The last month of PGY1 will expose every crack in your system. That’s exactly why it’s the best time to fix them before you’re the senior everyone else depends on.
You are not “almost done.” You’re in the transition zone. The decisions you make in this final month will determine whether PGY2 feels like a controlled step up or a chaotic free‑fall.
Let’s walk it chronologically—month, week, then day. I’ll tell you what to do, and when.
The Final Month: Big-Picture Priorities
At this point you should stop thinking like “the intern who survives” and start acting like “the junior who runs things.”
During this last month, your priorities are:
- Tighten your clinical workload systems
- Reflect honestly on PGY1—what worked, what didn’t
- Prepare mentally and practically to be the senior
Think of this month in three overlapping tracks:
- Workload – How you handle notes, orders, cross-cover, admissions.
- Reflection – What you actually learned, what you didn’t, what still scares you.
- Preparation – Concrete planning for senior responsibilities, scheduling, and leadership.

| Period | Event |
|---|---|
| Early Month - Weeks 1-2 | Systems tune up, feedback, gap spotting |
| Mid Month - Weeks 3-4 | Senior shadowing, leadership practice, handoff planning |
| End of PGY1 - Final 7 days | Consolidation, formal reflections, transition checklist |
Weeks 4–3 Before PGY2: Stabilize the Workload
At this point you should treat your current rotation as a test environment for next year’s systems. You’re not just “getting through the block” anymore. You’re stress‑testing how you’ll function as a senior.
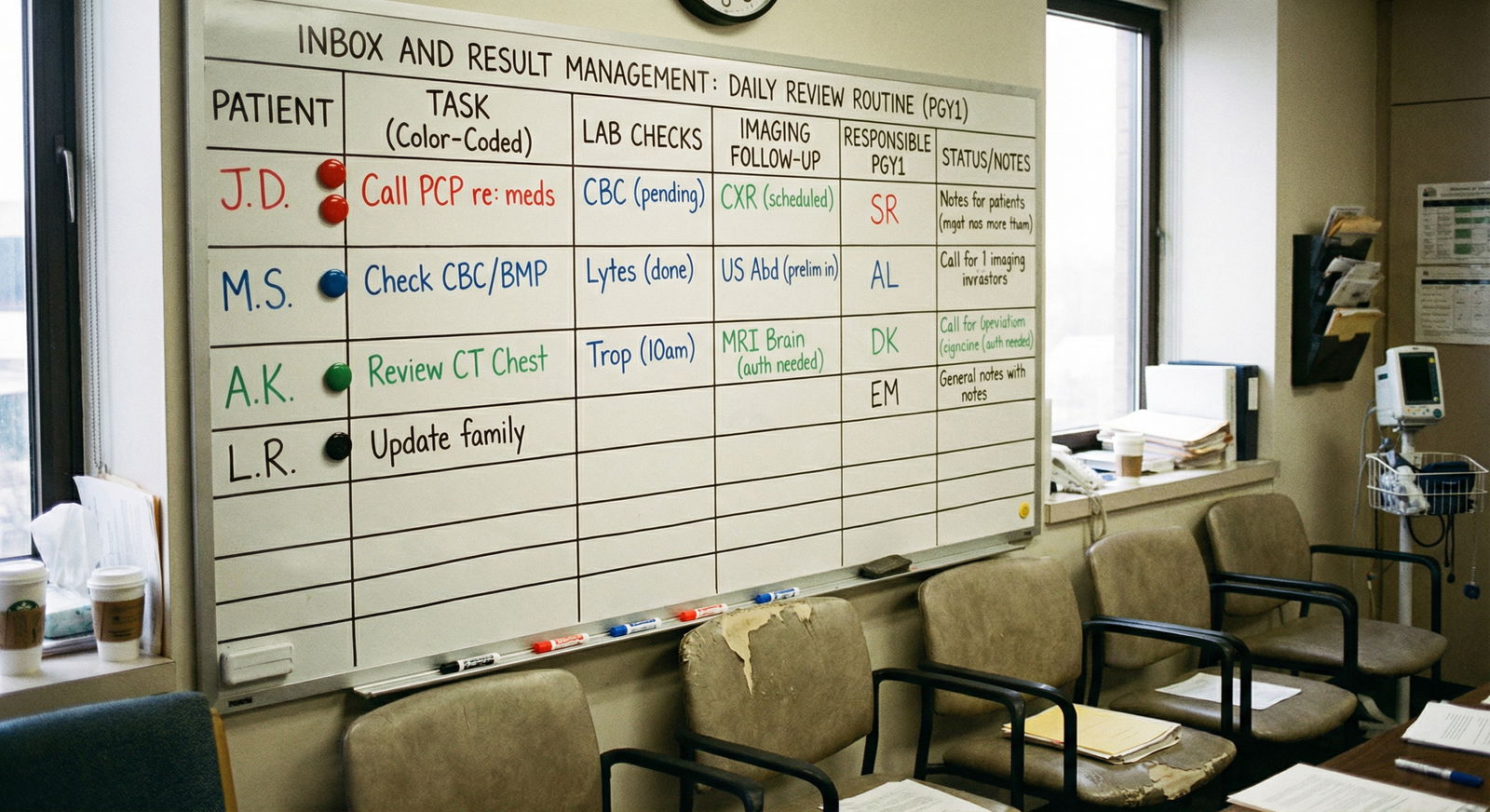
1. Standardize Your Daily Workflow
If your day still feels random, that’s the first problem to fix.
By now you should:
- Start every day with the same 5–10 minute pre-round routine
- Have a consistent way you pre-chart
- Use templates or smart phrases that actually save time
At this point you should clean up your workflow:
Pre-rounding
- Decide a fixed order: vitals → I/Os → overnight events → new labs/imaging → focused exam
- Create a 1‑line summary for each patient in your head (or in a tiny note): “60M, CHF exacerbation, diuresis day 2, Cr trending up slightly.”
Notes
- Standardize note skeletons by service (medicine, surgery, ICU, ED).
- Stop rewriting full histories. Summarize: “Admitted for X on day Y; hospital course notable for A, B, C.”
Communication
- Set time blocks where you expect peak interruptions (early AM labs, 8–10am order clarifications, 4–6pm dispo chaos) and front-load your critical work before those windows.
If you don’t have these routines down now, PGY2 will hurt. Fix them here.
2. Audit Your Clinical Gaps
Everyone finishes PGY1 with holes. The dangerous ones are the holes you’re not aware of.
This month, at this point you should:
Make a quick list of “still uncomfortable with” topics:
- Chest pain that’s not obvious STEMI
- Borderline sepsis
- Non-invasive ventilation decisions
- New atrial fibrillation with RVR
- Post-op patients with borderline vitals
Pick 1–2 gaps per week and:
- Look up 1–2 solid review articles or an UpToDate summary
- Ask a senior or attending: “Can I run a quick case with you on X? I don’t feel strong on it.”
Do not wait for PGY2 to “force” you to learn this on the fly while a junior asks, “What do you want to do?” and you have no idea.
3. Start Acting Like the Senior for Small Things
You’re not officially the senior yet. But you can start working like one in bite‑sized chunks.
This week you should:
Volunteer to:
- Run part of table rounds: “I can lead through the cross-cover patients.”
- Teach a new intern or student 1 practical topic: “Admission orders for DKA,” “Basic insulin regimens,” “Hyponatremia basics.”
Practice decision‑making:
- When you call the senior, start with: “I think this is X. I’m considering doing Y or Z. I’m leaning toward Y because…”
- That framing is exactly what you’ll expect from your juniors next year.

| Category | Value |
|---|---|
| Clinical Workload | 55 |
| Reflection & Feedback | 15 |
| Senior Prep & Teaching | 20 |
| Admin & Logistics | 10 |
You’re training your brain to stop being purely reactive and start planning ahead.
Weeks 2–1 Before PGY2: Structured Reflection and Senior Prep
Now we shift from “fixing present problems” to “engineering the next year.”
At this point you should be doing deliberate reflection, not vague “I guess I learned a lot” thinking.
4. Do a Ruthless PGY1 Self-Review
Don’t wait for the semi‑useless official evaluation. Do your own.
This week you should set aside one uninterrupted hour (yes, actually schedule it) and write:
Three things you do well now that you couldn’t do in July
Example:- Comfortably run a basic sepsis workup and initial resuscitation
- Communicate with consultants efficiently
- Break bad news without stumbling
Three things that still feel shaky
- Example: “I still panic a bit when I see BP 80/40.”
- “I don’t like managing complex anticoagulation.”
- “I lose control of my time when I have more than 10 patients.”
Three habits that need to die before senior year
- Procrastinating on discharges
- Letting your notes balloon to novels
- Not asking for clarification when you don’t understand the attending’s plan
Write this down. This becomes your PGY2 improvement roadmap.
5. Get Explicit Feedback from People Who Know
At this point you should stop guessing how others see you. Ask directly.
Target:
- 1–2 seniors who supervised you multiple times
- 1 attending who’s seen you across at least a full rotation
- 1 nurse you work closely with (yes, do this; they know how you function for real)
Ask very specific questions:
- “What will make me a strong senior next year?”
- “What’s one thing that might hold me back?”
- “If you were in trouble at 3am, what would you want me to be better at?”
Do not defend yourself. Just listen. Write it down that day.
6. Shadow the Senior Deliberately
You’ve been watching seniors all year, but mostly in survival mode. Now you watch them like you’re taking over their job—because you are.
This week you should:
- Pick 1–2 shifts or days and tell your senior:
- “I want to pay attention to how you run the team, not just my patients. Can I shadow your thinking for a bit?”
Specifically observe:
- How they:
- Prioritize: which page they return first, which patient they see first
- Communicate with:
- Nurses
- Consultants
- ED
- Night float
- Run rounds:
- Who speaks first
- How they correct juniors without destroying confidence
- Handle disasters:
- Code blue
- Sudden decompensation
- Angry family
Then ask them:
- “What are 3 things you do now that you wish you learned before being a senior?”
- “What did you underestimate the most about PGY2?”
You’re stealing their experience before you earn it the hard way.

Final 7–10 Days: Tighten, Transfer, and Transition
This is crunch time. At this point you should be executing a clear transition plan.
Think of the last 10 days as:
- Clean handoffs
- Final skill tightening
- Mental reset for the next year
7. Build and Use a “Senior Year Launch” Checklist
You’re not going to remember everything in the fog of call and fatigue. So yes, make an actual checklist.
Sample checklist items:
Clinical:
- Review your program’s escalation policies (RRT criteria, transfer to ICU thresholds).
- Re-read institutional order sets for: sepsis, DKA, stroke, ACS.
- Identify your go‑to resources for quick decision help (UpToDate, EM:RAP, local guidelines).
Leadership:
- Decide how you’ll run rounds (order, expectations for interns, how you want notes done).
- Draft a short “Expectations for the Team” script for day 1 with new interns:
- When to call you
- How to structure presentations
- Documentation expectations
- What you promise them (teaching, protection from nonsense where possible)
Personal:
- Schedule one actual day off before PGY2 starts. No moonlighting, no research, nothing.
- Fix non-work chaos: car inspection, dentist, bills, travel, family stuff. This all explodes mid-July if you ignore it.
| Focus Area | Daily Time Target |
|---|---|
| Clinical Workload | 70–75% |
| Senior Prep | 10–15% |
| Reflection & Notes | 5–10% |
| Admin/Logistics | 5–10% |
8. Clean Up Your Handoffs and Loose Ends
At this point you should be thinking like the person who’s inheriting your mess.
For your current patients:
- Stop punting decisions “to tomorrow” when tomorrow is post‑you.
- Make plans explicit in your notes:
- “If fever recurs, do X.”
- “If BP stays under Y, consider Z.”
For your program:
Clarify your PGY2 schedule:
- Know your first 3–4 rotations.
- Identify which are senior‑heavy (wards, ICU, nights) vs more independent (clinic, electives).
Send any necessary emails:
- Chiefs: “Anything I should review before I’m a senior on [service]?”
- Rotation directors: confirm expectations if you’re starting in a high-risk slot (e.g., ICU senior in July).
You don’t want to discover those expectations at 2am during your first cross-cover night.
9. Formalize What You’ve Learned
This is where you lock in your PGY1 experience so it doesn’t evaporate into vague impressions.
In your final week, at this point you should:
Write a 1–2 page “PGY1 Lessons” document:
- Clinical patterns you now recognize quickly
- Rules of thumb that actually held up (and those that didn’t)
- Pitfalls you fell into:
- Treating numbers instead of the patient
- Over-ordering imaging
- Forgetting to reassess after big changes
Add a short section:
- “If I could talk to my PGY2 self six months from now, I’d remind myself to…”
You’ll be shocked how useful this is when you feel stuck in December of PGY2.

| Category | Value |
|---|---|
| July | 20 |
| October | 45 |
| January | 60 |
| April | 75 |
| End of PGY1 | 85 |
Day-to-Day: How Your Last Month Should Actually Look
Let’s get concrete. Here’s how a typical day in your last month should feel.
Morning (Pre-rounds to Late Morning)
At this point in the day you should:
Use a tight pre-round routine:
- 1–2 minutes per patient max for data review.
- Jot 1–2 key issues per patient, not full essays.
Build mini-teaching moments:
- Pick one patient and tell the medical student: “You’re going to present this one. I’ll help you structure it.”
Practice senior‑style thinking:
- For each patient, ask yourself:
- “What’s the discharge barrier?”
- “What could go wrong in the next 12 hours?”
- “If this patient crashes, what will it look like first?”
- For each patient, ask yourself:
Midday (Rounds, Procedures, Calls)
This is where your future senior role really shows.
During this block you should:
Watch the attending but imitate the senior:
- Help keep rounds moving: gentle redirection, clarifying plans, summarizing.
- Step in to clarify unclear tasks for the intern or student.
Practice closed-loop communication:
- “So to recap: you’ll call cardiology now, and if they recommend cath we’ll move bed 3 to step-down.”
Say “I’ll handle that” sometimes:
- Call the consultant yourself.
- Coordinate a complicated transfer.
- Lead the family meeting alongside your attending rather than hiding in the back.
Late Afternoon / Early Evening (The Chaos Window)
Every service has that 4–7pm pileup. If you can handle this reasonably now, PGY2 will be survivable.
At this point in the day you should:
Force yourself to prioritize deliberately:
- Write a 3‑item “must get done before sign-out” list:
- Time-sensitive orders
- Discharges
- Unstable follow-ups
- Write a 3‑item “must get done before sign-out” list:
Practice mini-triage:
- A nurse calls about mild tachycardia in a stable patient and a new admission from ED at the same time.
- Decide: which do you attend to first, and why? Act like the senior would.
Ask your senior:
- “Can we briefly walk through how you prioritize pages in this time window?”
- Then copy their decision tree.
End of Shift (Last 20–30 Minutes)
If you’re sprinting full-speed to the last minute, your system is broken. Fix it now.
At this point in the day you should:
Start a hard stop 20–30 minutes before sign-out:
- Final orders.
- Micro-review of your sickest patients’ vitals and labs.
- Clean, accurate handoff updates.
Handoff like a senior:
- “Sick but stable because of X, if Y happens do Z, I’m most worried about A overnight.”
- That style will be exactly what you expect from your interns next year.
Spend 3–5 minutes on reflection:
- One thing that went well.
- One thing you’d redo.
- One decision you want to look up tomorrow.

Nights and Days Off During the Last Month
Even your off-time in this last month should be strategic. Not joyless—but intentional.
On Night Float or Call
At this point on nights you should focus on:
Rapid pattern recognition:
- Chest pain calls
- Hypotension pages
- “Patient is more confused” notes
Practicing escalation:
- Decide sooner when to:
- Call your senior/attending
- Call ICU
- Get imaging vs wait
- Decide sooner when to:
Use 10–15 quiet minutes to:
- Write down 1–2 “nightmares” you don’t feel ready for (e.g., crashing post-op patient, refractory hypoxia)
- Review one algorithm or guideline per night
On Your Days Off
You do not study all day. That’s how you burn out. But you don’t completely ignore PGY2 either.
On a day off in this last month you should:
- Spend:
- 1–2 hours max on:
- Reviewing your “PGY1 Lessons” document
- Skimming guidelines for frequent emergencies in your specialty
- The rest:
- Sleep
- Non-medical life
- Some activity that reminds you you’re a person, not just a badge and pager
- 1–2 hours max on:
Three Things to Remember About Your Last Month of PGY1
- This month is not “bonus time.” It’s the training ground for how you’ll function as a senior. Treat it like a live rehearsal.
- At every point, shift your mindset from “What do I do?” to “How would I explain this plan to someone junior to me?” That’s the real transition.
- Leave PGY1 with systems, not vibes: clear routines, a written lessons document, and a concrete senior-year launch checklist. Those are what will keep you standing when everyone starts looking to you.



















