load, plus stroke call intensity. The right answer depends entirely on what kind of stress you tolerate better: volume/chaos vs. tragedy/irreversibility.
2. Are things really that different after residency, or does burnout just persist?
For many, things improve after residency. But it is not automatic. If you roll straight from a brutal training program into a high-RVU, under-staffed job “because the pay is good,” you can stay burned out or get worse. The people who truly improve post-residency are the ones who deliberately choose:
- Reasonable panel sizes or patient caps
- Supportive environments
- Schedules aligned with their energy and family needs
Not the ones who just accept the first job offer.
3. Can I protect myself from burnout by planning to work part-time later?
“Future part-time” is a fantasy many people cling to and never actually reach. Barriers:
- Financial pressure (debt, cost of living, lifestyle inflation)
- Culture that shames reduced FTE
- Partners or groups that “do not do part-time” If your survival plan for a demanding specialty is “I will just go 0.6 FTE later,” you need to confirm that such roles actually exist in your target region and are socially accepted in your field.
4. I like both IM and neurology. How do I choose without burning out later?
Watch yourself carefully on rotations. When you leave a busy IM day vs a busy neurology day, which type of tired do you prefer? Which annoyances bother you less:
- Endless med rec, disposition, and multi-morbidity juggling (IM), or
- Repeatedly delivering bad news and living with uncertain, often irreversible outcomes (Neuro)?
Then look at realistic job options, not just the “ideal” version you have in your head. Talk to attendings who are 5–10 years out, not just residents.
5. What is the single biggest burnout mistake applicants make with IM and neuro?
They assume that interest in the subject matter automatically translates to tolerable daily life. Loving pathophysiology does not mean you will love 20 MyChart messages about dizziness. Enjoying stroke localization does not mean you can emotionally absorb nightly conversations about devastating deficits. Ignoring the lived, hour-by-hour reality of these specialties is the core mistake that breeds burnout.
Key points to walk away with:
- Do not confuse “flexible specialty” or “academic prestige” with a humane, sustainable daily life.
- Pay attention to how you actually feel on IM and neurology rotations; your real reactions are your best burnout predictor.
- Ask hard, specific questions about call, documentation, and culture, and be willing to walk away from shiny programs that clearly run on resident and junior faculty sacrifice.




















