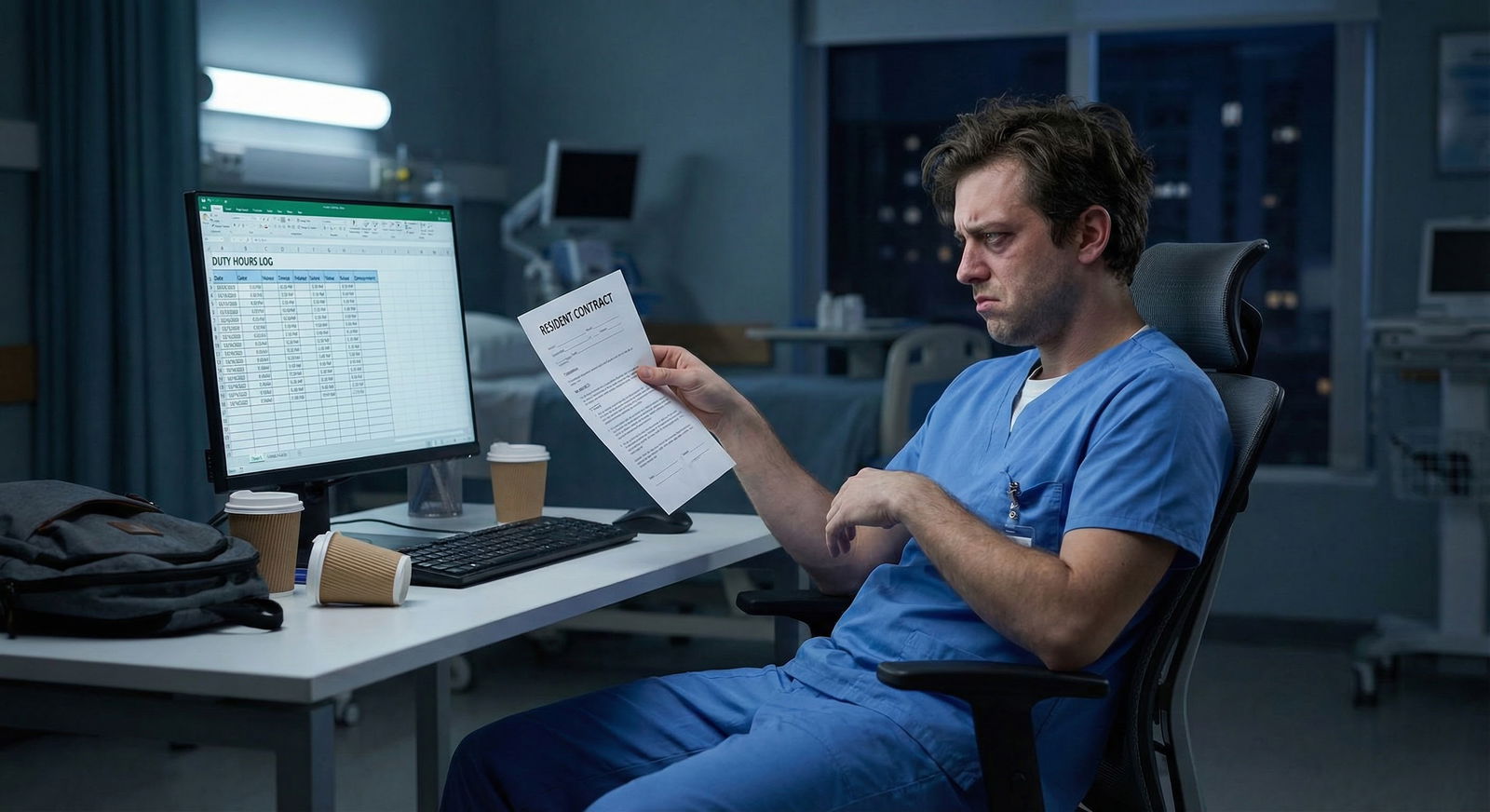
The fastest way to wreck a good residency is not burnout. It is a moonlighting violation that your program director learns about from the ACGME instead of from you.
Let me be direct: residents usually do not get in trouble for moonlighting because they are greedy. They get in trouble because they are sloppy and assume the rules are “guidelines” instead of hard limits with audit trails.
You can absolutely moonlight safely and legally in many programs. But if you do it the way a lot of residents do—quietly, informally, and with fuzzy math on your hours—you’re playing chicken with your license, your visa (if applicable), and your ability to graduate on time.
This is what trips people up.
The Core ACGME Moonlighting Rules Residents Keep Ignoring
Most residents who violate ACGME rules don’t even know exactly what those rules say. They just go off vibes: “Everyone in the class above us moonlighted; it must be fine.”
That’s how people end up in front of the Clinical Competency Committee pretending they didn’t know.
Here are the non‑negotiables that ACGME cares about for all specialties:
- Moonlighting counts toward duty hours
- Duty hours must average ≤80 hours/week over 4 weeks
- You must have 1 day in 7 free (averaged over 4 weeks)
- You must have required time off between duty periods
- Residents cannot moonlight without written program director approval
- PGY‑1s are not allowed to moonlight. Period.
- Program requirements may be stricter than ACGME; hospital policy may be stricter than both
Ignore any of those, and you’ve just made your program non‑compliant. Programs do not like being made non‑compliant.
| Rule Area | Typical Requirement |
|---|---|
| Duty hours cap | ≤80 hrs/week, averaged over 4 weeks |
| Day off requirement | 1 day off in 7, averaged over 4 weeks |
| PGY‑1 moonlighting | Not allowed |
| Approval | Written PD approval required |
| Counting hours | Moonlighting hours = duty hours |
| Rest between shifts | Must maintain ACGME rest requirements |
Do not rely on “what everyone says” about what’s allowed. Your PD and your GME office define the details. And they’re the ones answering to ACGME when something goes wrong.
Mistake #1: Treating Moonlighting as “Off the Books”
The most common—and dumbest—mistake: pretending that moonlighting “doesn’t count” as work.
Let me spell it out.
If you:
- Work at Hospital A as a resident from 7a–7p
- Then work at Hospital B from 8p–8a for moonlighting
- And only log 12 hours on your residency duty hour system
…you just lied on a federally monitored compliance record. That’s not “rounding.” That’s falsification of records.
How people accidentally do this
I’ve watched residents do all of the following:
- Only record duty hours from their own program hospital, not their external moonlighting gig
- “Forget” to log a string of moonlighting nights during an ICU month because the numbers looked scary
- Log the moonlighting in the wrong category (e.g., “home call” or “other”) so the total looks more reasonable
- Stop updating duty hours entirely during peak moonlighting season
They think the GME office is just nagging them about paperwork. They forget those logs are exactly what ACGME reviewers will ask for if there’s ever a complaint or a bad outcome.
Why this is so dangerous
When you treat moonlighting as invisible:
- You break the 80‑hour rule on paper, not just in real life
- You give your PD no chance to adjust your schedule to keep you compliant
- You create a neat little dataset that proves you intentionally hid hours
- You drag your whole program into an ACGME citation if they audit
Do not do “off the books” work. If you’re not comfortable putting it into duty hours, you should not be doing it.
Mistake #2: Ignoring the 80‑Hour Average Because “It’s Just This Month”
Residents tend to think in rotations. ACGME thinks in rolling 4‑week blocks.
The classic error:
“I’m on an easier elective next month, so I’ll just load up on moonlighting this ICU month.”
Here’s the trap: duty hours are tracked by actual weeks, not by your rotation labels.
You might convince yourself of this logic:
- ICU month: 75 clinical hours/week + 12 moonlighting hours/week = 87
- Next month: easy elective at 55 hours/week, no moonlighting
- Average over 8 weeks = (87+87+55+55)/4 = 71 hours/week
You think you’re safe. But your program’s duty hour system usually doesn’t know that next month will be easy when you schedule moonlighting for this month. All it sees in real time is weekly and rolling 4‑week violations.

| Category | Value |
|---|---|
| No Moonlighting | 70 |
| 8 hrs/wk Moonlighting | 78 |
| 16 hrs/wk Moonlighting | 86 |
Where this bites residents
- Some duty hour systems auto‑flag 80+ hours in any single week
- ACGME site visitors look at patterns of violations, not just the average
- If there’s a patient safety event, the plaintiff lawyer will go week by week, not by your 4‑week smoothing fantasy
The risky mindset is: “I’ll make up for it later.” That sounds like a loan. And like all loans, it accumulates risk and interest.
If you’re regularly hitting 70+ hours/week from residency alone, heavy moonlighting is asking for trouble. Sooner or later your rolling average crosses the line, and the wrong person notices.
Mistake #3: Moonlighting Without Written PD Approval (or With a Vague One)
Verbal approval is not approval. A joking “yeah, go make your millions” from a PD during a conference doesn’t count.
The ACGME’s language is clear: residents must not moonlight without specific approval of the program director. That means documented. Usually in a standard GME form or email.
Where I’ve seen residents screw this up:
- “My PD said moonlighting was okay in general, so I didn’t need to tell them about each gig.”
- “The hospital credentialing office cleared me. Isn’t that enough?”
- “Everyone in my class does it. Nobody is getting individual forms signed.”
Then someone has a bad outcome at the moonlighting site. Suddenly the PD is being asked:
- Did you approve this?
- Did you assess the resident’s readiness?
- Did you ensure the resident would still meet all duty hour rules?
If the only honest answer is “I had no idea,” this becomes a program problem, not just your problem.
What proper approval should look like
You want something like:
- A GME moonlighting approval form signed by your PD and sometimes DIO
- A statement that clearly says:
- How many hours per week are permitted
- What settings (internal vs external)
- What type of work (ED coverage, cross‑cover, urgent care, etc.)
- A requirement that you report all moonlighting hours in the duty hour system
If your program doesn’t have a formal process, that’s not a green light. That’s a risk flag. Get explicit, written permission anyway. Email counts. But keep it.
Mistake #4: Pretending PGY‑1 Moonlighting “Doesn’t Count”
This one is straightforward: ACGME prohibits moonlighting for PGY‑1 residents. Internal. External. Cash. Food vouchers. All of it.
Yet every year, there’s at least one intern who:
- “Helps out” at a family member’s clinic seeing patients
- Works “PRN” at their old scribe job but now writes orders “just to help”
- Covers urgent care shifts under a supervising physician but functions like an independent provider
They rationalize it as: “I’m not really moonlighting; I’m just picking up extra experience and getting paid.”
The ACGME does not care how you label it. If you’re:
- Using your MD/DO degree
- Interacting with patients
- Providing clinical work
- Getting compensated
…that is moonlighting, and PGY‑1 residents are not allowed to do it.
You do not want to be the intern whose side hustle becomes an institutional self‑report to ACGME.
Mistake #5: Internal vs External Moonlighting Confusion
Residents constantly mix these up:
- Internal moonlighting – at your own institution
- External moonlighting – at a different hospital/clinic
Your program may allow one but not the other. They may impose different rules on each.
I’ve seen this scenario more times than I care to admit:
- Program explicitly bans external moonlighting
- Resident assumes internal shifts are fine because “we’re just covering extra nights for the department”
- Those shifts are:
- Paid separately
- Not counted as part of the residency schedule
- Sometimes completely unreported in duty hours
That’s still moonlighting. And if it’s not being counted toward duty hours, that’s a double violation.
Watch out for “gray zone” shifts
Red flags:
- “Bonus pay” for extra call above the contract
- Urgent care shifts under faculty NPI but you’re seeing all the patients
- Extra ED coverage that’s not built into the rotation schedule
- “Per diem” roles that magically started when you became a resident
If you’re being separately paid to provide clinical care, assume it is moonlighting until your GME office tells you otherwise in writing.
Mistake #6: Overstepping Scope of Training While Moonlighting
This one doesn’t just risk ACGME problems. It risks malpractice and licensure trouble.
Residents get into trouble when they moonlight in roles that assume a level of independence they don’t actually have yet. Typical risky setups:
- A PGY‑2 IM resident running a solo rural ED at night
- A psych resident covering a general med floor with no in‑house attending
- A surgical resident doing urgent care procedures with minimal backup
The ACGME requires that moonlighting must not interfere with the resident’s ability to achieve the goals and objectives of the educational program. If you’re functioning like an attending outside your training level, you are one serious case away from everyone asking why the program “allowed” it.
Hospitals love cheap coverage. They will absolutely overestimate what a resident can safely handle. You are the one whose name goes on the line when something goes sideways.
If the moonlighting role expects you to be fully independent with little backup:
- Your PD is unlikely to be thrilled if they see the job description
- Your malpractice carrier might have an opinion too
- ACGME reviewers will not be impressed if they hear about it
Ask for the exact responsibilities and expected level of independence in writing. Share that with your PD before agreeing.
Mistake #7: Letting Moonlighting Crush Your Rest Requirements
Residents fixate on the 80‑hour rule and forget the rest and days‑off rules are just as real.
Common failures:
- Working a 24‑hour moonlighting shift right before a regular clinical day
- Stacking moonlighting on your only “day off” every week
- Doing late‑night moonlighting followed by early‑morning clinic every time it’s offered
ACGME expects:
- 1 day free of all clinical work every 7 days, averaged over 4 weeks
- Adequate time off between duty periods (varies by specialty and year, but there are minimums)
Note that “all clinical work” includes moonlighting. So:
- If you moonlight every Sunday during a tough inpatient month, you might have zero actual days off
- If you go from a night moonlighting shift directly to scheduled residency work, you may break rest rules
This is how your life starts to feel like one long shift with random naps. And how errors start to creep in.
Protect one real day off. Not “day to catch up on notes and moonlight at night.” A real break.
Mistake #8: Assuming Your Visa Status Makes Moonlighting “Flexible”
If you’re on a visa (J‑1, H‑1B, etc.), you have another layer of rules.
The mistake I’ve seen too many times:
- Resident on a J‑1 or H‑1B picks up external moonlighting
- Hospital credentialing clears them (because they’re focused on licensure, not immigration)
- Resident assumes “If credentialing approved it, it must be legal”
Then an immigration lawyer gets involved. And it turns out:
- Their visa is tied to a specific employer and site
- No one amended the petition for the external work
- The moonlighting likely violated visa terms
Now it’s not just ACGME. It’s immigration status, future employment, maybe even ability to stay in the country.
Rule of thumb: if you’re on a visa, you do not moonlight anywhere—internal or external—without explicit written clearance from:
- Your PD
- Your GME office
- An immigration attorney or institutional international office
If any of those say “no,” believe them.
Mistake #9: Trusting Other Residents’ “Rules” More Than Written Policy
The most dangerous sentence in residency:
“Everyone does it and it’s never been a problem.”
I once heard a senior resident tell an intern:
“You don’t need to report those shifts. They’re not really ‘duty hours’ because they’re not for our program.”
That’s how bad habits pass down like family recipes, except the outcome isn’t cookies, it’s citations.
If you don’t want your career tied to someone else’s judgment:
- Ask for your program’s moonlighting policy in writing
- Ask GME for the institutional moonlighting policy
- Read the relevant section for your specialty in the ACGME Program Requirements
If anyone’s advice contradicts what’s written—PD, chief, senior resident—go with the written version and ask for clarification in email. Paper trails protect you.
Mistake #10: Letting Moonlighting Undermine Your Performance
This is the “soft” violation that becomes a hard problem when someone complains.
Even if you’re technically within all ACGME rules, too much moonlighting can show up as:
- Chronic tardiness for rounds
- Falling asleep in conference
- Sloppy notes, missed orders, more cross‑cover calls about your patients
- Worsening in‑service exam scores
Program directors are not dumb. When a resident suddenly gets more tired, more irritable, and strangely has nicer things than their peers, everyone puts two and two together.
And remember: ACGME requires that moonlighting must not interfere with the resident’s ability to achieve the goals and objectives of the educational program. That’s not vague. Your performance is part of compliance.
Even if the GME office never calls it a “moonlighting violation,” your PD can:
- Revoke moonlighting privileges
- Delay graduation if they feel your training was compromised
- Give you a professionalism or patient safety remediation plan
None of that is worth an extra check.
How to Moonlight Without Stepping on a Landmine
Let me flip this around. If you’re going to moonlight, here’s how you avoid becoming an ACGME horror story.
1. Get the rules from the source
Do this before you sign anything:
- Read your residency contract for any moonlighting clauses
- Ask GME for the institutional moonlighting policy
- Ask your PD:
- “Does our program allow internal moonlighting?”
- “Does our program allow external moonlighting?”
- “Are there PGY‑level limits?”
2. Get explicit, written PD approval
You want an email or signed form that covers:
- Whether you may moonlight at all
- Maximum hours per week
- Types of permissible settings
- Requirement to log all hours in the duty hour system
Save that email somewhere you can still find it in two years.
3. Log everything
Every hour of moonlighting goes in your duty hour system:
- No exceptions
- No “I’ll skip this one so the average looks better”
- No “this is more like volunteering” fantasies
If logging it makes the numbers break, the solution is to stop doing it. Not to stop logging it.
4. Check your weekly and 4‑week totals before saying yes
Quick mental check:
- What’s your typical residency hours this month?
- How many moonlighting hours are you adding?
- What does that do to your rough 4‑week average?
If your base rotation is already 70 hours/week, 16 hours/week of moonlighting is basically daring the system to flag you.
5. Protect real rest
Non‑negotiables:
- One true day off every week (averaged), with no moonlighting
- Respect the time‑between‑shifts rules for your specialty
If your only day off becomes a 12‑hour ED moonlighting shift every week, you’re not “hustling.” You’re eroding your margin of safety.
The Bottom Line
Three things I want you to walk away with:
- Moonlighting hours are duty hours. If you’re not willing to log them, you should not be doing them.
- Verbal “it’s fine” is not protection. Get written PD/GME approval, know your program’s actual policy, and stay inside it.
- Short‑term cash is not worth long‑term damage. A moonlighting gig that risks your ACGME compliance, visa, performance, or reputation is a bad trade—no matter how good the hourly rate looks.

















