The first 72 hours after a disabling diagnosis are not for “being strong.” They are for building a survival plan.
Most people waste those first days in shock, vague Googling, and half-remembered phone calls. Then, three weeks later, they discover they missed crucial forms, deadlines, or workplace steps that would have protected them. I have watched that play out more times than I care to count.
Let’s not do that.
You have 72 hours to set a foundation: medically, legally, financially, and practically. I am going to walk you through those three days—hour by hour in broad blocks, with concrete checklists. You will not fix your life in 72 hours. You will create a structure so your life is fixable.
Hour 0–4: Right After the Diagnosis
At this point you should do almost nothing external. Your brain is flooded. Use this window to capture information, not to make big decisions.
Step 1: Lock down the medical facts (before you forget)
Right after the appointment or as soon as you get home:
Write down exactly what you were told.
Bullet points. No essays. Include:- Name of the diagnosis (exact spelling)
- Stage/severity (if applicable)
- What the doctor said about prognosis (temporary, progressive, permanent, uncertain)
- Medications started or changed
- Follow-up tests or imaging ordered
Get immediate access to your medical records portal.
- Make sure you can log in to MyChart or whatever system they use.
- Confirm your email and phone are correct.
- If they gave you visit summaries or handouts, take photos or scans and put them in one folder on your phone/computer labeled:
DX-Day1.
Record clarifying questions while they are fresh.
Examples:- “How will this affect my ability to work?”
- “What symptoms mean I should go to the ER?”
- “Is this likely to get worse quickly or slowly?” You are not answering them now. You are parking them for the follow-up.
Step 2: Create a “critical info” document
Open a note on your phone or a single piece of paper. At the top, write:
- Diagnosis:
- Date diagnosed:
- Treating clinician + contact:
- Current meds:
- Next appointment date/time:
This becomes your anchor. You will use it constantly—for forms, work emails, family talk, everything.
Hour 4–12: Stabilize Yourself and Your Immediate Safety
You are still on Day 1. At this point you should focus on two things: your body and your immediate safety.
Step 3: Stabilize basic physical needs (yes, really)
Shock makes people do dumb things—like skip food, overmedicate, or drive when they should not.
In the first 12 hours:
- Eat something with protein and carbs. You need stable blood sugar to think.
- Hydrate. Especially if pain, dizziness, or meds are involved.
- Check your meds.
- Confirm what you are supposed to start, stop, or change.
- Set alarms on your phone for any new dosing schedule.
If your diagnosis affects consciousness, mobility, or cardiac/respiratory function (stroke, seizure disorder, severe heart failure, advanced lung disease, etc.):
- Identify a “watcher” for the first night.
Someone who:- Knows your condition
- Knows when to call 911
- Has your medication list and doctor’s number
Step 4: Decide your driving and work status for the next 24–48 hours
Do this early. Do not wait for a crisis.
Driving
Ask yourself bluntly:- Did the doctor say “Do not drive” (for seizures, syncope, vision loss, etc.)?
- Are you on new meds causing sedation, dizziness, or confusion?
If yes or even “I’m not sure”:
- Call or message the clinic: “I was just started on X and diagnosed with Y. Am I safe to drive?”
- Until clearly told otherwise, assume no. Arrange rides or delivery.
Work for the next 1–2 days
If you are employed or in school, send a short, controlled message. No oversharing.Example email to supervisor (Day 1):
I had an urgent medical evaluation today and received a new diagnosis. My physician has recommended that I take the next 1–2 days to stabilize treatment and follow up.
I will be out on [date(s)] and will provide an update once I have more detailed guidance from my healthcare team.
This buys you time without locking you into long-term statements.
Day 2 (Hours 12–36): Build Your Medical and Legal Base
You have made it through the shock window. Day 2 is for structure. At this point you should focus on:
- Clarifying your medical plan
- Documenting functional impact
- Starting the disability/accommodations trail
Step 5: Clarify the next 30 days medically
Use your questions list from Day 1.
If you already have a follow-up appointment scheduled in the next 1–2 weeks:
- Send a message through the portal with 3–5 focused questions:
- “What should I avoid doing until I see you again?”
- “Are there red flag symptoms that should send me to the ER?”
- “Do I need any work or school restrictions documented now?”
- “Is this condition expected to be stable, or could it worsen quickly?”
- Confirm your medication list and doses in that same message. Ask:
“Can you confirm my current medication list and doses are correct in my chart?”
If you do not have a follow-up appointment:
Call the office before 10:00 a.m. on Day 2.
Script:
I was just diagnosed with [condition] yesterday with [clinician name]. I need a follow-up appointment within the next [time frame they mentioned] and I need to discuss work/school restrictions and documentation. What is your earliest available slot?
A lot of patients mumble “whenever is fine.” It is not. Say the words “work/school restrictions” or “disability paperwork.” Schedulers move faster when they hear those.
Step 6: Document how this diagnosis actually disables you
Diagnosis alone rarely drives accommodations. Function does. Start capturing it now.
On Day 2, use a simple structure:
- Physical function
- Walking/standing: “Can walk 5 minutes with cane, then need to sit.”
- Lifting: “Cannot safely lift more than 10–15 lbs.”
- Fine motor: “Typing causes severe pain after 10 minutes.”
- Cognitive function
- Concentration: “Can focus about 15–20 minutes before mental fatigue.”
- Memory: “Forget instructions unless written down.”
- Sensory
- Vision: “Cannot read standard print more than 5–10 minutes.”
- Hearing: “Need amplified sound / cannot follow group conversations.”
- Time-related
- “Need 1–2 rest breaks of 15–20 minutes in a 4-hour period.”
You are not exaggerating; you are describing your worst typical day, not your best one. This text will become the backbone of future forms, letters, and accommodation requests.
Day 2 Afternoon: Start the Disability Accommodations Track
At this point you should open channels, not necessarily file full applications yet. You are setting up the dominoes.
| Context | Who to Contact First | Typical Title/Office |
|---|---|---|
| Workplace | HR or direct supervisor | HR, People Operations |
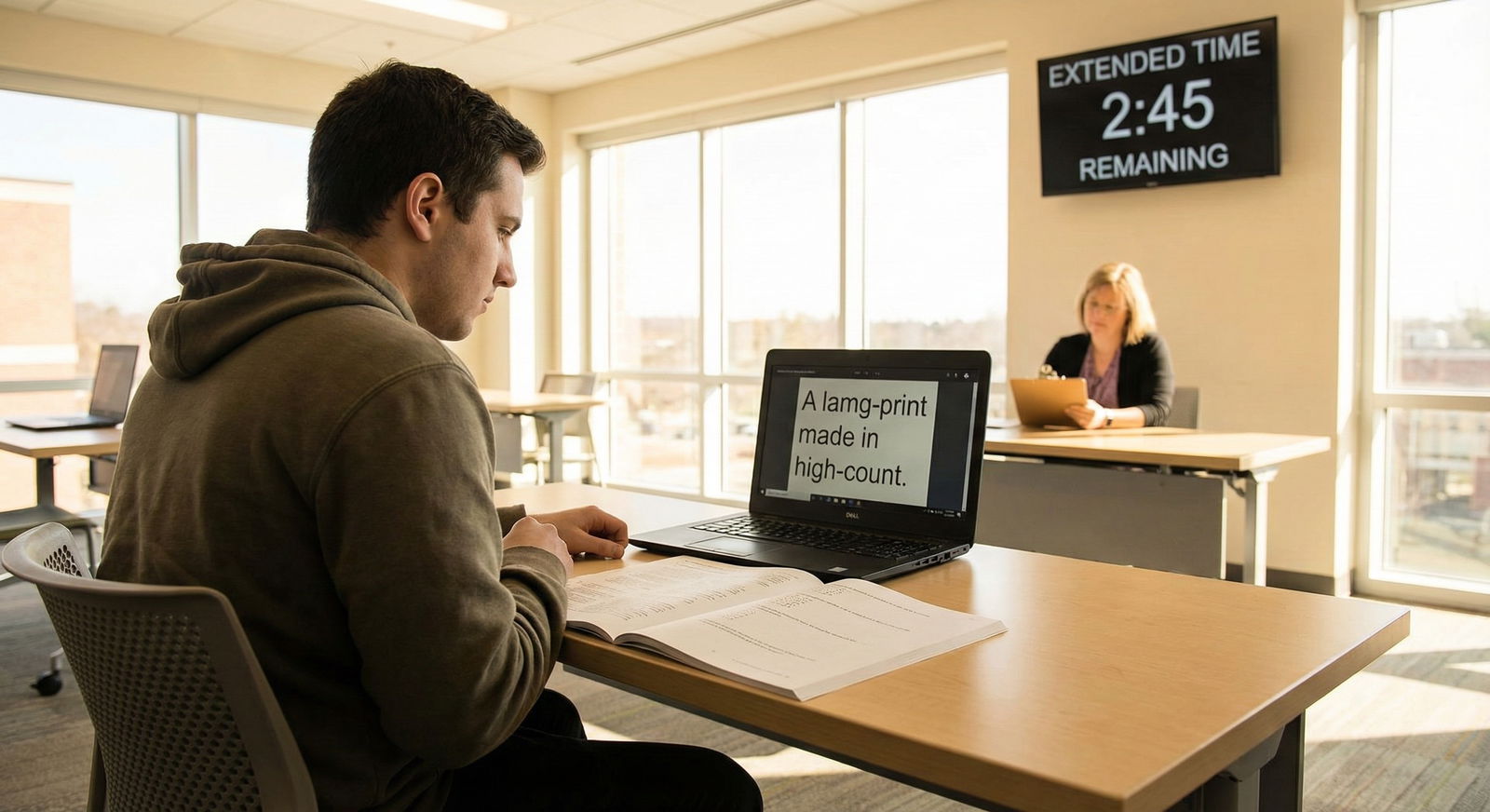
| University | Disability/Accessibility Svcs | Office of Disability Svcs |
| K–12 school | School counselor | Special Education / 504 |
| Government aid | State disability office | Vocational Rehabilitation |
| Legal advice | Disability rights org | Legal Aid / Advocacy Group |
Step 7: First contact with work or school (not a full disclosure yet)
If you are employed:
By the end of Day 2, you should:
Identify your HR / benefits portal.
Send a controlled email to HR (not a casual Slack DM) if your condition may limit your job:
I was recently diagnosed with a medical condition that may affect some aspects of my work. I am exploring whether workplace accommodations might be appropriate.
Could you please let me know the process for requesting accommodations under the ADA and who I should speak with?
That phrase “process for requesting accommodations under the ADA” does two things:
- Signals this is a legal category, not a favor.
- Gets you routed to the right person or form.
If you are a student:
Email your disability / accessibility office:
I have received a new disabling medical diagnosis and anticipate needing academic accommodations.
Could you please share your documentation requirements and the process for setting up an intake meeting?
You do not need your full letter from your doctor yet. You are simply starting the clock and learning what paperwork they will need.
Day 2 Evening: Build Your Information Guardrails
The temptation is to spend all night on the internet. That is how people end up convinced they will be dead in 6 months based on a 2003 forum post.
Step 8: Set strict research limits and choose sources
Make a rule: no more than 60–90 minutes of online research per day in the first week.
Then:
Identify 2–3 credible sources:
- Major hospitals (Mayo Clinic, Cleveland Clinic, academic centers)
- National specialty organizations (e.g., National MS Society, American Diabetes Association)
- Government sites (NIH, CDC where applicable)
Write down:
- Which subtypes or stages apply to you
- Which treatments are standard first-line care
- Any phrases you do not understand for your list of questions
What you avoid:
- Reddit diagnosis horror stories
- Random blogs promising miracle cures
- Anyone selling a “protocol” that cures everything
Day 3 (Hours 36–72): Turn to Logistics and Next Steps
By Day 3, shock has started to ebb. Now you build practical scaffolding: money, documentation, and support.
Step 9: Do a 30-minute financial snapshot
You are not rebuilding your budget today. You are getting a map.
In a single sitting:
List your current income sources:
- Job wages
- Partner/spouse income
- Stipends, scholarships
- Existing benefits (VA, SSDI, etc.)
List non-negotiable monthly expenses:
- Housing
- Utilities
- Food (rough number)
- Medications / copays you already know
Identify fragile points:
- “If I miss more than X weeks of work, I cannot pay rent.”
- “I do not know if my insurance will cover this treatment.”
Pull your insurance card and create a note with:
- Insurer name
- Member ID
- Customer service number
- Pharmacy benefits manager (if separate)
Your goal: by the end of this 30 minutes, you know where a crisis would hit. That informs your next calls.
Step 10: Call your insurance about the diagnosis (yes, this early)
Do this on Day 3, during business hours. Use a script and take notes.
Questions to ask:
- “My new diagnosis is [name]. Can you confirm that [major medication/test/therapy] is covered under my plan?”
- “Do I need prior authorization for any of the treatments my doctor mentioned?”
- “Is there a case manager or care coordinator available for complex conditions?”
- “What is my out-of-pocket maximum for the year?”
If they offer a case manager, accept. It is one of the few actually helpful insurance services when used well.
Day 3 Midday: Prepare for Work/School Documentation
At this point you should convert your functional notes into something your clinician and HR or disability office can use.
Step 11: Draft your “functional limitations” summary
Using what you wrote on Day 2, tighten it into 1–2 short paragraphs plus bullets.
Example:
Due to [diagnosis], I experience significant limitations in walking, standing, and concentration. On a typical day:
- I can walk about 5 minutes with a cane before needing to sit.
- Standing in one place more than 3–5 minutes causes severe pain and dizziness.
- I can concentrate on cognitively demanding tasks for about 20 minutes before needing a short break.
- Fatigue worsens over the course of the day; mornings are typically better than afternoons.
You will share this with:
- Your clinician (to help them write accurate work/school notes)
- HR / disability services (once formal processes start)
Step 12: Ask your clinician for an initial work/school note
Do not wait until you are in crisis.
Send a message through the portal:
I am starting the process of discussing accommodations with my [employer/school].
Could you please provide an initial note that:
- Confirms I have a medical condition affecting [mobility/energy/vision/etc.], and
- Recommends temporary restrictions (for example: reduced hours, no heavy lifting, ability to sit as needed, flexible deadlines)?
I have attached a brief description of my current functional limitations to help guide this.
Attach or paste your functional summary. You are making your clinician’s job easier. That usually speeds everything up.
Day 3 Afternoon: Set Up Your “Support Grid”
You cannot carry this alone. But you also cannot have 15 people texting “How can I help?” and no system.
Step 13: Choose 1–2 point people
Select:
One primary medical admin person (spouse, parent, close friend) who can:
- Help with rides to appointments
- Sit in on important visits
- Track questions and notes
One logistics person who can:
- Help with forms, deadlines, and mail
- Keep track of applications (FMLA, disability, accommodations)
If it is the same person, fine. What matters is clarity.
Give them:
- Your diagnosis name
- Your main clinician’s name and contact
- A short explanation of how it affects daily function
- Clear permission levels (what they can and cannot access or share)
Step 14: Create a basic appointment and document system
Nothing fancy. Just consistent.
Minimum viable system:
- Digital folder structure (on your computer or cloud drive):
Disability/MedicalVisit SummariesLabs & ImagingWork-School NotesForms & Applications
- One running document titled:
Questions for Doctor – [Name]- Add date-stamped bullet lists leading up to each visit.
- Calendar entries for:
- All appointments
- Any known deadlines (FMLA forms, insurance paperwork, school accommodation reviews)
This is tedious. It will save you dozens of hours later.
Day 3 Evening (Hours 60–72): Decide the Next 2–4 Weeks
At this point you should stop obsessing over the rest of your life and define an interim plan.
Step 15: Make a 2–4 week “holding plan”
Take 20–30 minutes and write down, for the next 2–4 weeks:
Medical priorities
- Follow-up visit(s) scheduled?
- Any tests you need to schedule?
- Symptoms you are tracking (pain, fatigue, seizures, blood sugar, etc.) with a simple log.
Work/school priorities
- Are you working normal hours, reduced, or out temporarily while you figure this out?
- What deadlines need to be moved or delegated this month?
- When will you meet formally with HR or disability services?
Energy conservation rules Examples:
- 1 major task per day (appointment or work meeting, not both).
- No back-to-back days of heavy exertion.
- Set a hard stop in the evening to protect sleep.
Support check-ins
- Who will you update weekly?
- When will you review finances again (not daily—weekly is enough for now)?
You are not carving your future into stone. You are giving your brain a smaller, defined container so it can stop spinning.
Visual: 72-Hour Timeline Overview

| Period | Event |
|---|---|
| Day 1 (0-24h) - Hour 0-4 | Capture diagnosis details, create critical info doc |
| Day 1 (0-24h) - Hour 4-12 | Stabilize safety, food, meds, decide driving/work status |
| Day 2 (24-48h) - Morning | Clarify follow-up care, document function |
| Day 2 (24-48h) - Afternoon | Contact HR or disability office, set research limits |
| Day 2 (24-48h) - Evening | Organize medical info, plan questions |
| Day 3 (48-72h) - Morning | Financial snapshot, call insurance |
| Day 3 (48-72h) - Midday | Draft functional summary, request work/school note |
| Day 3 (48-72h) - Afternoon/Evening | Set support grid, 2-4 week holding plan |
Common Pitfalls in the First 72 Hours
You will be tempted by a few bad moves. Avoid them.

| Category | Value |
|---|---|
| Endless Googling | 80 |
| No HR/School Contact | 70 |
| Ignoring Finances | 60 |
| Not Documenting Function | 75 |
| Driving Unsafely | 90 |
Briefly:
Endless Googling
Consumes hours, raises panic, produces zero actionable steps.Radio silence with work or school
Then you show up 3 weeks later asking for major changes with no paper trail. That is how accommodations get delayed or denied.Ignoring finances
Denial feels better, until a bill hits or you cannot work and have no plan.Not documenting function
Later, when a form asks “Describe how your condition limits your daily activities,” you stare at a blank page under deadline.Driving when you should not
This one is non-negotiable. If your diagnosis affects consciousness, vision, or balance, you clarify driving status with a clinician. Or you do not drive.
The Bottom Line in Three Moves
Over these 72 hours, your job is not to be heroic. It is to be methodical.
- Capture and clarify: Get the diagnosis facts, follow-up plan, and functional impact written down in plain language.
- Open the right channels: Contact your clinician, HR or disability office, and insurance—not with your life story, but with specific process questions and initial documentation requests.
- Build a short-term structure: Set up basic files, support people, and a 2–4 week holding plan so you can respond to this diagnosis instead of just reacting to it.
You cannot control the diagnosis. You can absolutely control how organized the next 72 hours are. That difference compounds over the months that follow.



















