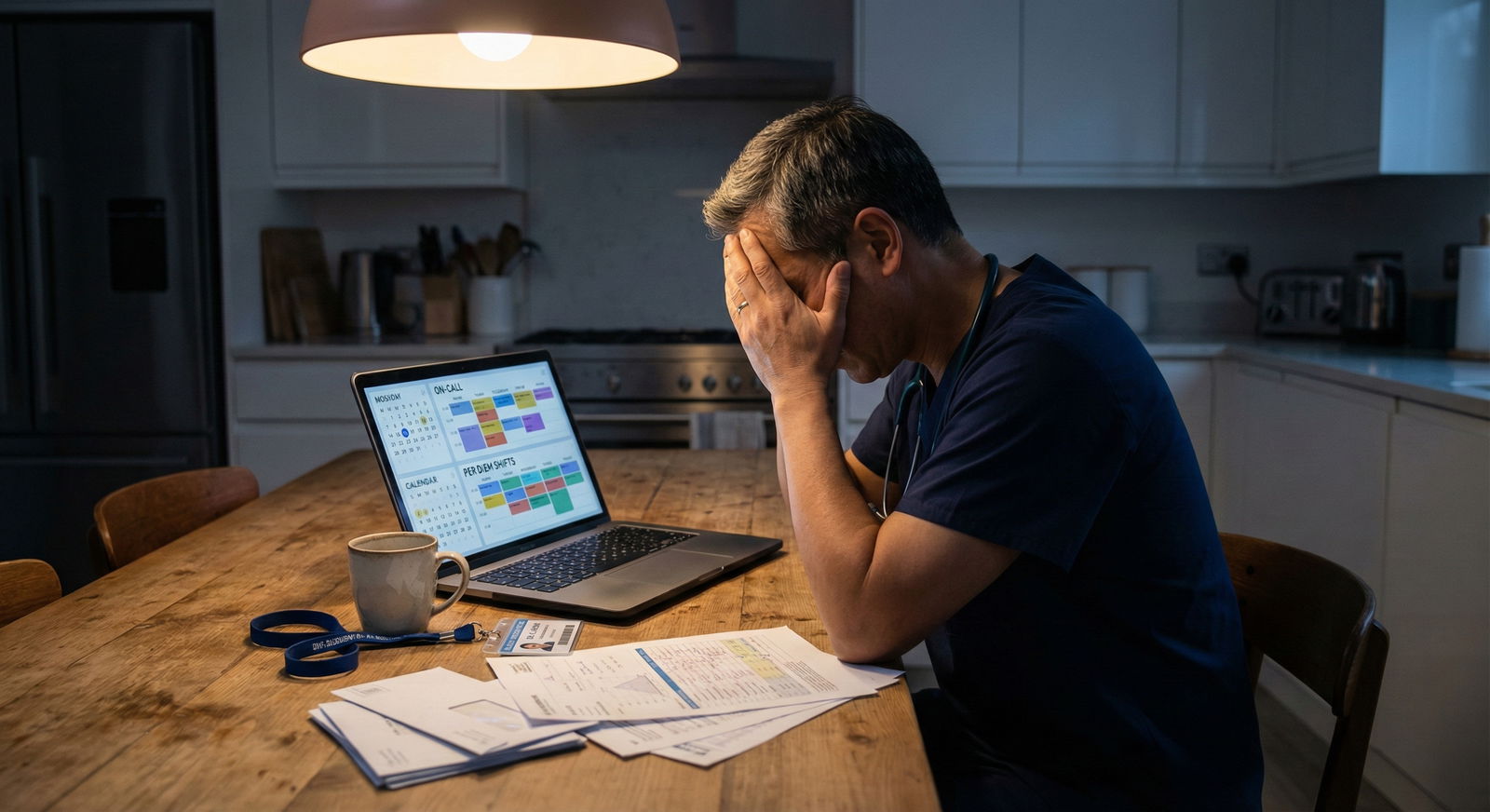
Saying yes to “easy” per diem money is how a lot of good clinicians quietly burn out or blow up their careers.
The mistake isn’t doing extra shifts. The mistake is acting like per diem work is free money with no real cost to your primary job, your reputation, or your long‑term future. It is not.
Let me walk you through the traps I see over and over. The stuff people only admit to privately, usually after something bad has already happened.
The Fantasy vs. The Reality of Per Diem Work
Per diem looks great on paper: flexible hours, high hourly rate, no long-term commitment, “just picking up a couple shifts.” You tell yourself:
- “It’s only weekends.”
- “It’s just for 6 months to pay off debt.”
- “I won’t let it interfere with my main job.”
That’s the fantasy.
The reality is different:
You’re not adding per diem to an empty schedule. You’re stacking extra hours on top of call, meetings, admin, EMR inbox, and the never‑ending “can you just…” from your main employer. You’re trying to squeeze a second job into the margins of a schedule that’s already marginal.
Here’s what people forget: fatigue, divided loyalty, and schedule complexity don’t care about your intentions. They wreck performance whether you “meant to let it affect your job” or not.
Mistake #1: Treating Your Main Job Like It’s Bulletproof
The fastest way to tank your primary job is to act like it’s guaranteed.
I’ve seen this play out in multiple hospitals: clinician picks up lucrative per diem work elsewhere, starts subtly favoring those shifts over their main employer—then looks stunned when their “secure” job evaporates.
How it shows up:
- Requesting schedule swaps at your main job to protect high‑pay per diem days.
- Coming in visibly tired on days after per diem night shifts.
- Saying “I can’t stay late, I have another shift” a few too many times.
- Turning down committee work or leadership tasks because “I’m already booked” (but that booked time is somewhere else).
Supervisors notice. Colleagues notice. Admin definitely notices.
They interpret it as:
- Less commitment
- Less availability
- Less reliability
Especially dangerous if you’re early in your career, new to the hospital, or still within any kind of probationary or partnership‑track period. You’re sending the exact opposite signal of what you think: not “motivated and hardworking,” but “split focus and future flight risk.”

| Category | Value |
|---|---|
| Highly committed | 5 |
| Neutral | 15 |
| Divided loyalty | 45 |
| Likely to leave | 35 |
If your main employer starts to see you as someone who’s halfway out the door, you’ve just turned your core job into a replaceable contract. Do not make that mistake unless you’re actually ready to walk.
Mistake #2: Underestimating Fatigue and Cognitive Slippage
One of the dumbest myths in medicine is, “I can handle it. I’ve done 28‑hour calls. I’m built for this.”
No, you’re not. Not indefinitely. Not with age. Not on top of a full‑time clinical load.
Per diem work often happens exactly when your body and brain need recovery:
- Nights
- Weekends
- Post‑call days (the “I’ll just go to the other hospital after I sign out” genius move)
- “Days off” that become 12‑hour shifts
Sleep debt is cumulative. Cognitive fatigue is real. And mistakes don’t show up as big, obvious errors at first. They start small:
- You miss one abnormal lab.
- You forget to document one key discussion.
- You’re a little shorter with a patient.
- You cut corners on charting “just this once.”
Then it escalates.
I’ve watched otherwise sharp clinicians:
- Show up to main job shifts already partly burned from a weekend moonlighting marathon.
- Confuse protocols between hospitals because they’re mentally flipping between different order sets and policies.
- Blank on which system to check for follow‑up because they saw the patient at one hospital, but are working at another, and are too tired to think straight.
You don’t get extra cognitive capacity just because the per diem shift pays $110/hour.
Most people only course‑correct after:
- A near‑miss that wakes them up.
- A peer quietly saying, “You okay? You seem off lately.”
- A formal performance conversation.
Avoid being that person. Build in absolute no‑work zones in your schedule, and honor them like your license depends on it—because eventually it might.
Mistake #3: Ignoring Contract Landmines and Non‑Competes
If you haven’t pulled out your employment agreement and actually read the moonlighting section, you’re playing with fire.
Common landmines:
- Non‑compete clauses that restrict working at competing facilities within a certain radius.
- Requirements to disclose any outside clinical work.
- Specific prohibitions on working for certain hospital systems or urgent care chains.
- Rules around telemedicine or cross‑state practice.
I’ve seen clinicians rationalize:
- “It’s just PRN at a SNF, they’ll never care.”
- “This urgent care isn’t really competing with the hospital.”
- “It’s telemed; it doesn’t count, right?”
Then one billing record, one patient complaint, or one gossip‑heavy nurse connects the dots—and suddenly HR is calling.
If your main employer finds out you:
- Violated a non‑compete
- Failed to disclose outside work as required
- Used their credentialing/reputation to obtain another gig without permission
you won’t get a polite warning. You’ll get a pointed conversation, if not a formal write‑up or contract non‑renewal.
Do not guess. Do not assume “everyone does it.” The people who get in trouble are usually the ones who thought it was too minor to matter.
Mistake #4: Letting Per Diem Warp Your Professional Reputation
Here’s what no one tells you: reputations travel between institutions a lot faster than you think.
If you’re per diem at Hospital B and employed full‑time at Hospital A, the staff overlap is real:
- Nurses who float between both.
- Specialists who consult at both.
- Administrators who know each other socially.
If you show up to per diem shifts exhausted, cranky, or disengaged because “this is just my side gig,” that bleeds back to your main job.
Common behavior that destroys credibility:
- Consistently leaving right at shift end no matter what’s going on (“I’m per diem, I’m not staying late”).
- Being less thorough because “this place isn’t my main responsibility.”
- Arguing about workload or assignments with language like “I’m just here to help, I’m not doing all that.”
People don’t compartmentalize your professionalism: “good at Hospital A, sloppy at Hospital B.” They just decide you’re that kind of clinician.
And then? When it’s promotion time, committee selection time, partnership track time, people remember the grumbling, the shortcuts, the half‑effort.
You might think you’re gaming the system—giving 100% to your main job and 70% to per diem. Outside eyes just see inconsistency. That hurts you in both places.
Mistake #5: Failing to Run the Math Like a Grown‑Up
The hourly rate on per diem shifts seduces a lot of people into bad decisions.
You glance at the rate:
- “$120/hour? I’d be stupid not to take that.”
- “One extra weekend a month could pay my car off early.”
But you don’t calculate the real cost.
You should be asking:
- How many hours of sleep will I lose before/after that shift?
- What’s the realistic impact on my energy and attitude in my main job next week?
- What am I sacrificing—exercise, family time, actual rest—that keeps me functioning at a high level?
- How much will this delay long‑term goals like board studying, research, networking, or leadership roles?
And then: what’s the tax effect? Per diem often doesn’t withhold correctly, you get hit with self‑employment tax or under‑withholding, and suddenly your “extra money” shrinks dramatically on April 15.
| Scenario | Gross Extra Income | Est. Taxes/Fees | Realistic Net | Hidden Cost |
|---|---|---|---|---|
| 2 shifts/month | $2,400 | $800 | $1,600 | 2 lost weekends of recovery |
| 4 shifts/month | $4,800 | $1,700 | $3,100 | Chronic fatigue, family strain |
| 6 shifts/month | $7,200 | $2,700 | $4,500 | Performance risk at main job |
Those numbers are rough but you get the point. You’re trading high‑value things—health, attention, long‑term opportunity—for short‑term cash that’s smaller than you think.
If you’re trying to fix bad financial decisions with more shifts instead of changing spending or planning, per diem becomes a band‑aid over a hemorrhage. And it keeps you trapped.
Mistake #6: Confusing Short‑Term Hustle With Long‑Term Strategy
This one is subtle but dangerous.
Someone will say: “I’m only doing this for a year to crush my loans.” Then two years later they’re still doing it, more burned out, less happy, not much richer, and completely stuck in golden handcuffs.
The pattern:
- Per diem boosts income.
- You adjust lifestyle upward to match.
- That new baseline now requires the extra income.
- Dropping per diem feels impossible without a “pay cut.”
- You double down instead of stepping back.
I’ve watched residents and early attendings moonlight so heavily they never build the CV that would actually buy them freedom: no QI projects, no leadership experience, no meaningful mentorship, no research. Just a string of shift counts and W‑2s.
When promotions, fellowship spots, or better jobs appear, they’re oddly underqualified—despite having worked a ton of hours—because they spent all their professional energy doing the highest‑pay, lowest‑growth work available.
You can absolutely use per diem strategically. But it has to be:
- Time‑limited.
- Purpose‑driven.
- Reviewed every 3–6 months with brutal honesty.
If you can’t clearly explain why you’re still doing it and what specific metric will tell you to stop, you’re not being strategic. You’re just working more by inertia.
Mistake #7: Botching Boundaries and Communication
One silent career killer: acting like your main job should “understand” or “accommodate” your per diem schedule.
Your primary employer owes zero loyalty to your side gigs.
Red flags that you’re messing this up:
- You ask your scheduler for specific days off to accommodate a per diem block schedule.
- You turn down main‑job opportunities because of pre‑booked per diem shifts.
- You “forget” to mention that you’re working post‑call somewhere else.
- You complain in the main job about being tired “because you were at X last night.”
To your colleagues, that sounds like: “I’m prioritizing other work over this team, and you all need to deal with the fallout.”
Do not weaponize your fatigue. Do not expect sympathy for exhaustion you chose.
If you’re going to do per diem, the burden is on you to:
- Schedule it strictly around your main responsibilities.
- Take the hit when there’s a conflict—per diem gets dropped, not your primary role.
- Keep your post‑per‑diem complaining to yourself, not your team.
You want to be seen as reliable, present, and committed where you earn your main paycheck. Anything that undermines that is expensive, even if nobody calls you out directly.
Mistake #8: Ignoring Malpractice, Credentialing, and Risk Stacking
More institutions, more risk. That’s the unsexy truth.
Each per diem site means:
- Another set of credentials.
- Another EMR system to keep straight.
- Another malpractice policy (or evidence that your current carrier knows exactly what you’re doing).
- Another stack of protocols, formularies, and unique “don’t ever do X here” rules.
The risk is not just one catastrophic error. It’s the accumulation of small vulnerabilities:
- Failing to document something in the per diem setting that later gets scrutinized.
- Ordering meds using one hospital’s dosing habits in another hospital’s system.
- Inconsistent follow‑up practices between sites that confuse patients—and regulators.
Worst‑case scenario: a bad outcome at a per diem job spills over to your main one, either via credentialing review, NPDB reporting, or just internal politics. You might think, “If something bad happens, at least it’s not at my main job.” That is fantasy. Your name and license are the same everywhere.
And if your primary employer finds out you’ve been practicing in higher‑risk or poorly supervised environments without disclosure? You’ve just handed them a ready‑made reason to distance themselves.
How to Do Per Diem Without Letting It Wreck You
I’m not saying “never moonlight” or “never do per diem.” I’m saying: stop treating it like a harmless side quest. If you’re going to do it, do it like a professional protecting their real asset—your main job and your long‑term career.

| Step | Description |
|---|---|
| Step 1 | Offered Per Diem Work |
| Step 2 | Do Not Accept |
| Step 3 | Disclose When Required |
| Step 4 | Recheck Every 3 to 6 Months |
| Step 5 | Read Contract and Policies |
| Step 6 | Clear Reason and Time Limit? |
| Step 7 | Schedule Protects Sleep and Main Job? |
Use something like that as your brain’s checklist, even if you never draw it out.
Ask yourself:
- Am I legally and contractually allowed to do this?
- Can I fully protect my sleep, my performance, and my primary schedule?
- Is this clearly temporary, with a defined end point?
- Am I willing to drop this instantly if my main job or health starts to slip?
If any of those answers are “no” or “ehh, I’ll figure it out,” that’s your warning. Do not override it just because the hourly rate looks pretty.
The Bottom Line
Three things to walk away with:
- Your main job is the asset. Per diem is a tactic. Don’t flip that hierarchy and then act surprised when your “side hustle” poisons the well.
- Fatigue, contracts, and reputation don’t care about your intentions. If you let per diem compromise any of those, your core career will pay the price.
- If you can’t do per diem in a way that protects your primary role, your sleep, and your long‑term goals, then you can’t afford the money—no matter what the rate is.

















