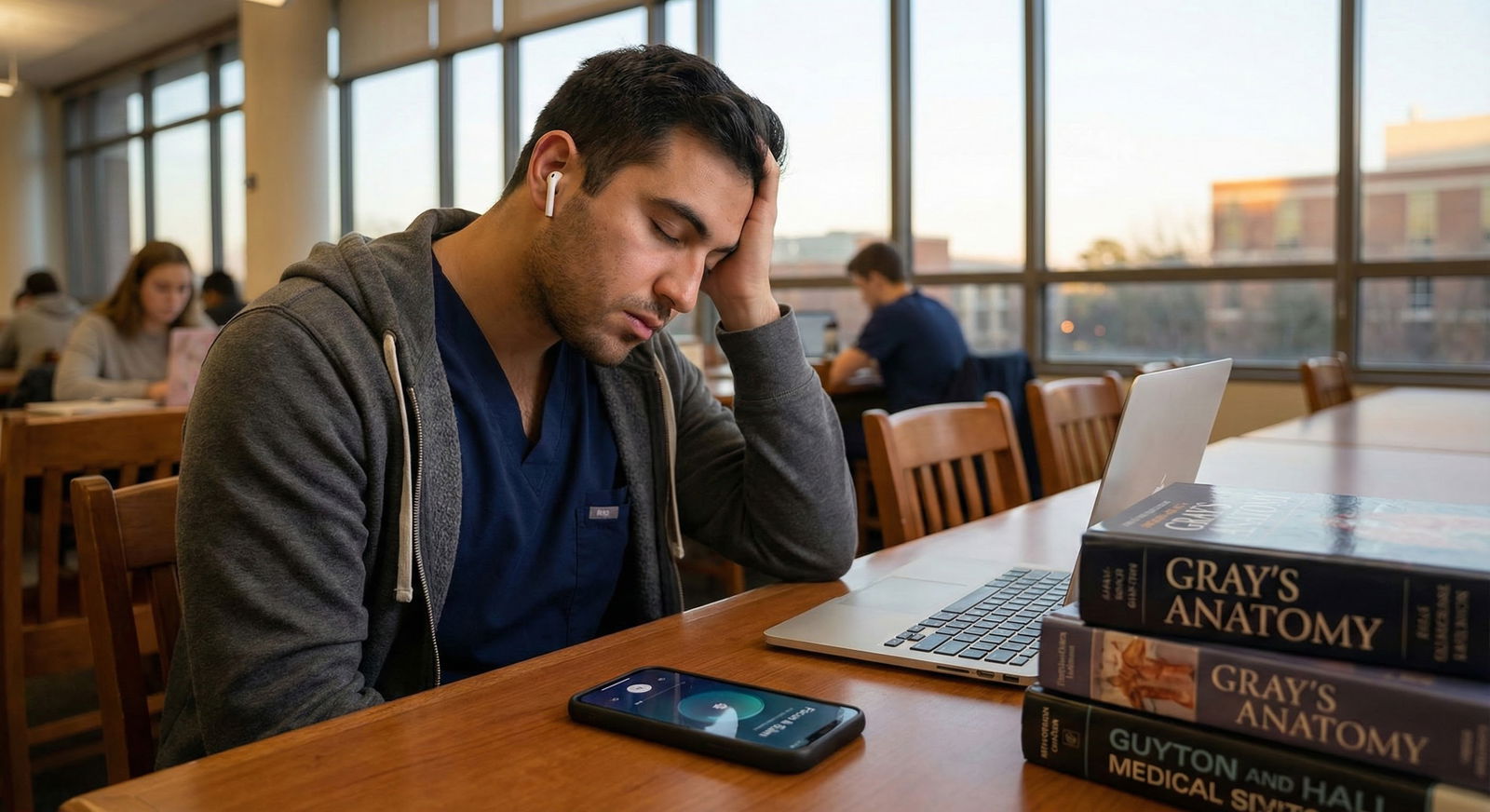
What do you actually get if you add a meditation app to a life full of 14‑hour study days, relentless exams, and constant low‑grade panic—real relief, or just a prettier timer for your anxiety?
Let’s be blunt: meditation apps are neither magic nor a scam. They’re tools. For med students under heavy stress, they can absolutely help—but only in specific ways, and only if you use them strategically instead of like a guilt-inducing gym membership on your phone.
Here’s the breakdown you’re looking for.
What Meditation Apps Actually Do (Scientifically, Not Vaguely)
Strip away the branding and soft music and most meditation apps do a few core things:
- Guide you through mindfulness or breathing exercises
- Help you build a habit with reminders and “streaks”
- Offer quick interventions for acute stress, poor sleep, and focus lapses
You don’t have to take the app’s word for it. There’s real data behind this.
Multiple randomized controlled trials in medical students and residents show:
- Short daily mindfulness practice (often app-based or app-like)
- Decreases perceived stress
- Reduces symptoms of anxiety and depression
- Improves sleep quality
- Sometimes improves attention and working memory
Is this life-changing for everyone? No. Is it clinically useful for a lot of overwhelmed med students? Yes.
Here’s the part people miss: the benefit you get has way more to do with how you use it than which app you pick.
How Much Help Can You Realistically Expect?
Let’s talk expectations, because this is where people get disillusioned.
Meditation apps are good at:
- Lowering the “background noise” of stress
- Helping you fall asleep faster and sleep more deeply
- Giving you simple, repeatable tools during panic or overwhelm
- Making you more aware of when you’re mentally spiraling
- Slightly improving focus and emotional regulation
They are not good at:
- Fixing burnout when your schedule is objectively brutal
- Replacing therapy or psychiatry for moderate–severe anxiety or depression
- Solving toxic environments, abusive attendings, or systemic issues
- Working if you open the app once every 3 weeks and say “meh, didn’t help”
Think of them like a stethoscope: powerful tool, zero value in your backpack.
Where They Actually Fit in Med School Life
Let’s map this to real med school phases, because the needs change.

| Category | Value |
|---|---|
| M1 Fall | 60 |
| M1 Spring | 70 |
| M2 Board Prep | 95 |
| M3 Rotations | 85 |
| M4 Interviews | 75 |
Preclinical years (M1–M2)
Stress type: volume and identity. You’re drowning in content and feeling like an imposter.
Meditation apps help most here with:
- Sleep onset: guided sleep meditations, body scans
- Brief recovery breaks: 5–10 minute “reset” sessions between blocks of Anki/lectures
- Early awareness of spiraling: noticing catastrophizing before it runs your day
If you’re doing 10–15 minutes a day, you usually feel a difference within 1–2 weeks. Not nirvana. But a lower baseline hum of anxiety.
Dedicated board prep (USMLE/COMLEX)
This is where I see the apps earn their keep, if used right.
Use them for:
- Pre-study settling: 5-minute breathing or focusing exercise before diving into UWorld
- Panic control: short SOS meditations when you score low on an NBME and your brain is screaming “I’m not going to be a doctor”
- Sleep routine: same 10–15 minute track every night to signal “we’re done for today”
What you should not do: schedule 45-minute meditations and then guilt yourself for “failing” when you inevitably skip. That just adds another failure to your day.
Clinical years (M3–M4)
Different stressor: loss of control. Random call schedules, emotional cases, difficult teams.
Here, apps help mainly with:
- Micro-recovery: 3–5 minute breathing in the call room, stairwell, or parked car
- Pre-sleep decompression after heavy cases or bad days
- Emotion processing: some apps have brief “check-in” or self-compassion modules
But again, they’re not going to make a brutal surgery month feel gentle. They just keep your stress response from getting locked in the red zone 24/7.
Which Features Actually Matter (And Which Are Just App Store Glitter)
Don’t get seduced by aesthetics alone. For a med student under heavy stress, these features actually move the needle:
| High-Value Feature | Overhyped / Low-Value Feature |
|---|---|
| Short 3–10 min sessions | 45+ min advanced practices |
| Offline downloads | Endless celebrity guest content |
| Sleep-specific tracks | Inspirational quote collections |
| SOS / emergency meditations | Fancy background animations |
| Progress reminders | Complex social/community feeds |
If an app doesn’t make it stupidly easy to:
- Start a 5-minute session with 2 taps
- Save favorites you actually use
- Work offline (for hospital basements, planes, etc.)
…it’s going to sit unused.
A Simple, No-BS Way to Use Meditation Apps Under Heavy Stress
Here’s a concrete framework. If you follow this for 2–3 weeks, you’ll know if meditation apps are “for you” or not—without wasting time or money.
Step 1: Define your main problem (1 sentence)
Not a vibe. A problem.
Examples:
- “I can’t fall asleep because my brain is replaying lectures and mistakes.”
- “I have daily waves of panic during board prep.”
- “I snap at people by 4 pm and feel constantly on edge.”
Your problem determines how you use the app.
Step 2: Pick one primary use case
Don’t try to do everything at once. Choose ONE:
- Sleep
- Focus before studying
- Panic / acute anxiety
- Emotional decompression after shifts
Then:
- Sleep → 10–15 minute nightly routine
- Focus → 5 minutes before your first major study block
- Panic → 3–5 minute SOS track saved to favorites
- Decompression → 10 minutes after getting home or before bed
Step 3: Set a tiny, realistic minimum
For heavy stress, willpower is gone. So set the bar embarrassingly low:
- “I will open the app and do 3 minutes daily.”
- If you do more, great. But 3 minutes is the win.
If you’re thinking “3 minutes can’t do anything,” you’re wrong. I’ve seen students go from never meditating to consistent practice because 3 minutes felt doable at midnight after call. And over time, 3 often turns into 7–10 without drama.
Step 4: Attach it to an existing habit
Don’t rely on raw discipline. Attach it to something you already do:
- After brushing teeth at night → sleep meditation
- After pouring morning coffee → 5-minute focus session
- After turning off Anki for the day → decompression track
If you’re starting a “new habit” floating in space, it dies by week two of exam block.
The Real Limitations (Where Apps Are Not Enough)
I’m not going to pretend a meditation app fixes serious mental health problems.
Red flags where an app alone is not sufficient:
- You’ve lost interest in things you used to enjoy for more than 2 weeks
- You’re having frequent thoughts of self-harm, not wanting to wake up, or “everyone would be better off without me”
- You’re using alcohol, weed, or stimulants just to sleep, cope, or function
- Panic attacks are frequent and disabling
- Your performance is collapsing (not just “lower than I want,” but failing, missing deadlines, not showing up)
In those cases:
- You need a real human: campus counseling, a therapist, psychiatrist, or physician
- Meditation can be an adjunct to treatment, not the main intervention
If your school has free counseling and you’re ignoring it while trying 8 different meditation apps instead—that’s backwards.
Apps vs Other Coping Strategies: How They Compare
You’ve only got so much time and energy. So how do meditation apps stack up against other tools?

| Category | Value |
|---|---|
| Exercise | 80 |
| Sleep hygiene | 75 |
| Meditation app | 60 |
| Talking to friend | 70 |
| Therapy | 85 |
Roughly how I’d rank them for most med students:
- Exercise: Highest return if you can fit it in consistently. But on 80-hour weeks, it’s often the first thing to go.
- Sleep hygiene: Game-changing but hard when your brain is screaming about tomorrow’s exam.
- Meditation app: Lower barrier, can be done in bed, call room, Uber, bathroom, wherever. Not perfect, but accessible.
- Talking to a friend: Great for connection, not always for skills.
- Therapy: Gold standard for real distress, but limited by cost, access, and your schedule.
The value of meditation apps is that they’re available exactly when you’re anxious, it’s 1 am, and the gym is closed and your therapist is asleep.
Practical Recommendations: If You’re Going to Try This, Do It This Way
If you want a concrete starting point, use this 14‑day experiment:
Days 1–3: Setup phase
- Pick ONE app (free trial is fine)
- Choose:
- 1 sleep track (10–15 min)
- 1 short focus track (3–5 min)
- 1 SOS/panic track (3–5 min)
- Save them to favorites
Days 4–10: Consistency test
- Every night: do the same sleep track before bed
- On days you study: do the focus track before your first serious block
- Use the SOS track if you hit a panic spike (even once makes a difference)
You’re assessing:
- Is it easier to fall asleep?
- Are your pre-study freak-outs slightly quieter?
- Do you feel less wrung-out at the end of the day?
Days 11–14: Adjust or ditch
- If you notice benefit: keep going and maybe add a second track for decompression after exams or shifts
- If you notice nothing at all: try a different style (less “woo,” more breathing-based, or vice versa) or accept this isn’t your tool and move on without guilt
Bottom Line: Do Meditation Apps Really Help Med Students Under Heavy Stress?
Yes, they can—when:
- You use them for specific problems (sleep, panic, focus), not as vague “wellness”
- You keep the sessions short and consistent, not aspirational and unrealistic
- You let them be part of your toolkit, not the entire plan
They won’t fix a toxic culture, an impossible exam schedule, or untreated depression. But for many med students, they turn the volume down from 9 to 6. And in the middle of boards or a brutal rotation, that difference is not small.
FAQ (Exactly 6 Questions)
1. How many minutes a day do I actually need to meditate for it to help?
For most med students, 5–15 minutes a day is enough to see benefits in a couple of weeks. You don’t need 45-minute sessions. I’d rather see you do 5 minutes daily than 30 minutes once a week. Consistency beats duration.
2. Is there any point starting during dedicated board prep, or is it “too late”?
Not too late at all. In dedicated, even a week of short, daily practice can help with sleep and panic. Don’t aim for perfection. Aim for a 3–10 minute track before bed and, if possible, a 3–5 minute session before your first study block. That’s it.
3. Are free meditation options good enough, or do I need a paid app?
Free is often good enough to start. Many apps have limited free libraries that cover basics: breathing, body scans, sleep tracks. You can also use completely free resources (like simple timed breathing or YouTube-style body scans). If you notice real benefit and want more structure, then consider paying.
4. What if my mind won’t stop racing and I “fail” every meditation?
That’s not failure—that’s the whole game. Meditation is noticing your mind racing and gently bringing it back, over and over. If you catch your mind wandering 100 times, that’s 100 reps. Over time, the wandering lessens in intensity and you react less violently to it.
5. Can meditation apps replace therapy for anxiety or burnout?
No. They’re useful adjuncts, not full treatment. If you’re dealing with significant anxiety, depression, burnout, or any thoughts of self-harm, you need a human clinician. Use the app alongside therapy or meds, not instead of them.
6. What’s the single best way for a med student to start using a meditation app today?
Tonight, pick one sleep track (10–15 minutes max). Commit to using it every night for 7 days before bed, phone on Do Not Disturb, lights off. Don’t worry about “doing it right.” Just listen. After a week, decide if your sleep onset and pre-sleep anxiety improved at all. If yes, keep going and add one short daytime track. If no, switch style or app once—then re-test.
Key takeaways: meditation apps help most when you target a specific problem and keep it short and consistent; they’re a solid tool but not a cure for serious distress; and a 7–14 day focused trial is enough to see whether they’re worth a real place in your med school survival kit.




















