It’s 10:45 p.m. You were supposed to sign out at 7. Everyone else from your call team is gone. You’re still in the workroom finishing three discharge summaries, two appeal letters, and a pile of orders that somehow “became yours.”
The senior just said, “Thanks so much, you’re a lifesaver,” as they walked out. You’re not feeling like a lifesaver. You’re feeling like a doormat. And you’re starting to wonder: Is everyone doing this much? Or am I getting dumped on?
You’re in your first year as an intern. You don’t fully know what’s “normal” yet. You don’t want to be labeled lazy, unprofessional, or “not a team player.” But something about this pattern feels off.
Let’s treat this like what it is: a situation with real risks—burnout, resentment, mistakes, bad evaluations—but also real levers you can pull.
Here’s how to handle it.
Step 1: Figure Out If You’re Actually Being Singled Out
Before you confront anyone or spiral mentally, you need data. Not vibes. Data.
Spot the patterns
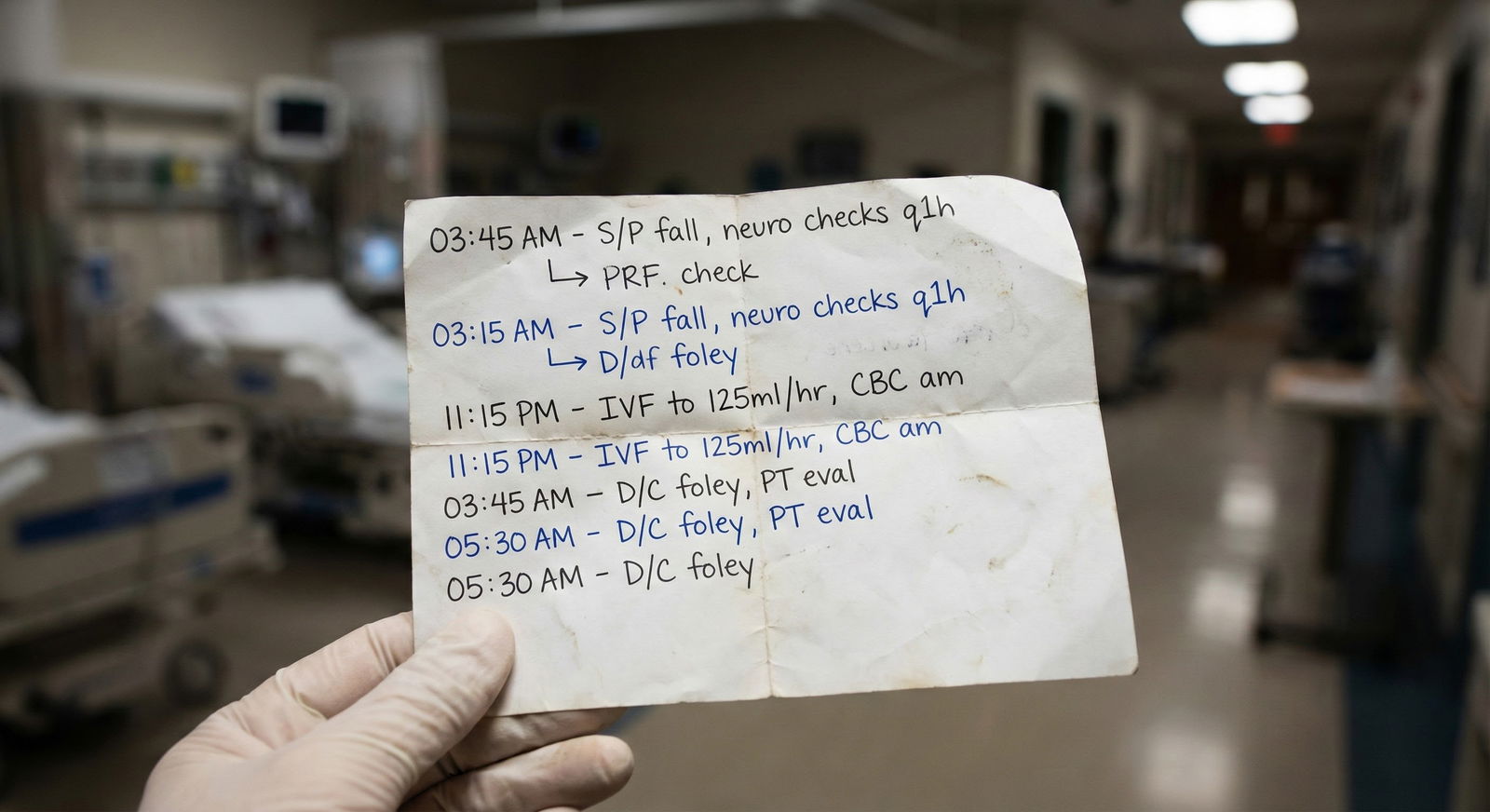
For the next 1–2 weeks, track your workload. Literally write it down or log it on your phone.
Track things like:
- How many patients you’re carrying vs. co-interns
- Who did discharges, cross-cover calls, procedures, notes, admits, consults
- When you arrived and when you left
- How often you’re the one who “just helps out” on everyone else’s tasks
You’re looking for patterns over time, not one bad shift.

| Category | Value |
|---|---|
| You | 3 |
| Co-intern A | 7 |
| Co-intern B | 6 |
| Co-intern C | 6 |
(Where 1 = “unfairly heavy” and 10 = “very fair/comfortable” as you honestly perceive it.)
I’ve seen this repeatedly: when interns actually track their work, one of two things happens:
- They confirm they’re clearly doing more, or
- They realize they’re doing a different type of work—less glamorous grunt work—and it feels like more even if the raw numbers are similar.
Both matter. But the solution is slightly different.
Ask one trusted co-intern
Pick one person who seems reasonably fair and not gossipy. Something like:
“Hey, I’m trying to sanity-check my sense of workload. This is my first year and I honestly don’t know what’s normal. Does it seem like I’m carrying about the same load as you, or am I off?”
Avoid: “Do you think Dr. X is dumping on me?” That drags them into drama. You want a read on the workload, not a coalition.
If they say, “Yeah, you always seem to have the sickest or most patients,” that’s signal.
If they say, “We’re all dying,” that’s a different problem—systemic, not personal targeting.
Step 2: Separate Three Different Problems
“Unfair workload” is usually a mix of:
- Systems issue (bad staffing / bad design)
- Culture issue (toxic team norms, blame, hierarchy abuse)
- You issue (you take on everything, don’t set boundaries, or work slower because you’re new)
You need to be honest which ones are in play.
Systems issue
Clues:
- Everyone’s staying late, every day
- Different interns on different teams all say the same thing
- The cap is technically 10 patients but everyone has 15–18 “because nights is swamped”
- There’s chronic nursing/ancillary understaffing and residents are plugging gaps
You being overworked here isn’t personal. You’re in a broken system. That changes your strategy.
Culture issue
Clues:
- One attending or senior consistently gives you scut and “protects” favorites
- You get comments like “You’re fast, you don’t mind doing a few extra, right?”—every day
- When something unpleasant comes up (discharge summaries, appeals, placement paperwork), eyes drift to you
- You’re doing non-educational work while others get procedures, family meetings, teaching time
This is where “targeted” usually lives.
You issue (skill + boundaries)
This part stings, but you have to rule it out:
- You say “yes” before anyone else speaks up
- You don’t push back when work gets shifted to you
- You’re slower with notes/orders, so you end up being the last one around—and people keep handing you “quick favors”
- You over-explain everything and double/triple check non-critical stuff, burning time
Some of this is normal intern growth. Some of it is controllable. And if you fix your piece, the targeted feeling often eases.
Step 3: Fix What’s In Your Control First (Quietly)
Before you go to war with a senior or attending, tighten up your own game. Not because it’s “your fault,” but because it gives you leverage and credibility.
Get faster and more focused
Pick one weak point:
- Notes taking forever? Build and refine templates. Ask a strong senior: “Can I see your note template?”
- Orders delayed because you’re anxious? Prioritize: safety-critical orders first (antibiotics, insulin, anticoag, fluids), fluff later.
- You do everything perfectly but slowly? Drop perfectionism where it doesn’t matter. A social note doesn’t need literary flair.
Time yourself: “How long did that H&P actually take?” Then try to shave 5–10 minutes without sacrificing safety.
Stop auto-volunteering
If you’re the one saying “I can do it” before silence even lands, you’re training the team to dump on you.
Try this:
- When a task is floated (“Someone needs to do these three discharges”), pause for 3–5 seconds.
- Let someone else speak up. Do not reflexively volunteer.
- If no one volunteers and it truly has to be done, negotiate:
“I can take one of them if someone else can grab the other two—I’ve still got three new admits to finish.”
Small, calm, firm.
Use neutral, boundary-setting language
You don’t need to be dramatic. You just need to stop accepting an infinite pile.
Examples on the fly:
- “I can do that, but I won’t be able to finish X before sign-out. Which is higher priority?”
- “I’m at capacity with four active issues on my list. Can we redistribute or adjust expectations?”
- “I can take that on next, but right now I need to get these stat orders in safely.”
You’re not refusing. You’re forcing your senior to make a decision instead of mindlessly stacking more on your plate.
Step 4: When It Is Targeted – Address It Up the Chain
Let’s say you’ve tracked the workload. You’ve tightened your own efficiency. You’re not auto-volunteering. And you still consistently end up with the worst load.
Now you escalate.
Start with your senior (if they’re part of the problem)
Pick a neutral time. Not during a code, not when they’re buried.
Something like:
“Can I run something by you? I’ve noticed over the last week or two that I’ve been carrying more patients and a lot of the discharges / extra paperwork. I’m totally happy to work hard, I just want to make sure I’m not misunderstanding expectations or falling behind in other learning opportunities.”
You’re signaling:
- I’ve noticed a pattern
- I’m not accusing
- I care about education and fairness
If you feel brave and it’s really clear:
“On Tuesday, I had 14 patients while the others had 9–10. Yesterday I did all four discharges. I’m starting to feel stretched to where I’m worried about missing things. How can we make the workload more balanced?”
Concrete numbers make it hard to gaslight you.
If the senior blows you off
You’ll hear some version of:
- “We’re all suffering, it’s intern year”
- “It’ll make you stronger”
- “Everyone thinks they’re doing the most”
If they truly won’t budge and the pattern continues, next step is your chief or program leadership.
Step 5: Use Chiefs and Program Leadership Strategically
You are not “weak” for looping in chiefs or the program director. They exist exactly for crap like this. The trick is doing it smartly.
Go to chiefs first if possible
They’re closer to the ground and less likely to trigger nuclear drama. Email or message:
“Hey, do you have a few minutes this week to discuss workload balance on [service X]? I’m not sure if what I’m experiencing is standard for the rotation, and I’d appreciate your perspective.”
When you meet, be specific and calm:
- “Over the last 10 shifts, my average census has been ~14 vs 9–11 for my co-interns.”
- “Disproportionate share of non-educational tasks is falling to me.”
- “I’ve already tried optimizing my efficiency and talking briefly with my senior.”
Your ask is not “please yell at them.” Your ask is:
- “Is this normal for this rotation?”
- “If not, how do you suggest I handle it?”
- “Can you help reinforce expectations about fair workload distribution?”
When it’s bad enough for PD-level involvement
Examples:
- One attending regularly singles you out for demeaning comments + extra work
- Retaliation after you raised concerns
- Patient safety is getting compromised because of the overload
Then you set up a meeting with the APD/PD:
“I’d like to discuss some concerns I have about workload distribution and safety on [service]. I’ve tried resolving it at the team level and with the chiefs, but I’m still concerned.”
Again, show you’ve tried steps 1–3 before step 10.
Step 6: Protect Your Evaluations and Your Sanity
You’re not just protecting your time. You’re protecting your reputation and mental health.
Document, briefly and privately
You don’t need a novel. But a simple running log saved somewhere private (not hospital email) helps:
- Date / shift
- Your census vs co-interns
- Major extra tasks clearly dumped on you
- Any conversations you had with seniors / attendings about it
If your evaluation later says “struggles with workload” or “difficulty managing tasks,” you’ve got receipts and context.
Be visibly professional, not visibly bitter
Unfairness makes people snappy. That’s how they get dinged.
You can be firm without eye-rolling, sarcasm, or passive-aggressive comments in front of nurses or attendings.
Examples of assertive but professional phrases:
- “Given my current list, I’m worried about being able to do that safely without dropping something important.”
- “Can we redistribute a bit so we’re all getting home at a reasonable time?”
- “I’m not refusing—I’m saying I need help prioritizing.”
What you want faculty to think:
“Hard worker. Advocates appropriately. A bit overloaded.”
Not:
“Complains constantly. Difficult.”
Step 7: Decide When to Just Survive the Rotation
Sometimes the honest answer is: this month is garbage, the culture won’t change in four weeks, and your best strategy is to mitigate harm, not fix the system.
You may be here if:
- You’re at the tail end of a malignant rotation with entrenched norms
- The power dynamics are bad and leadership is complicit
- You’ve already spoken up and got nowhere, and you don’t want to die on this particular hill
In that case, your approach shifts:
- Strip your work to safe, necessary tasks. No heroics, no extras “just to be nice.”
- Leave on time when your work is done. Don’t linger to pick up random extras just to feel helpful.
- Use off days to actually rest, not catch up on more prep for this same toxic environment.
- Debrief with someone outside the program (therapist, friend, partner) so you don’t normalize abuse.
You’re not weak for choosing survival over crusading.
Step 8: Long Game – Don’t Let This Shape Your Entire Identity as a Doctor
Unfair workloads, bad seniors, malignant rotations—these are all real. But they’re also phases. You don’t want to internalize:
- “I’m the person who always has to say yes.”
- “If I ever set boundaries, I’m a problem.”
- “Medicine = constant exploitation.”
You want to come out of this with:
- Clearer sense of your limits
- Better time-management and efficiency
- Experience advocating for yourself without starting fires
- Radar for truly malignant environments you’ll avoid later
If you ever become a senior or attending (you will), remember this. Don’t turn into the person who says “We all went through it, you’ll be fine.” That line is lazy and cowardly.
Concrete Scripts for Common Scenarios
You’re tired. Let me give you actual words you can use.
Scenario 1: Senior keeps dumping discharges on you
Senior: “We’ve got four discharges. You can take all of them, right?”
You:
“I can definitely take one or two, but with my current list and two new consults, I won’t be able to safely manage all four. Can we split them up so I’m not missing things on my other patients?”
If they insist:
“I’m uncomfortable with that from a safety perspective. Can we ask the attending how they’d like us to prioritize?”
Now the attending is looped in. Sometimes that’s enough to rebalance things.
Scenario 2: Co-intern frequently shifts work to you
Co-intern: “Hey, can you just do my cross-cover checks tonight? I have to leave right at 7 for something important.”
You:
“I’ve got my own cross-cover load, so I can’t safely take on yours as well. If there’s one urgent thing, I can help with that, but your general list needs to be covered by you or the senior.”
You’re allowed to say no to being their personal safety net.
Scenario 3: Attending piles on “just one more thing” repeatedly
Attending: “Can you also call the family for a long goals-of-care discussion this afternoon?”
You (already slammed):
“I’m happy to be part of that, but with my current workload I probably can’t lead a full hour-long meeting today. Would it work if I join you or the senior for part of it, and I can help with documentation?”
You’re signaling: I’m not lazy, I’m limited.
| Situation | First Contact | Next Step If Unresolved | Documentation Needed? |
|---|---|---|---|
| Slightly heavier load than peers | Senior | Chief resident | Helpful but not vital |
| Clear pattern of targeted extra work | Senior | Chief then APD/PD | Yes |
| System-wide overload affecting everyone | Chief | APD/PD | Yes, for safety issues |
| Retaliation after raising concerns | Chief or PD | GME/HR if severe | Absolutely |

| Step | Description |
|---|---|
| Step 1 | Notice pattern of extra work |
| Step 2 | Track workload 1 to 2 weeks |
| Step 3 | Improve efficiency and boundaries |
| Step 4 | Discuss with senior |
| Step 5 | Continue and monitor |
| Step 6 | Meet with chief resident |
| Step 7 | Meet with APD or PD |
| Step 8 | Personal issue or systemic? |
| Step 9 | Improved? |
| Step 10 | Still unsafe or unfair? |

FAQs
1. What if my co-interns say they’re also overwhelmed—does that mean I’m not being targeted?
Not automatically. It might mean the whole system is overloaded and you’re getting the worst of it. That’s why you need specifics: average census, types of tasks, length of stay. If all of you are drowning equally, that’s a systems problem you and your co-interns should bring to chiefs together. If you’re consistently carrying more or doing more non-educational scut, that’s layered on top.
2. Will speaking up hurt my evaluations or reputation?
It can, if you come in hot, emotional, or blaming. It usually does not when you’re specific, calm, and focused on safety and fairness. Frame it as: “I want to provide safe care and get the same educational experiences as my peers.” Also, programs generally know who their problem seniors/attendings are. If three interns in a row say the same thing, you’re not the problem; you’re the data point.
3. How do I know when something is bad enough to report formally?
Use this mental checklist:
- Are patients potentially less safe because of the workload?
- Has the pattern persisted for >1–2 weeks despite you adjusting your own approach?
- Have you already tried at least one conversation with your immediate senior?
If the answer is yes to these, that’s not just “intern pain.” That’s something chiefs or leadership should hear about.
4. What if I’m just slower than everyone else and that’s why I feel overloaded?
Then your main job is skill-building, not fighting. Honestly ask: “If someone else had my exact list, would they be drowning too?” If the answer is no, ask a strong co-intern or senior to shadow you for an hour and critique your workflow. Most efficiency problems are fixable: not batching tasks, not pre-charting, writing novels instead of notes, re-checking non-critical labs obsessively. Fixing those won’t just make you feel better now; it’ll make every future year easier.
Key takeaways:
- Don’t trust your frustration alone—track actual workload and patterns.
- Fix what’s in your control (efficiency, boundaries) while calmly pushing back on clearly unfair distribution.
- When patterns persist or impact safety, loop in chiefs and leadership strategically, and protect your own evaluations with brief documentation and professional behavior.



















