Most residents start moonlighting either too early and burn out, or too late and miss tens of thousands of dollars. You’re going to do better than that.
You want a clear, chronological answer: When is it actually safe to start moonlighting, and how do you plan for it from MS4 through PGY‑2? Let’s walk year by year, then month by month, then week by week.
Big Picture: The Earliest You Should Even Consider Moonlighting
Let me set a line in the sand:
- As an MD/DO, you do not moonlight as an MS4 or PGY‑1 intern. If you are thinking about it, stop.
- As a resident, you should not moonlight until:
- You’re fully licensed at the state level (not just training license).
- You’re comfortable independently managing common emergencies in your specialty.
- Your PD explicitly signs off.
- Your schedule has some predictable lighter stretches.
For most people in traditional 3–7 year residencies, that means:
- Earliest realistic start: Late PGY‑2 or early PGY‑3.
- Exception: Some prelim + advanced setups, anesthesiology, EM, hospitalist-heavy IM programs where people can start safely in late PGY‑2 if their training is strong.
So the question isn’t “Can I technically moonlight in PGY‑2?” It’s “How do I use MS4 → PGY‑2 to be ready by late PGY‑2 or PGY‑3 without risking my license, my sanity, or my fellowship chances?”
MS4: Set Up Future You, Don’t Chase Dollars Yet
You’re not moonlighting as an MS4. But you are making choices that will determine how early you can safely start later.
Fall of MS4 (ERAS season): Choose training that supports future moonlighting
At this point you should be:
- Looking at programs and asking blunt questions:
- “Do your residents moonlight?”
- “At what level do they typically start?”
- “Is there an institutional policy?”
- “Any restrictions based on visa status?”
- Paying attention to:
- Whether the program has:
- In-house resident-run services (night float, house officer roles).
- A culture of resident autonomy vs everything going through attendings.
- Graduates who talk about moonlighting in PGY‑3+.
- Whether the program has:
You want programs where:
- Residents actually moonlight (not just theoretically allowed).
- The PD has a clear, written policy.
- Senior residents aren’t all visibly wrecked and bitter from overwork.
Red flag: “We don’t formally allow moonlighting, but people find ways.” That’s how careers get wrecked.
Winter–Spring of MS4: Learn the business basics early
You’re not signing contracts yet, but you can quietly prep:
At this point you should:
- Spend 1–2 hours/month on:
- Understanding malpractice coverage types:
- Claims-made vs occurrence.
- Tail coverage.
- Basic financial literacy:
- How 1099 income works.
- Quarterly estimated taxes.
- Understanding malpractice coverage types:
- Keep a running note (Google Doc, Notion, whatever) titled:
“Future Moonlighting – Questions for Chief/PD”
Add to it when you hear attendings or residents talk about:- Hour caps.
- Dangerous moonlighting setups.
- Pay structures.
Result: When you’re finally allowed to moonlight, you won’t be the wide-eyed PGY‑2 asking what a W‑9 is.
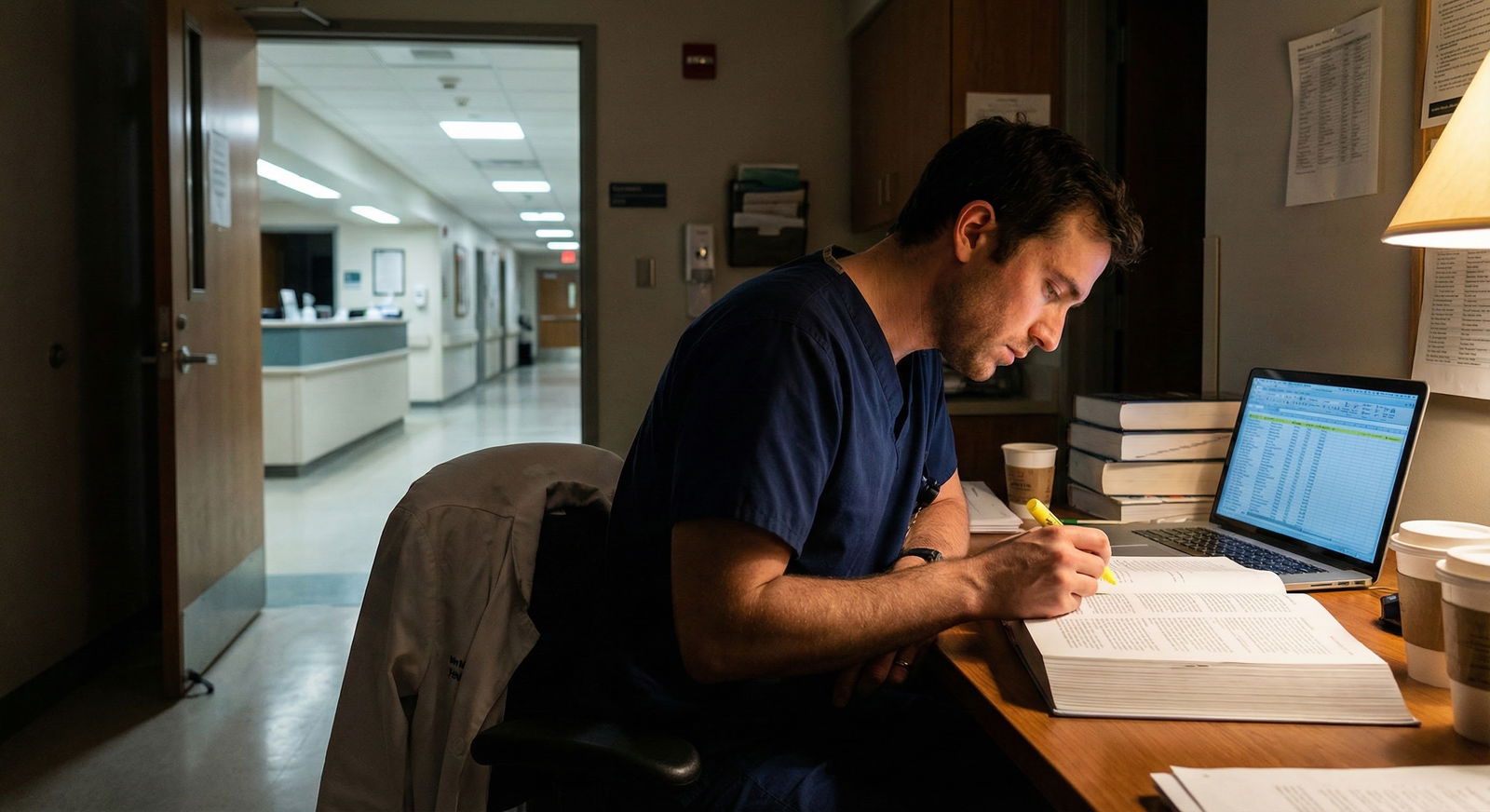
PGY‑1 (Intern Year): Build Competence, Not Side Income
Intern year is no-moonlighting territory in nearly all legitimate programs, for good reason. You’re barely keeping your head above water.
July–September (First 3 months): Survival and skill acquisition
At this point you should:
- Focus on:
- Getting fast and safe with:
- Admission H&Ps.
- Cross-cover calls.
- Overnight triage.
- Common emergencies in your field (e.g., hypotension, chest pain, acute dyspnea).
- Getting fast and safe with:
- Quietly observe:
- Which seniors are moonlighting.
- What kind of jobs they take (urgent care, telemed, ED fast track, floor coverage).
- Who looks stable vs who looks dead on their feet.
You’re not asking “How can I do that now?” You’re asking “What did they have to be comfortable with before they could safely do that?”
October–December: Clarify the rules on paper
By late fall of PGY‑1, once you’re not constantly lost, you can start asking targeted policy questions.
At this point you should:
- Find your institution’s GME moonlighting policy:
- Internal vs external moonlighting rules.
- Requirements for:
- Full license vs training license.
- PD approval.
- Duty hour tracking.
- Ask seniors specific, grounded questions:
- “When did you feel truly ready to moonlight?”
- “What cases did you still feel shaky on when you started?”
- “What would you do differently if you could start over?”
Capture their answers. They’re gold.
January–June (End of PGY‑1): Quiet preparation only
You’re still not moonlighting. But you can start lining up prerequisites.
At this point you should:
- Confirm licensure timelines for your state:
- When are you eligible for a full license?
- How long does processing usually take? (Ask PGY‑3s; they know the real number.)
- Make a tentative skills checklist for yourself:
- “Before I moonlight, I want to be solid at…”
- Managing common overnight calls independently.
- Running codes (or at least being a competent code team member).
- Handling basic procedures relevant to your field’s typical moonlighting (e.g., lac repairs, abscess I&D, simple airway decisions for EM/IM folks).
- “Before I moonlight, I want to be solid at…”
- Start a modest emergency fund:
- Goal by end of PGY‑1: at least 1–2 months of living expenses.
- Why? So you’re not forced into sketchy moonlighting because you’re broke.
Your mindset in PGY‑1: train like someone who plans to be safely independent in a couple of years. Which you do.
PGY‑2: The Planning and Licensing Year
PGY‑2 is where people get impatient and make bad choices. You’re going to pace it.
July–September of PGY‑2: Decide if moonlighting is even on your PGY‑2 radar
At this point you should:
- Honestly assess:
- How busy and malignant (or not) your program is.
- How fried you felt at the end of PGY‑1.
- Whether you’re on heavy rotations this year (ICU months, night float blocks, ED months).
- Ask yourself:
- “If I add 1–2 moonlighting shifts a month, will it:
- Jeopardize board studying?
- Push me over 80 hours when combined with residency?”
- “If I add 1–2 moonlighting shifts a month, will it:
- Talk to your PD or APD candidly:
- “I’m thinking about moonlighting later in residency. From your perspective, what milestones should I hit first?”
If your PD hesitates or says “Absolutely not in PGY‑2,” listen. They’ve seen residents crash and burn.
Licensure Timeline During PGY‑2
Most external moonlighting requires a full, unrestricted state license. That’s a bureaucratic slog. You plan backward.
At this point you should:
- Check your state’s requirements:
- Some need 1 year of postgraduate training.
- Some require Step 3/COMLEX Level 3 completion.
- Back-plan something like:

| Period | Event |
|---|---|
| Summer PGY2 - Jul-Aug | Confirm state requirements |
| Summer PGY2 - Aug-Sep | Schedule and study for Step 3 |
| Fall PGY2 - Oct | Take Step 3 |
| Fall PGY2 - Nov-Dec | Gather documents for license |
| Winter-Spring PGY2 - Jan | Submit full license application |
| Winter-Spring PGY2 - Feb-Apr | License processing |
| Winter-Spring PGY2 - May-Jun | Explore moonlighting options |
You don’t need this exact schedule, but you do need a schedule.
October–December of PGY‑2: Concrete prep and boundary setting
Once the licensure ball is rolling, you start formal planning.
At this point you should:
- Confirm institutional rules in detail:
- Are you allowed internal moonlighting (extra shifts at your own hospital)?
- Are you allowed external moonlighting (completely different hospital/system)?
- Maximum hours per week/month, including moonlighting, under ACGME:
- Create a personal cap that’s actually lower than the legal cap:
- Example: “No more than 16 extra hours per week averaged, and never after a 24‑hour call.”
- Start scouting types of moonlighting that match your skills and risk tolerance:
| Type | Typical PGY Level | Risk/Complexity |
|---|---|---|
| In-house cross-cover | Late PGY2–PGY3 | Moderate |
| Community hospitalist | PGY3+ | Higher |
| Urgent care | PGY3+ | Moderate |
| ED fast track | PGY3+ | Higher |
| Telemedicine | PGY3+ | Variable |
Your goal isn’t to start yet. It’s to avoid promising your future self 6 night shifts a month in a chaotic community ED as your first gig.
Late PGY‑2: When It Might Be Safe to Start (If Everything Lines Up)
Now we’re at the heart of your question.
If you’re going to start as a PGY‑2 at all, it’s usually in the second half of the year, and only if several boxes are checked.
Safety Checklist Before First Shift
At this point you should only start moonlighting if you can honestly say yes to most of these:
Clinical readiness
- “I can independently manage the top 10 scenarios I’ll see on this job.”
- “I know when to call for help and who that person is.”
- “I’ve run or co-run enough codes and rapid responses that I don’t freeze.”
Logistical readiness
- “I have:
- Full, unrestricted state license in hand.
- DEA number (if required).
- Malpractice coverage clearly documented in writing, including tail.”
- “I understand:
- Who is supervising me (if anyone).
- What happens if I get sued.
- How to report moonlighting hours for duty hour logs.”
Personal readiness
- “I’m not already living at constant exhaustion.”
- “I’ve talked this over with:
- My partner/family (if applicable).
- At least one senior resident who knows the specific job.”
- “I have an emergency fund so I’m not moonlighting out of sheer desperation.”
If several of those are no, you’re playing with fire starting in PGY‑2.
Choosing Your First Gig: Conservative > Sexy
Everybody loves to brag about big hourly rates in chaotic setups. Ignore that at first.
At this point you should aim for:
- Lower acuity, predictable environments:
- In-house cross-cover at your own institution.
- Low-acuity community hospital night coverage with backup available.
- Structure your first 3 months like this:
- Month 1: 1–2 shifts total.
- Month 2: 2–3 shifts total.
- Month 3: Max 3–4 shifts, then reassess.
Track everything: how you feel, how your day job performance changes, how your mood shifts.
How to Plan Week-by-Week Once You Start Moonlighting
Once you’ve begun, you need a system or you’ll quietly drift into burnout.
Weekly Structure Template
After you start moonlighting, a typical safe cap in PGY‑2 might look like:
- 1 moonlighting shift every 2 weeks during heavy rotations.
- 2–3 shifts/month during lighter rotations.

| Category | Value |
|---|---|
| Residency Clinical Hours | 200 |
| Moonlighting Hours | 24 |
| Study/Academic Time | 20 |
| Personal/Rest | 116 |
The point of the chart: if moonlighting hours crowd out sleep/personal time instead of non-essential fluff, you’re in the danger zone.
Before Each Month Starts
At this point you should:
- Look ahead at your residency schedule:
- Mark heavy months (ICU, nights) as no-moonlighting months.
- Mark lighter months (clinic blocks, elective) as potential moonlighting months.
- Pre-block:
- 1 completely off day per week – no residency, no moonlighting, no academic stuff if you can manage it.
- Sync with your PD’s expectations:
- If you’re on remediation, clerkship-style rotations, or struggling academically, you do not add moonlighting. Period.
Before Each Individual Shift
The day before every moonlighting shift, run a quick checklist:
- “Am I on call within 24 hours before or after this shift?”
- “Am I already pushing 70+ duty hours this week?”
- “Am I sick, emotionally drained, or behind on critical residency tasks?”
If you’re yes to any of these, cancel or reschedule if at all possible. Your residency performance is non-negotiable. Losing a moonlighting gig is cheaper than losing your spot.
Risk Management: How Not to Blow Up Your Career
Most moonlighting disasters follow the same pattern: young resident, new job, unclear supervision, exhaustion, and a bad case walking through the door at 3 a.m.
At this point—before you sign anything—you should:
- Read the contract yourself, then have:
- A senior who has worked there review it.
- Optionally a physician-side attorney look at any red flags.
- Clarify in writing:
- Who provides malpractice and what limits.
- Whether moonlighting counts as “independent practice” versus “under attending.”
- What patient volume is expected (per hour/shift).
Dead-simple safety questions to ask the site:
- “If I’m over my head clinically at 2 a.m., who do I call?”
- “Am I the only physician in-house?”
- “Do I have admitting privileges, and who are the backup attendings?”
If they dodge or gloss over these, walk.
Financial Plan: What to Do With the Extra Money
If you’re going to sacrifice time and sleep, at least make the money work for you.
At this point you should:
- Decide a written rule for moonlighting income, for example:
- 50% → high-interest debt (credit cards, personal loans).
- 25% → emergency fund or future down payment.
- 25% → lifestyle (travel, nicer apartment, childcare help).
- Never rely on moonlighting money to cover your bare minimum monthly expenses. That’s how you get trapped saying yes to unsafe shifts.
Treat moonlighting income as accelerator money, not survival money.
Red Flags That You Started Too Early
If any of this starts happening after you begin moonlighting in PGY‑2, you need to back off:
- You’re nodding off on residency rounds.
- Errors or near-misses creep into your main job.
- Your evaluations suddenly mention “attention to detail,” “professionalism,” or “availability.”
- You stop studying entirely because there’s no time left.
- Your relationship(s) are falling apart and you’re constantly irritable.
At that point, the question isn’t “Should I adjust my moonlighting schedule?” It’s “Do I stop entirely for 3–6 months and re-evaluate?” The answer is usually yes.
Quick Phase-by-Phase Summary
Here’s the chronological backbone, condensed:
MS4
- Choose programs with clear moonlighting policies.
- Learn basics of licensing, malpractice, and 1099 income.
- Do not chase under-the-table work. Not worth it.
PGY‑1
- Zero moonlighting.
- Build clinical competence and speed.
- Understand your institution’s formal policies.
- Start small emergency fund.
Early PGY‑2 (Jul–Dec)
- Decide if moonlighting is even plausible this year given your program.
- Plan licensure and Step 3 timeline.
- Set personal hour caps and non-negotiable “no moonlighting” months.
Late PGY‑2 (Jan–Jun)
- Only start moonlighting if:
- Fully licensed.
- Malpractice is clear.
- PD explicitly approves.
- You’re clinically solid and not drowning already.
- Begin with low-acuity, conservative gigs.
- Limit to 1–3 shifts/month initially, track the impact.
FAQ (Exactly 3 Questions)
1. Can I moonlight as a PGY‑1 if I find a place that will hire me?
You shouldn’t. Even if someone is willing to use you as cheap coverage, you’re exposing yourself to massive clinical and legal risk when you’re least prepared. Most legitimate programs and GME offices explicitly ban PGY‑1 moonlighting. If a place is eager to hire an intern unsupervised, that’s a neon sign that their risk tolerance is insane. Walk away.
2. Is internal moonlighting always safer than external?
Not always, but usually it’s a better starting point. Internal gigs often come with systems you already know, EMR you already use, backup attendings you recognize, and a culture that aligns with your residency. External gigs can pay more but introduce new systems, unknown colleagues, and sometimes looser oversight. For your first 6–12 months of moonlighting, I strongly prefer internal or closely affiliated sites.
3. Will moonlighting hurt my chances for fellowship?
Moonlighting itself doesn’t hurt you. Slipping performance does. If your in-service scores drop, your research stalls, or faculty notices you’re half-present because you’re working extra nights, that will absolutely hurt your fellowship prospects. If you’re fellowship-bound in a competitive field, either delay moonlighting until PGY‑3+ or keep it extremely light and transparent with your mentors.
Open your calendar for the next 18 months right now and mark three things: your likely Step 3 window, your earliest possible licensure date, and the rotations where you absolutely will not moonlight. That’s your starting framework. Everything else gets built around those anchors.

















