
Moonlighting is not a moral failing. But it can absolutely be perceived as one if you’re not careful—and that’s what keeps people like us up at 2 a.m. refreshing our email.
You’re not crazy for worrying about this. I’ve heard versions of your question whispered in workrooms, muttered in elevators, and texted in group chats after a rough ward month:
“If I moonlight, are they going to think I care more about money than my training?”
“Will my PD think I’m not a ‘team player’?”
“What if something goes wrong while I’m moonlighting—does that nuke my career?”
Let’s pick this apart in a way that actually addresses the worst-case scenarios you’re afraid of, not just the sanitized “it’s fine if you’re responsible” line everyone throws around.
The Ugly Truth: Some People Will Judge You
I’m not going to sugarcoat this. There are attendings and program directors who see moonlighting and instantly think:
- “They’re burned out and just chasing money.”
- “If they have time to moonlight, they’re not working hard enough here.”
- “I didn’t moonlight and I turned out fine—why can’t they just live on their salary?”
Is this fair? No.
Is it real? Yes.
The problem isn’t moonlighting itself. It’s the story people tell themselves about your moonlighting.
If the story in their head is:
“This resident is crushed with 70–80 hour weeks and still adding more shifts for fun,” that reads as unsafe, impulsive, maybe even reckless.
If the story is:
“This resident is on a lighter elective month, is hitting all their milestones, and is picking up a supervised urgent care shift once or twice a month,” that reads very differently.
The fear we have—the fear you have—is that no matter what, they’ll default to the worst version of the story. That they’ll assume you’re uncommitted, distracted, or “not all in” on your residency.
But they don’t all think that way. And the ones who might are usually the ones who:
- Had a very different training system
- Don’t fully grasp current resident salaries vs cost of living
- See any sign of boundary-setting as “weakness” or “entitlement”
You can’t control who they are. You can control how you show up and how clearly you link moonlighting to responsible, adult decision-making instead of desperation or greed.
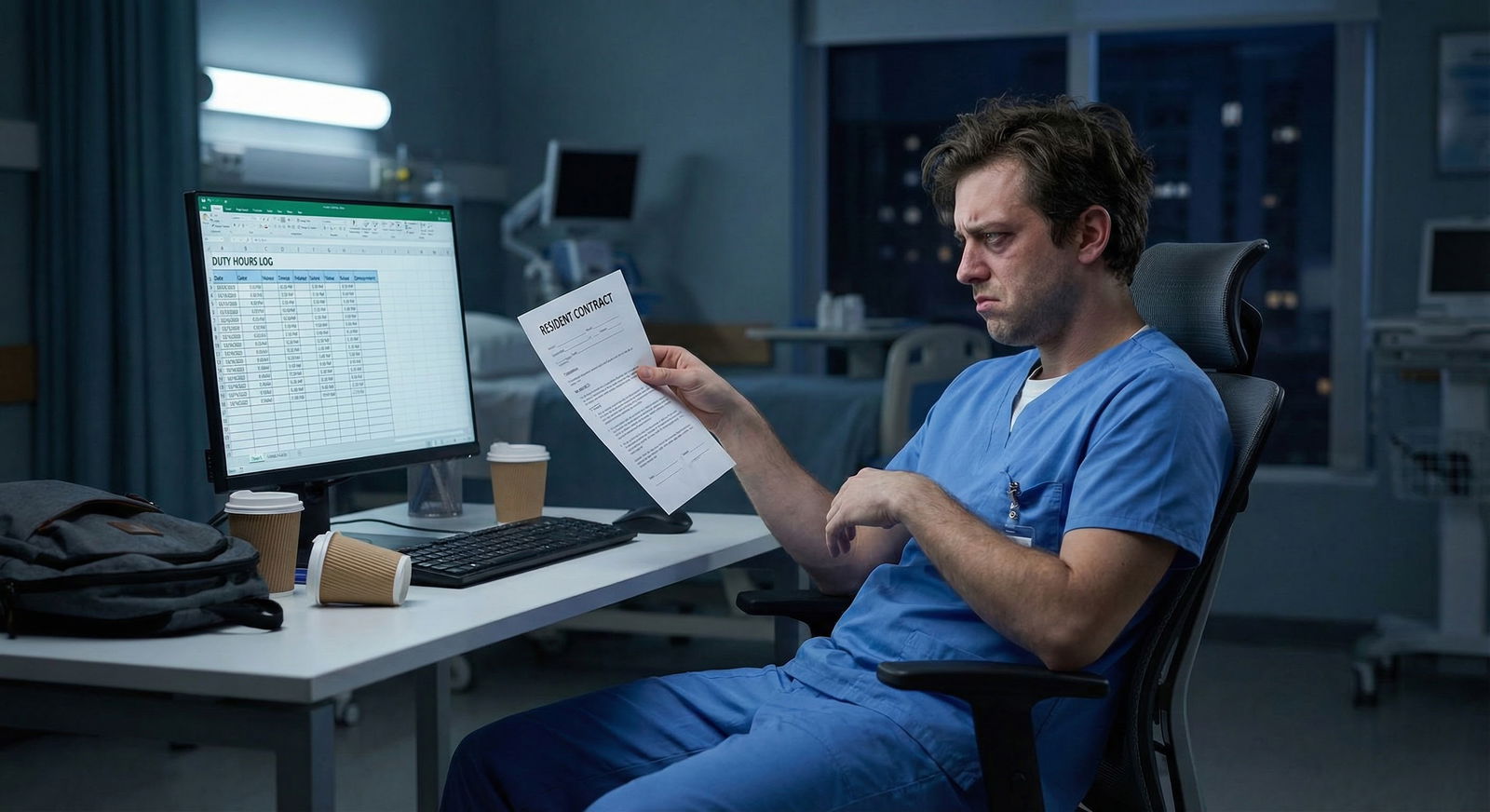
What Programs Actually Care About (Behind the Passive-Aggressive Policies)
Most programs don’t wake up in the morning thinking, “How can we ruin resident lives and stop them from earning extra?” Their real fears are more basic and, honestly, kind of understandable.
They’re worried that moonlighting will:
- Interfere with your duty hours and put them at risk with the ACGME.
- Drag down your performance—late notes, missed follow-up, slower on rounds.
- Increase patient safety risk if you’re showing up to your actual job exhausted.
- Lead to liability issues if something goes wrong and they’re somehow dragged into it.
- Create optics problems: resident bragging about $150/hr shifts while the PD is fighting for small raise increases.
So when you’re terrified that they’ll see you as uncommitted, what they’re really scanning for is:
- Has your performance slipped?
- Are faculty or co-residents complaining?
- Are your evaluations getting weirdly vague and chilly?
- Are you ever “unavailable” to your actual program because of outside work?
- Are you honest about your hours, or playing games with duty hour reporting?
They don’t care that you want to afford rent or pay off $300k in loans. They care whether your extra work creates new headaches for them.
Uncommitted, in their eyes, often translates to:
Unreliable. Tired. Sloppy. Harder to manage.
That’s what you actually have to avoid.
The “Red Flag” Version of Moonlighting vs The Safe Version
Let me divide this into two simple mental buckets, because this is where your worry really lives: “Which one do I look like?”

The red flag version (this is the nightmare you’re imagining)
This is how it looks when moonlighting does make someone appear uncommitted:
- They take overnight moonlighting shifts right before busy clinic/ward days.
- They start rolling into conference late or obviously exhausted.
- Notes and tasks pile up on their service because “I was on a moonlighting shift last night.”
- They miss didactics or mandatory events “due to scheduling mix-ups.”
- Faculty start making comments like, “They’re always hustling for extra shifts, but their notes are never done.”
- Other residents notice and begin resentfully saying things like, “We’re covering more because they’re never fully present.”
In that world, moonlighting isn’t just “extra work.” It’s pulling visible energy and attention away from your main job. That looks like lack of commitment, whether you intended it or not.
The safe version (what you’re secretly hoping is possible)
Here’s where moonlighting usually doesn’t get people labeled as uncommitted:
- They ask permission and follow all the program rules.
- They choose shifts on lighter rotations, not on ICU or wards months.
- They limit to occasional shifts that don’t trash their sleep schedule.
- Their evaluations stay strong or even improve.
- Their notes are done, patients are managed, and there are no complaints.
- They’re still showing up to conferences and participating like a normal human.
Same behavior (moonlighting), totally different pattern of consequences. Your fear is about getting lumped into the first bucket when you’re planning to live in the second.
How to Moonlight Without Looking Like You Don’t Care About Training
You’re scared because the line feels invisible. So let’s make it visible.
1. Be obnoxiously clear about program rules
I mean print them or screenshot them. Ask the chief or PD to clarify anything fuzzy, before you sign anything externally.
Look for:
- Whether moonlighting is allowed at all
- PGY level requirement (often PGY-2+)
- Whether you need written approval from PD or GME
- Whether internal moonlighting counts toward duty hours (almost always yes)
- Whether external moonlighting is even allowed (sometimes banned)
“Looking uncommitted” often starts with “looking sneaky.” If they find out from someone else that you’ve been moonlighting without telling them? That’s instant trust damage.
2. Tie moonlighting to a rational, adult reason
You don’t owe anyone your full financial trauma, but a calm, mature explanation helps reframe how people perceive it.
For example:
“I’m looking at one or two supervised urgent care shifts a month. My main goal is to build more confidence managing low-acuity outpatient issues independently, and the extra income will help with my loan payments. I’m planning to keep it limited to lighter months and off-call weekends.”
That doesn’t sound like “I hate my program” or “I don’t care about my training.” It sounds like you’re aware of tradeoffs and still centering your main job.
3. Protect your core performance like your career depends on it (because it does)
If you moonlight and your evaluations are stellar, few people will care. If you moonlight and start slipping, suddenly everyone will blame the moonlighting.
So before you even sign up for a shift, ask yourself, very brutally:
- Are my current evals solid or shaky?
- Am I already hanging on by a thread with fatigue, notes, or burnout?
- Would one more thing push me into doing noticeably worse?
If you’re already not sleeping, already behind on notes, already getting “concerned” comments on evaluations, moonlighting will not read as “committed but busy.” It’ll read as denial.
What If They Already Think I’m Uncommitted?
This is the nightmare loop: “What if I do everything right and they still assume the worst about me, just because I’m moonlighting at all?”
Here’s the uncomfortable reality: someone, somewhere, probably will judge. You don’t control every attending’s private opinion.
What you can do is make it incredibly hard for that opinion to stick in any way that matters.
You do that by:
Being proactive instead of hiding.
“I wanted to run my plan by you and make sure you don’t have concerns about my performance or schedule.”Asking for honest feedback.
“If at any point you see my performance slipping or hear concerns, I want to know immediately, and I’ll cut back or stop.”Checking in after you start.
“I’ve been moonlighting one or two times this month. Any feedback about how things are going on service or any concerns I should address?”
That last part does two things:
It shows you’re self-aware and that residency actually comes first. And it forces them to either say “No concerns” (which you can mentally bank) or give you early warning before rumors and narratives build behind your back.
What if Something Goes Wrong When I’m Moonlighting?
This is the real 3 a.m. fear: “What if there’s a bad outcome, a complaint, a lawsuit—am I suddenly ‘that resident who shouldn’t have been moonlighting’ forever?”

| Category | Value |
|---|---|
| Being judged | 80 |
| Burnout | 70 |
| Liability | 65 |
| Duty hours | 60 |
| Skill level | 55 |
You’re not imagining it—there is risk. But it’s not binary “career survives vs career explodes.” It’s more nuanced.
To not look reckless or uncommitted if something does go wrong:
- Make sure you’re properly credentialed and insured. No shortcuts, no assumptions.
- Work within your skill level. Don’t agree to manage things you know you’re shaky on just because the pay is good or the site is desperate.
- Keep records of approvals—emails from PD or GME, contracts, malpractice info.
If a bad outcome happens and you were moonlighting within the rules, at a reasonable volume, with strong performance in residency, that is very different from secretly taking unsafe shifts while bombing your home program.
Your fear is that one decision will permanently stain how committed you look. The real danger is a pattern. You control that pattern.
How Much Moonlighting Is “Too Much” Before It Does Look Bad?
Nobody gives you a hard number because it totally depends on your program, your specialty, and your baseline workload.
But if you want a gut-check threshold, I’d say:
- If you’re regularly bumping against or over 80 hours/week between residency and moonlighting—even if you’re “technically” logging 80 or less—you’re in dangerous optics territory.
- If anyone has to pick up slack for you because you’re tired, delayed, or overextended from moonlighting, that’s already too much.
- If you feel your attention fracturing—thinking about moonlighting logistics while on rounds, or rushing through notes so you can get to an outside shift—it will eventually show.
The uncommitted label doesn’t show up on week one. It shows up when people see a pattern of you treating residency as the thing you squeeze in around your side job.
If your behavior never even hints at that, most people won’t go out of their way to invent that narrative about you.
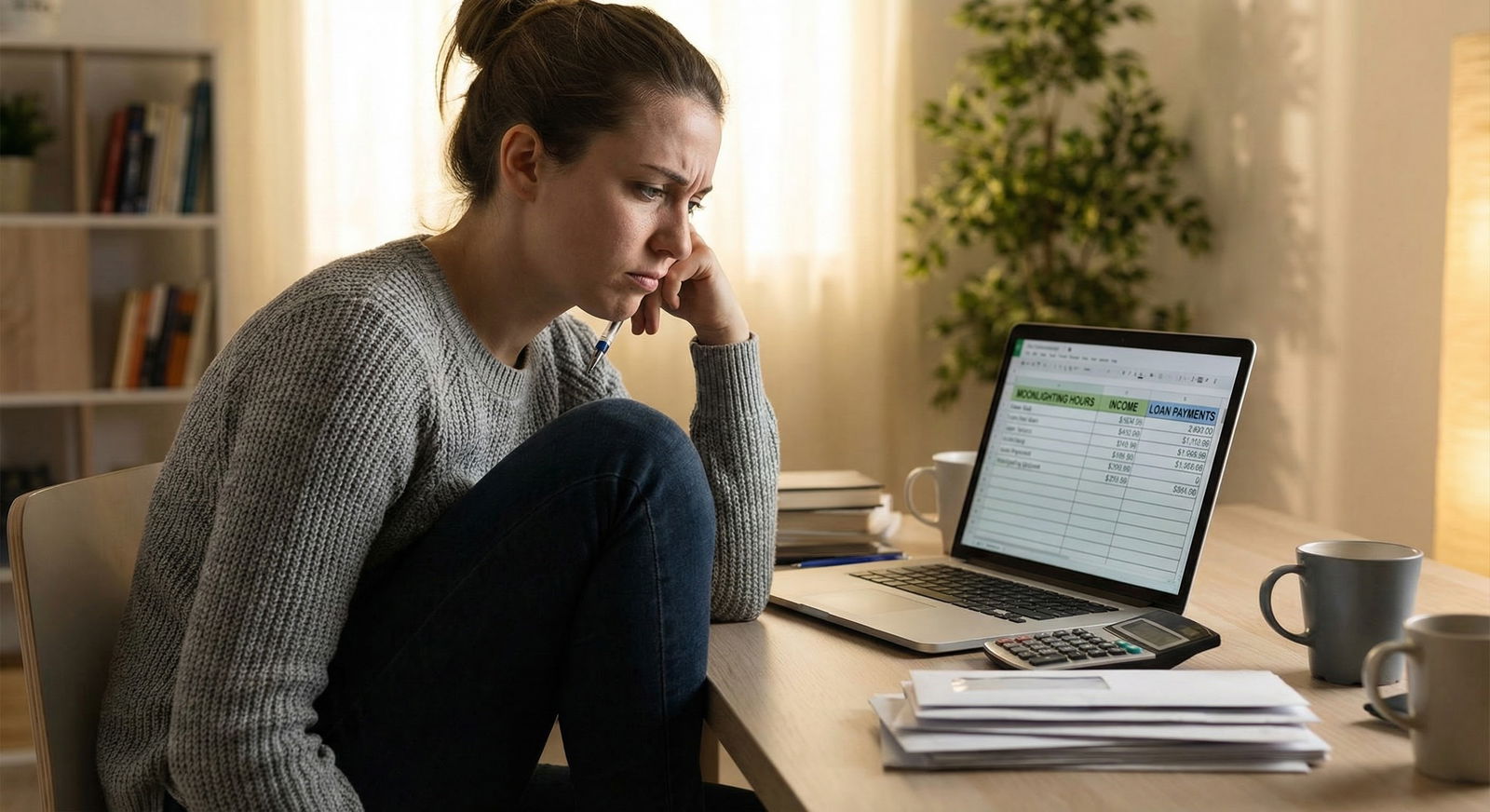
How to Reframe Moonlighting So It Doesn’t Eat You Alive with Guilt
Right now you probably feel like there are only two options:
- Don’t moonlight, stay “pure,” and feel resentful, broke, and trapped.
- Do moonlight, feel guilty and terrified you’re being judged all the time.
You need a third frame:
- Strategic, low-volume, transparent moonlighting that supports your development and financial sanity without touching your core responsibilities.
You’re allowed to want to pay rent without panic. You’re allowed to want a little control over your financial life instead of staring at interest on six-figure loans like it’s a horror movie.
If you:
- Protect your performance
- Follow the rules
- Ask for permission
- Monitor your own fatigue honestly
…then moonlighting doesn’t “prove” you’re uncommitted. It proves you’re navigating a broken system as safely as you can.
Will everyone see it that way? No.
Will enough people see your actual behavior and judge you on that instead of their own baggage? Yes.
You don’t need universal approval. You just need to not give anyone legitimate evidence that you care less about your residency than your side shifts.
| Aspect | Safer Pattern | Risky Pattern |
|---|---|---|
| Timing | Light rotations, off-call weekends | Pre-call nights, heavy ICU/wards |
| Volume | 1–3 shifts per month | Weekly or multiple per week |
| Transparency | PD approval, documented | Hidden, informal, no clear approval |
| Performance at Home | Stable or strong evaluations | Declining evals, complaints |
| Duty Hours | Logged accurately, within limits | Underreported, consistently >80 hrs |

| Step | Description |
|---|---|
| Step 1 | Interested in moonlighting |
| Step 2 | Do not moonlight |
| Step 3 | Review rules and get approval |
| Step 4 | Fix performance first |
| Step 5 | Choose low impact shifts |
| Step 6 | Monitor fatigue and evals |
| Step 7 | Cut back or stop |
| Step 8 | Continue cautiously |
| Step 9 | Program allows it |
| Step 10 | Performance solid? |
| Step 11 | Any concerns raised? |
FAQ (Exactly 6 Questions)
1. Will program directors automatically assume I’m less committed if I moonlight?
No, not automatically. They’ll assume you’re less committed if your moonlighting clearly affects your residency performance—missed conferences, chronic fatigue, delayed notes, complaints from attendings. If you stay ahead on all that and are transparent about your shifts, most PDs won’t turn moonlighting alone into a character judgment.
2. Should I tell my program about every moonlighting shift?
If your program requires approval or has policies about moonlighting (which most do), then yes, you should be upfront. Hiding shifts or being vague looks way worse than being transparent. Sneakiness is what gets labeled as “unprofessional” and “uncommitted” faster than the moonlighting itself.
3. How do I answer if someone bluntly asks, “Why are you moonlighting?”
Keep it calm and boring. Something like: “I’m doing a couple supervised shifts a month on lighter rotations to build more outpatient experience and help with my loans. I’m making sure it doesn’t interfere with my primary responsibilities here.” That frame is much harder to attack than “I need money” or “I’m trying to get ahead.”
4. What if my program technically allows moonlighting but my PD personally hates it?
That’s the worst gray zone. If the official policy says “allowed,” but your PD’s vibe is icy, you have to decide how much you’re willing to risk friction. If they openly tell you they’re concerned, I’d take that seriously. Burning your relationship with your PD over a few extra shifts isn’t worth it long-term, even if the policy’s technically on your side.
5. Can strong evaluations really “protect” me from the uncommitted label?
They don’t make you bulletproof, but yes, strong, consistent evaluations are your best shield. If faculty are writing, “Excellent work ethic, reliable, engaged in teaching,” it’s much harder for anyone to claim you seem detached just because you pick up occasional moonlighting shifts. Performance buys you credibility. Lack of performance makes moonlighting look like a smoking gun.
6. If I start moonlighting and feel my residency work slipping, is stopping going to look bad?
Stopping doesn’t make you look uncommitted; if anything, it makes you look self-aware. You can even say, “I tried a few shifts, but I noticed I was more tired than I liked, so I’ve decided to pause and refocus here.” That’s exactly the kind of judgment programs want to see. Pushing through obvious strain just to “prove” you can handle it—that’s what actually looks irresponsible.
Key takeaway #1: Moonlighting by itself doesn’t brand you as uncommitted; visible declines in performance and honesty do.
Key takeaway #2: If you’re transparent, follow the rules, keep your evaluations strong, and cut back the second your work slips, you’re already doing more than most to protect how you’re perceived.

















