The belief that “a fellowship will fix a low-paying specialty” is mostly wrong. The data show that subspecializing sometimes rescues income, sometimes barely moves the needle, and occasionally makes things worse once you factor in extra years of low pay.
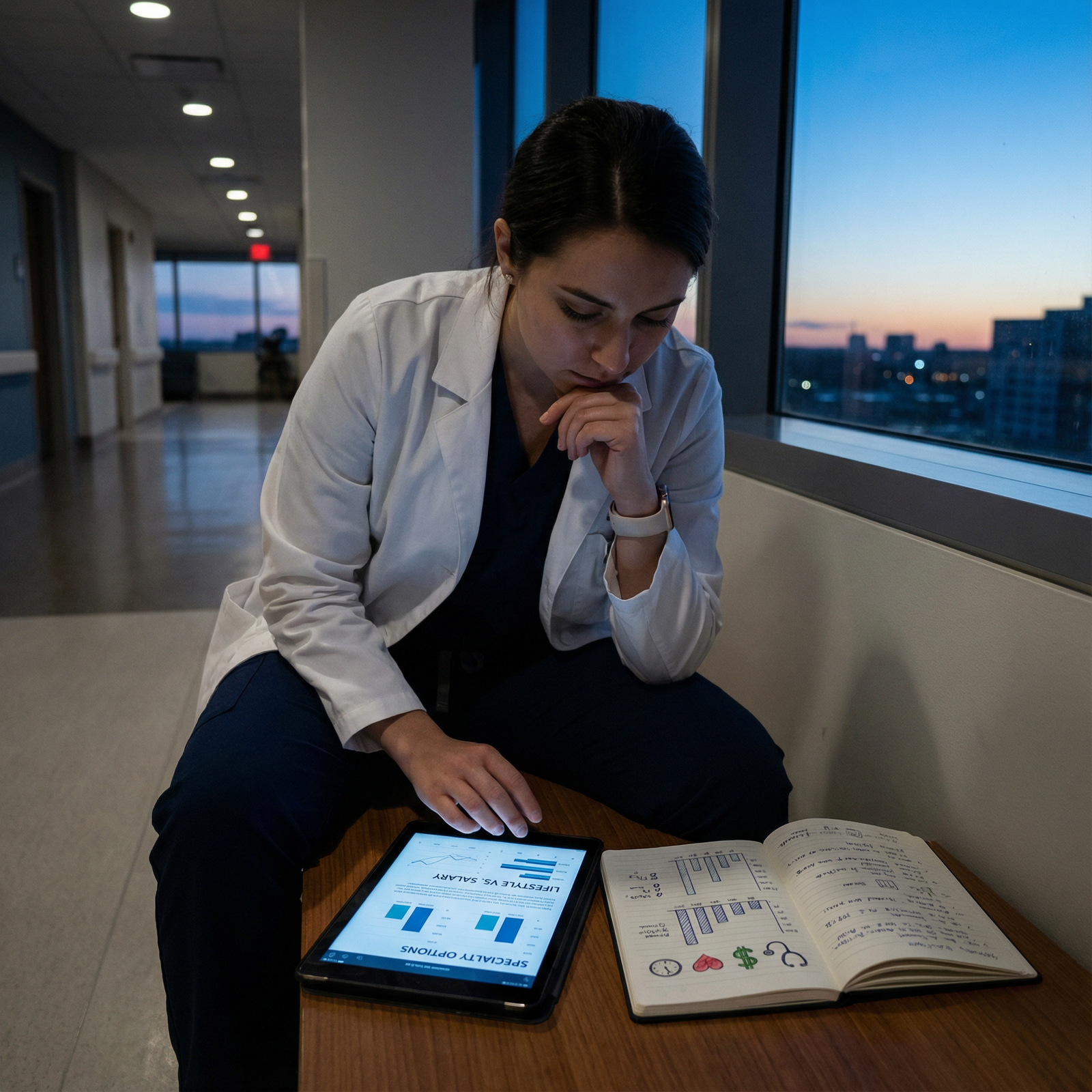
If you are in a low-paid specialty and thinking, “I will just do a fellowship and catch up,” you need to see the numbers laid out, not the anecdotes.
Below I will walk through actual compensation data, training lengths, and opportunity costs for the classic low-income paths: pediatrics, family medicine, psychiatry, neurology, and internal medicine in its lower-paid niches. Then we will answer the real question: does fellowship financially rescue you, or just make you a differently-trained low earner?
I am going to be blunt. For many of these paths, the fellowship is a lifestyle, intellectual-interest, or market-positioning decision, not a pay-rescue strategy.
1. Baseline: How Low Are the “Lowest Paid” Specialties?
You cannot talk about fellowship “rescue” without defining the starting point.
Using a synthesis of recent physician compensation surveys (MGMA, Medscape 2023–2024, Doximity), the lower end of the attending income spectrum clusters roughly as follows (all numbers approximate, rounded, and vary by region, practice type, and experience):
- Family Medicine: $250k–$290k
- General Pediatrics: $230k–$260k
- Pediatrics hospitalist: $260k–$310k
- Psychiatry (general adult): $290k–$340k
- Neurology (general): $290k–$340k
- Internal Medicine (general outpatient): $250k–$300k
- Geriatrics, Endocrinology, Infectious Disease, Rheumatology: $260k–$330k (yes, some IM subspecialties are still “low paid”)
Contrast that with:
- Orthopedic surgery, plastics, neurosurgery, cardiology, GI: commonly $550k–$800k+
- EM, anesthesiology, radiology: $400k–$550k+ range
So when a pediatrician says, “Maybe I should do cardiology so I don’t stay at $250k forever,” they are trying to move from the left tail closer to the median of physician incomes, not to the top 5%.
The key question: does fellowship move you from $250k territory to, say, $450k+, and does it do so early enough in your career to offset years of resident-level pay?
2. The Core Tradeoff: Extra Years vs. Marginal Income
Before diving into each specialty, let’s quantify the basic tradeoff:
- Additional training: typically 2–3 years of fellowship
- Compensation during those years: PGY4–6 salaries, roughly $65k–$80k per year depending on region
- Forgone attending income:
- A low-paid generalist starting at $250k–$280k
- So opportunity cost per year of fellowship ≈ $250k–$280k – $70k ≈ $180k–$210k
Over 3 years, that is roughly $540k–$630k of gross opportunity cost, plus debt interest, plus delayed retirement savings.
To “rescue” your income in any meaningful sense, the uplift in your attending salary from fellowship must be large enough, and last long enough, to outweigh that delay. Otherwise, you have just traded time and money for a title.
Let us quantify this properly in a simple comparison.
| Scenario | Years 1–3 Income (Post-Residency) | Starting Attending Income | Cumulative 10-Year Gross (Years 1–10) |
|---|---|---|---|
| Generalist (no fellowship) | \$250k/year | \$250k | \$2.5M |
| Fellow then Subspecialist | \$70k/year | \$350k | ≈ \$2.26M |
Rough math assumptions:
- Generalist: 10 years at $250k = $2.5M
- Fellow: 3 years at $70k (
$210k) + 7 years at $350k ($2.45M) = $2.66M - On raw gross income, you come out slightly ahead, but only if you really hit that $350k+ level and sustain it.
If your post-fellowship job pays $300k, the math flips, and you lose financially over the first decade. You might “catch up” later, but that is betting on a long career with constant demand.
That is the frame. Now, specialty by specialty.
3. Pediatrics: Does Subspecializing Rescue You?
Pediatrics is the archetypal low-paying field. Residents often talk themselves into fellowship with the line “only subspecialists get paid decently.” That is only partially true.
Synthesizing multiple compensation datasets, approximate numbers:
- General pediatrics: $230k–$260k
- Pediatric hospitalist: $260k–$310k
- Common pediatric subspecialties:
- Pediatric cardiology: $350k–$450k
- Pediatric critical care: $350k–$430k
- Neonatology: $350k–$450k, with outliers higher in high-acuity/locum markets
- Pediatric endocrinology, rheumatology, ID: often $250k–$320k (yes, still low)
To visualize this:

| Category | Value |
|---|---|
| Gen Peds | 245 |
| Peds Hosp | 285 |
| Peds Endo | 290 |
| Peds Cards | 400 |
| PICU | 390 |
| Neonatology | 410 |
General pattern:
- “Lifestyle” or cognitive subspecialties (endo, rheum, ID, heme-onc in some institutions) often do not provide a large bump over general pediatrics. Some are worse when you normalize for hours.
- High-acuity, high-intensity subspecialties (cardiology, PICU, NICU) usually give a real bump – on the order of $100k–$170k over general pediatrics.
Now layer in training length:
- Peds residency: 3 years
- Most peds fellowships: +3 years
- So 6 years total post-MD before “real” attending money
Does that rescue you? For the high-paying tracks, often yes in pure dollars over a long runway. But the cost is massive:
- 3 extra years at $70k → roughly $540k–$600k opportunity cost relative to a $250k pediatrician
- The uplift might be, say, from $250k to $400k (net +$150k/year)
Break-even rough math:
- You “lose” ≈ $540k by training 3 more years instead of working as an attending.
- You “gain” ≈ $150k/year once you are a subspecialist.
- Break-even ≈ $540k / $150k ≈ 3.6 years in practice.
So you start coming out ahead somewhere around year 4–5 as a subspecialist, assuming stable employment, no major shifts in reimbursement, and that you do not burn out of NICU nights at 45 and move to a lower-paid lifestyle job.
So in pediatrics:
- High-acuity subspecializing can financially rescue you relative to general pediatrics.
- Cognitive peds subspecialties often do not. They may even lock you into low pay with narrower job options.
One more subtlety: academic vs private. Academic pediatric subspecialists in many universities are still earning $230k–$280k with heavy research and teaching loads. That path is emphatically not a pay rescue, it is a mission choice.
4. Family Medicine: Can Fellowship Lift You Out of the Bottom?
Family medicine sits near the bottom of the income list, but its rescue route is less about traditional ACGME fellowships and more about scope of practice and setting.
Baseline:
- Outpatient FM, employed, standard panel: $250k–$290k
- Rural FM with procedures + OB: $300k–$400k+ in some markets
- Direct primary care / concierge hybrid: very wide range ($220k–$500k+) depending on panel and fees
Formal FM fellowships include sports medicine, geriatrics, obstetrics, addiction, palliative care, and academic medicine.
Compensation pattern (approximate national medians):
- FM + Sports Medicine: $300k–$380k (wide variance – employed vs owning a high-volume clinic with imaging / injections)
- FM + OB fellowship: can push into $320k–$400k in some markets, especially rural with call
- Geriatrics, Palliative, Addiction: often $260k–$320k, not a large jump from standard FM
The data show a few things:
- The biggest financial driver in FM is not fellowship; it is geography, procedures, and business model.
- Sports medicine can help, but if you end up employed in an academic center, your pay may actually be flat or lower vs a high-RVU community FM job.
- Geriatrics and palliative fellowships are notorious for adding 1–2 years of training with minimal or negative financial return.
From an opportunity-cost perspective, most FM fellowships are 1 year:
- Opportunity cost ≈ $250k (general attending) – $70k (fellow) ≈ $180k
- Post-fellowship uplift: maybe $30k–$80k/year depending on job.
Break-even is 2–6 years. Not awful. But remember: you could have achieved similar uplifts by moving to a rural market, increasing procedures, or joining a more aggressive compensation model without adding another credential.
So in FM, subspecializing can help, but it is rarely the primary financial lever. The market punishes cognitive, non-procedural work, fellowship or not.
5. Psychiatry: Are Fellowships a Pay Multiplier or a Detour?
Psychiatry has quietly crept up the pay ladder in the last decade due to demand, telepsychiatry, and shortages. It is no longer as low as pediatrics or primary care in many markets.
Baseline:
- General adult psychiatry: $290k–$340k (W2 employed, outpatient-heavy)
- Well-run private or telepsych practices: significant upside, $350k–$450k+ for high-volume attendings
Common fellowships:
- Child and Adolescent Psychiatry (CAP)
- Addiction
- Forensic
- Geriatric
Compensation patterns (approximate):
- Child and Adolescent: $320k–$380k average, some markets higher due to severe shortages
- Forensic psychiatry: $350k–$450k for those who really specialize and do high-paid legal work
- Addiction, Geriatric: often similar to or slightly above general psych, roughly $300k–$360k

| Category | Value |
|---|---|
| General Psych | 315 |
| Child & Adol | 350 |
| Forensic | 400 |
| Addiction | 330 |
The key detail: the psychiatry market is so hot that many general psychiatrists can match or exceed subspecialty salaries by running efficient outpatient or telehealth practices and avoiding academic pay caps. You do not need a fellowship to make “good money” in psychiatry.
Child and adolescent psych fellowship is 2 years if entered after PGY‑3 (the integrated fast-track model), which complicates the opportunity cost math slightly. But simplified:
- Extra 1–2 years at ~$70k–$75k
- Uplift of maybe $30k–$60k/year as a CAP vs general psych in W2 roles
- But a motivated general psychiatrist can sometimes out-earn a CAP by simply doing high-demand meds management with minimal overhead.
Verdict: In psychiatry, most fellowships are not strict financial rescue mechanisms. Forensic psychiatry is the strongest outlier if you commit to legal work. CAP helps, but the real driver is still market demand and how you structure your practice.
6. Neurology and “Low-Paying” Internal Medicine Subspecialties
Neurology and some IM subspecialties are in an odd limbo: long training, heavy cognitive load, relatively modest pay compared with procedural fields.
Baseline:
- General Neurology: $290k–$340k
- IM (general outpatient): $250k–$300k
- IM hospitalist: $300k–$360k (depending on shifts and geography)
Lower-paid IM subspecialties (ballpark):
- Endocrinology: $260k–$320k
- Rheumatology: $280k–$350k
- Infectious Disease: $260k–$320k
- Geriatrics (IM route): $250k–$300k
- Hematology-only (non-malignant heavy): often closer to low-300s in some systems
Higher-paid IM subspecialties:
- Cardiology: $500k–$650k (can be more for interventional)
- Gastroenterology: $550k–$700k+
- Pulm/CC: $420k–$520k, sometimes higher

| Category | Value |
|---|---|
| Gen IM | 275 |
| Endo | 295 |
| ID | 285 |
| Rheum | 320 |
| Cards | 575 |
| GI | 625 |
| Pulm/CC | 470 |
The obvious conclusion:
- If you are subspecializing in procedural IM fields (cards, GI, interventional subspecialties), yes, fellowship very clearly rescues you financially.
- If you are subspecializing into endocrine, ID, geriatrics, or some heme roles, the uplift over general IM is marginal at best, and sometimes negative when adjusted for call, complexity, or academic environments.
Neurology fellowships:
- Epilepsy, Stroke, Movement Disorders, MS, Neuromuscular, Neurocritical Care
- Many of these bump salaries modestly: into the $320k–$400k range, rarely beyond that without specific private practice structures or high-call neurocritical setups.
Add the training time:
- IM: 3 years + 2–3 year fellowship (5–6 total)
- Neurology: 4 years (PGY1 + 3 neurology) + 1–2 year fellowship (5–6 total)
For endocrine or ID, for example:
- Opportunity cost: 2–3 years of $70k vs potential $300k generalist income
- Extra income: maybe +$30k–$50k/year as a subspecialist
It takes a decade or more to fully “catch up,” and that is before you account for lifestyle and burnout risk.
Again: these fellowships are often negative financial plays if your sole goal is income.
7. Non-Financial Factors That Skew the Decision
Income is not the only variable, but you picked this topic, so let us stay quantitative while acknowledging a few big confounders.
Burnout and longevity
Working 1.0 FTE as a NICU attending at $425k for 7 years and then cutting to 0.5 FTE because you are exhausted is not obviously better than 0.8 FTE general pediatrics at $240k for 25 years.
If fellowship pushes you into a niche with high intensity and early burnout, the lifetime income advantage may vanish.
Geography and negotiation leverage
A subspecialty gives you scarcity value in some markets. A single pediatric gastroenterologist in a mid-sized city can often negotiate significantly better terms than the “7th general pediatrician” in a large hospital system.
This leverage is very uneven geographically. Rural and underserved areas often pay more for both generalists and subspecialists. The fellowship credential sometimes just opens doors; the negotiation skill sets the pay.
Academic vs private practice
Data from academic centers repeatedly show a 10–30% pay penalty vs community/private roles, especially in pediatrics and IM subspecialties. Most fellowships are pipelines to academic jobs.
So the paradox: the more competitive and research-heavy the fellowship, the more likely you are to spend your career in a system that underpays you relative to community RVU work.
8. What the Data Actually Say About “Rescue”
Strip away the narrative and look at categories.
Across the lowest paid specialties, you have three broad outcomes when you add fellowship:
- Clear financial rescue (large uplift)
- Marginal financial benefit (small uplift)
- Financially negative (delayed earnings with little or no pay bump)
Here is the pattern, simplified:
| Base Specialty | Fellowship Type | Typical Impact on Income |
|---|---|---|
| Pediatrics | NICU, PICU, Cards | Large positive uplift |
| Pediatrics | Endo, Rheum, ID | Small or neutral uplift |
| Family Med | Sports Med, OB | Small–moderate uplift, setting-dependent |
| Family Med | Geri, Palliative | Often neutral or negative |
| Psychiatry | Forensic | Large uplift if fully specialized |
| Psychiatry | Child, Addiction | Small–moderate uplift; market-dependent |
| IM/Neuro | Cards, GI, Interventional | Very large uplift |
| IM/Neuro | Endo, ID, Geri, some Neuro subs | Small or negative uplift |
Notice the pattern: the only consistently strong “rescues” are:
- High-acuity pediatric subspecialties
- Procedural heavy IM subspecialties (cards, GI, interventional)
- Forensic psychiatry for those who truly lean into the forensic niche
Everything else is either marginal or a wash.
9. How to Personally Run the Numbers
If you are choosing a fellowship from a low-earning base, you should treat it like an investment decision. With actual projections, not vibes.
Basic framework:
Estimate post-fellowship pay realistically
- Use compensation reports for your region and practice type
- Adjust down for academic centers by 10–30% if planning that track
Estimate generalist pay you could earn if you skipped fellowship
- Include realistic potential for rural/locums/telehealth/practice ownership if you are willing to do those
Compute opportunity cost:
- Opportunity cost per year ≈ (generalist attending pay – fellow salary)
- Multiply by fellowship years
Estimate uplift:
- Uplift = (post-fellowship attending pay – generalist pay) per year
Compute simple break-even:
- Break-even years ≈ total opportunity cost / uplift
If break-even is >10 years, and you are on the fence about the field itself, you are probably not being rescued financially. You are just buying a credential.
You can sanity-check this with your own numbers or I can walk through a specific scenario if you tell me your specialty and target fellowship.
10. The Bottom Line: When Fellowship Actually “Rescues” a Low-Paid Income
The data show a very clear conclusion:
Fellowship rescues income only when it moves you into a substantially higher compensated niche, usually:
- Procedures (cards, GI, interventional subspecialties)
- High-acuity pediatric care (NICU, PICU, peds cards)
- Highly monetizable niches in psych (forensics)
Most cognitive and lifestyle-focused fellowships in the lowest paid specialties do not fix low income.
- Endocrine, geriatrics, ID, palliative, many academic-heavy pediatric subspecialties fall here.
- They may offer meaning, interesting work, or better day-to-day fit. But financially, they often just add years of low pay with minimal upside.
You can often get a “rescue” effect faster with:
- Geography changes (rural, underserved)
- Practice model shifts (private, telehealth, direct care, procedural expansion)
- Negotiation and productivity tweaks
So, does subspecializing rescue low-paid incomes?
Sometimes. But only if you treat it as a hard-nosed financial decision tied to specific high-paying niches, not as a magical promotion that automatically upgrades your pay grade.
If you are going to trade 2–3 more years of your life and six figures of opportunity cost, do it with a spreadsheet open, not just a hope that “fellows get paid more.”



















