The belief that “everyone moonlights as a PGY‑2” is wrong. And buying into it blindly is one of the fastest ways to burn out, screw up your training, or put your license at risk.
Let’s dismantle this the way it should be dismantled: with data, policy, and a cold look at incentives.
The Myth vs Reality: Who Actually Moonlights?
Residents talk about moonlighting like it is some universal rite of passage. “Once you hit PGY‑2, you’ll moonlight, pay off your credit cards, and finally breathe.” I have heard versions of that speech at orientation, in call rooms at 3 a.m., and from attendings trying to be “real” with their teams.
But here is what the data and policies actually show:
- Many large academic programs either heavily restrict or completely prohibit moonlighting for PGY‑2s.
- A significant number of residents never moonlight at all during training.
- Where moonlighting is allowed, only a subset of residents actually do it regularly, and an even smaller subset makes “big money” from it.

| Category | Value |
|---|---|
| Big Academics | 20 |
| Community Programs | 55 |
| University Affiliated | 40 |
| Rural Programs | 60 |
These are rough patterns pulled from surveys, GME reports, and specialty organization discussions—not fantasies from the call room:
- Large academic IM and surgical programs: often <25% of residents moonlight at all, and many only in PGY‑3+.
- Community IM/FM/EM/psych programs: far more moonlighting, sometimes >50%, usually later in residency.
- Highly procedural or high‑acuity specialties (surgery, OB, anesthesiology): moonlighting is less common and more tightly regulated, often due to malpractice and competency concerns.
So no, “everyone” does not moonlight PGY‑2. The people who say that often:
- Trained in a very specific type of program (often community or lower‑acuity), and
- Are compressing multiple years into one narrative (“I moonlighted a ton in residency” = mostly PGY‑3+), and
- Are remembering the money, not the tradeoffs.
The Rules That Actually Govern Moonlighting (Not the Stories)
This is the part most residents do not bother to read, then act surprised when they get smacked by GME or the ACGME.
There are three overlapping rule sets that matter:
- ACGME requirements
- Institution and program policies
- State licensing and malpractice rules
1. ACGME: The 80‑Hour Problem
The ACGME does not care how badly you want to pay your loans. It cares about duty hours and supervision.
Key facts:
- Moonlighting counts toward the 80‑hour work week. Internal or external. If a PGY‑2 tells you, “My moonlighting doesn’t count toward my duty hours,” they are either misinformed or admitting a violation.
- Programs are explicitly responsible for monitoring all clinical work, including moonlighting, to ensure compliance.
- Residents must not be assigned to moonlighting if it interferes with their educational experience or well‑being. That’s not “guidance.” That’s a requirement.
When residents “forget” to log moonlighting hours, they put the program at risk. When programs look the other way, they are playing chicken with citations and accreditation.
2. Institutional and Program Policies
Here’s where the myth really dies. Pull up the moonlighting policy for a few big‑name programs and compare.
| Program Type | PGY‑2 Moonlighting | Typical Restrictions |
|---|---|---|
| Big academic IM | Usually no | PGY‑3+ only, internal only |
| Community FM | Often yes | Good standing, PD approval |
| EM at county hospital | Sometimes | Minimum shift count, PD sign‑off |
| Surgical residencies | Rare | Often prohibited entirely |
Common institutional rules:
- Must be in good academic standing (no remediation, no professionalism flags).
- Must have full state license, not just training license, for many external jobs.
- Must carry separate malpractice coverage for external moonlighting.
- Must get program director approval in writing before starting.
If you are being told, “Everyone just picks up some extra shifts; it’s not a big deal,” and none of this is documented, you are walking into a regulatory minefield.
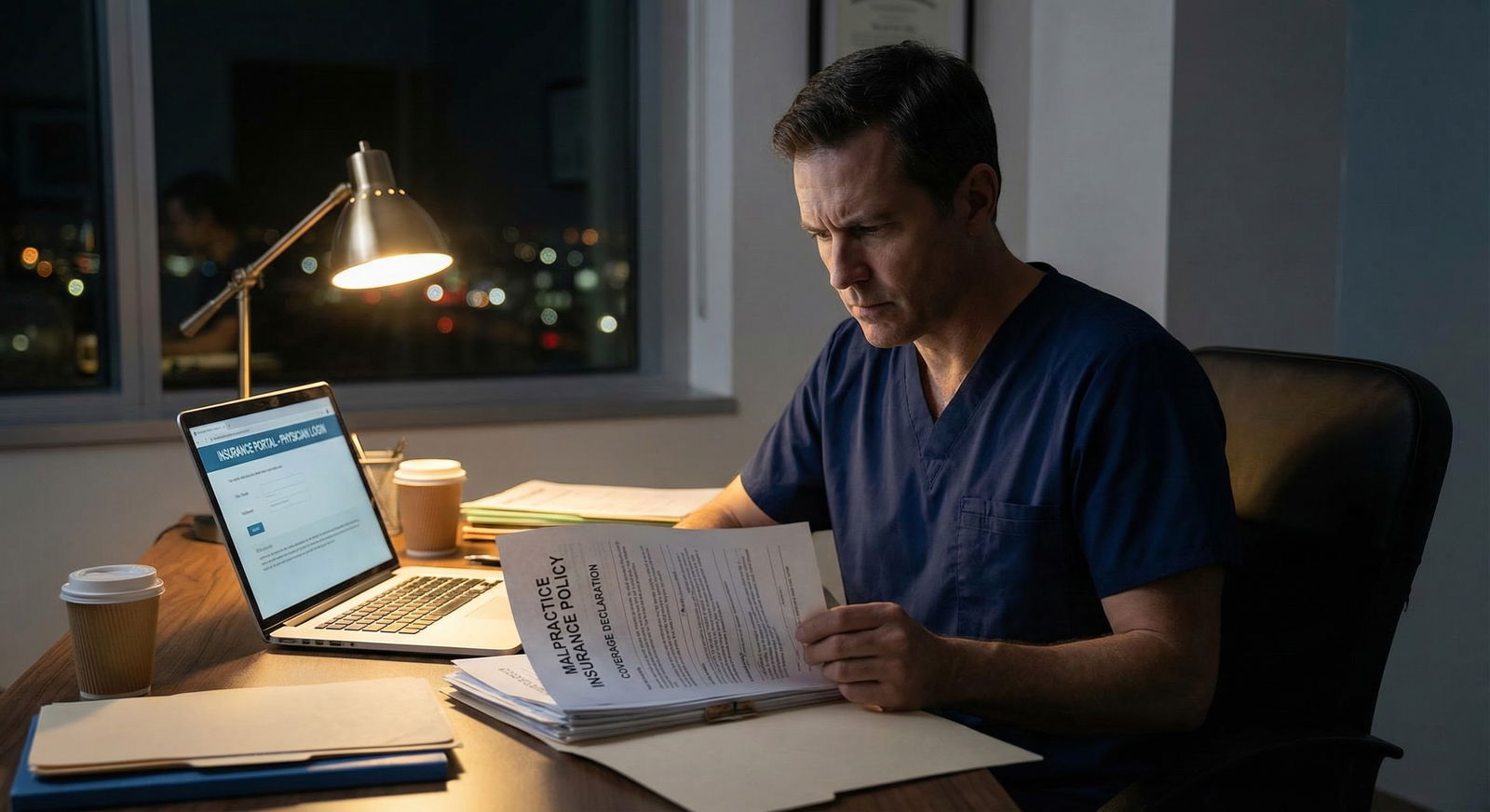
3. Licensing, Billing, and Malpractice
Another inconvenient fact: you are not a cheap attending. You are a trainee, and that has billing and liability consequences.
Three common traps:
- Working on a training license in an external job that actually requires a full, unrestricted license. That can be a licensing violation.
- Assuming your training program’s malpractice covers outside work. Often it does not. Many hospital policies explicitly exclude moonlighting.
- Working beyond your documented competence (example: PGY‑2 IM doing solo ED coverage in a small hospital with no attending on site). If something catastrophic happens, plaintiff attorneys will have fun with that.
I’ve seen residents discover during a lawsuit that nobody really knew whose malpractice policy applied to their moonlighting shifts. You do not want to be that case.
The Money: Helpful Boost or Overhyped Side Hustle?
Let’s talk about why people do this in the first place: money.
PGY‑2 salaries in the U.S. are often in the $62k–$70k range base, depending on region. Moonlighting rates vary wildly:
- Low acuity inpatient or outpatient: $60–$100/hour
- ED coverage in small hospitals, cross‑cover: $100–$150/hour
- Procedure‑heavy or high‑acuity roles: sometimes more, sometimes with nasty catch‑up expectations

| Category | Value |
|---|---|
| Low-acuity clinic | 70 |
| Inpatient cross-cover | 90 |
| Small community ED | 120 |
| Rural ED solo coverage | 160 |
On paper, if you pick up 16 hours a week at $100/hr, that is $1,600/week, or roughly an extra $6,400/month before taxes. Sounds life‑changing.
Reality:
- Federal + state + FICA will carve off a large chunk. Effective marginal tax rate could be 30–40% depending on your situation.
- You are paying that tax on more fatigue, more risk, and often worse hours than your training shifts.
- Many residents cannot actually sustain 16 extra hours weekly without their performance dropping somewhere else—usually in their primary job or their health.
Reasonable, sustainable patterns I see more often:
- 1–2 shifts per month used to cover specific expenses (childcare, a car payment, minimum loan payments).
- A few months of heavier moonlighting near the end of residency while boards and job offers are already secured.
The people who do 40–60 hours of moonlighting on top of full‑time residency? They exist. They are also rolling the dice on mistakes, citations, and burnout. Survivorship bias is loud here; the ones who flamed out are not at the reunion bragging.
When You Actually Should Say No (Even If You Need Money)
This is the part nobody says out loud on that “residents as financial hustlers” side of social media.
There are situations where a PGY‑2 saying “yes” to moonlighting is honestly just a bad decision. Not morally. Logistically, educationally, even legally.
Here are the big red flags.
1. Your Core Training is Not Solid Yet
If any of these are true, moonlighting is usually premature:
- You are struggling to independently manage typical patients at your own level.
- You need frequent attending backup on routine decisions.
- You have had recent feedback about medical knowledge gaps, time management, or clinical judgment.
- You are on any kind of remediation plan, formal or informal.
Moonlighting assumes you can safely function with less support than you have at your day job. If you are still leaning hard on your attending and seniors, you have no business flying solo in someone else’s hospital or clinic.
2. Your Hours Are Already Maxed Out
If you are regularly:
- Hitting the 80‑hour cap even without moonlighting,
- Coming in early / staying late off the clock to finish notes,
- Using your “days off” to catch up on sleep and basic life tasks,
then layering moonlighting on top is not impressive. It is reckless.
Residents tell themselves, “It’s only a few more hours.” But those “few hours” are never truly free—your body will reclaim them somewhere. Usually in the form of mistakes, slowed cognition, or crashing on a day you needed to study.
3. It Compromises Key Rotations or Your Future Plans
If you are in any of these situations, I’d be very cautious:
- You’re applying to a competitive fellowship and currently on showcase rotations (ICU, subspecialty months) where evaluations matter.
- You are in the ramp‑up period before a major exam (Step 3, specialty in‑training exam, board prep).
- You are learning high‑risk procedures or working in new settings that already stretch your bandwidth.
I’ve watched residents tank fellowship‑critical rotations because they were fried from nights at an outside ED. The short‑term cash did not compensate for the long‑term hit.
4. The Job Itself Is Sketchy
Some moonlighting gigs are flat‑out inappropriate for a PGY‑2, no matter your confidence level:
- Solo ED coverage in a hospital with no in‑house attending backup and minimal subspecialty support.
- “Hospitalist” roles where you are effectively the attending of record with minimal oversight and volumes that would strain a seasoned attending.
- Positions where the job description is vague, malpractice coverage is “we’ll figure it out,” and nobody wants to send you the contract in writing.
If the setup sounds like something people brag about in anonymous forums but attendings raise an eyebrow when you describe it, pay attention to that second group.
A Rational Framework for Deciding About Moonlighting in PGY‑2
Instead of “everyone does it” or “never do it”, you need a structured way to decide.
Think in four domains:
- Training
- Health
- Regulatory/Legal
- Financial

| Step | Description |
|---|---|
| Step 1 | Thinking about moonlighting |
| Step 2 | Do not moonlight |
| Step 3 | Probably wait |
| Step 4 | Limited, structured moonlighting |
| Step 5 | Program allows it for PGY 2 |
| Step 6 | In good standing and solid clinically |
| Step 7 | Can stay under 80 hours and rest |
| Step 8 | Job has clear coverage and malpractice |
| Step 9 | Money solves specific problem |
Walk through each:
Training:
Are you objectively strong at your current level? Ask senior residents and attendings you trust. If the answer is “not yet” or “getting there,” your priority is training, not extra work.
Health:
Track your duty hours honestly for a few weeks. If you are already near 70–80 hours with call and “informal” work, you do not have room for moonlighting without violating rules or wrecking yourself.
Regulatory/Legal:
Do you have, in writing:
- PD approval?
- Confirmation that hours will count and be monitored?
- Proof of malpractice coverage?
- Clarity on your license status for that job?
If any of those are fuzzy, the correct answer is no.
Financial:
This is where people lie to themselves. Do not just think “more money good.”
Ask:
- What very specific problem am I solving with this money? (“Pay off the 26.99% APR credit card over 6 months” is valid. “I just want more cushion” is vaguer.)
- Can I accomplish the same goal with fewer shifts over a longer period?
- Have I already cut the low‑yield bleeding from my budget (random subscriptions, expensive commutes, eating out constantly) before I sell away my limited free time?
Moonlighting makes sense when the financial upside is concrete and time‑limited, not just because everyone’s doing it.
The Social Pressure Problem: You Don’t Have to Imitate the Loudest Resident
One last myth to kill: “If you are not moonlighting, you are leaving money on the table and being dumb.”
No. You are trading one scarce resource (time, sleep, recovery, actual learning) for another (cash). That is a trade. Not an obvious win.
The residents who talk the loudest about moonlighting often:
- Are weirdly proud of suffering.
- Like projecting an image of being ultra‑competent and in demand.
- Have normalized exhaustion to a degree that is not healthy.
You do not see their sleep tracker. You do not see their notes backed up. You do not see the near misses they never reported. You definitely do not see what their performance reviews actually say.
Years from now, nobody will care how many moonlighting shifts you did in PGY‑2. They will care if you are a competent attending, not burned out, and not carrying the weight of one bad outcome you were too tired to prevent.
FAQs
1. Is there any situation where moonlighting as a PGY‑2 actually makes good sense?
Yes, but it is narrower than people admit. Example: your program clearly allows PGY‑2 moonlighting; you are strong clinically, consistently under 60–65 hours/week; the moonlighting shift is low‑acuity, well supervised, with explicit malpractice coverage; and you have a defined, time‑limited financial goal (e.g., paying off one toxic debt over 6–12 months). In that scenario, a small, controlled number of shifts can be reasonable.
2. What if my co‑residents are all moonlighting and I feel like I am falling behind financially?
You are not seeing the full picture of their debt, support systems, or what is slipping in their lives. If your long‑term career or health takes a hit because you kept up with their short‑term cash grab, you lose that trade. You can always moonlight more as a senior or as an attending; you cannot retroactively fix a damaged training experience or a burnout spiral.
3. How do I safely bring this up with my program director?
Be direct and structured. “I’m considering limited moonlighting. Our policy says PGY‑2s may be eligible. Here is my current average duty hours, my evaluations, and the specific job details including coverage and malpractice. Do you think this is appropriate for me now?” A good PD will appreciate the thoughtfulness—and might tell you “not yet” with reasons that actually help you.
4. Is it ever okay to not log moonlighting hours if my program unofficially expects it?
No. That is how you end up with ACGME violations, dishonest reporting, and a very ugly conversation if something goes wrong. If the only way the gig works is by pretending those hours do not exist, the gig is incompatible with your actual job and regulatory environment. Walk away.
Years from now, you will not remember the exact amount you made from a few extra shifts. You will remember whether training made you into the kind of physician you trust yourself to be—and whether you protected that process when it counted.

















