
The number of “mysterious” night‑time ICU crashes is wildly overestimated. Most of them are pattern recognition plus disciplined structure.
Let me break this down specifically.
Night shift in the ICU is not about heroics. It is about having a repeatable, boringly systematic script that you run every single time a patient acutely decompensates. The people who crash and burn on nights are not the ones who “don’t know enough physiology.” They are the ones who lose structure, get tunnel vision, and forget basics under alarms and pressure.
You are in residency. You are tired. You are often alone or functionally alone. So you need a rigid mental framework that still works when your frontal lobe is half offline at 03:40.
This article is that framework.
The Non‑Negotiable First Moves: Before You Even Think
When the nurse calls “Hey, can you come see 12? He doesn’t look right,” you already lost if your first thought is “What could be causing this?” Wrong starting point.
Your first steps are procedural, not cognitive.
- Say: “I am coming. Put him on full monitor, get vitals now, page respiratory.”
- Walk, do not run, but do not dawdle.
- As you approach the room, your mind switches into ICU crash script mode.
Inside the room, this is your move set:
Announce and take control.
Say out loud, clearly: “Okay, I am here. I will run this. Please keep updating me on vitals.”
This does two things: calms the room and tells you that you are in charge.Look at the patient, not the monitor.
If the patient is grey and apneic but the monitor says “SpO2 100%,” the patient wins. The monitor is lying or lagging.Run an aggressive, no‑nonsense ABC check.
Do not overcomplicate this. You are looking for any immediately reversible disaster.Airway
- Is there an endotracheal tube? Is it in the mouth? Where is the lip marking compared to last note?
- Is the patient talking or making sounds? If not intubated, can they protect airway?
Breathing
- Is the chest moving symmetrically?
- Bag the patient for 5–10 seconds if needed: do you feel resistance (bronchospasm, obstruction, pneumothorax) or very easy bagging (disconnection, leakage)?
- Look for kinked tubing, disconnected ventilator, water in circuit, HME clogged.
Circulation
- Check femoral or carotid pulse yourself. Do not trust the pleth.
- Quickly look at the arterial line waveform if present: damped? lost?
- Bleeding? Obvious line disconnection? Surgical site oozing?
If there is no pulse: you are in ACLS, not “ICU nuance” mode. Call the code, start compressions, delegate.
If there is a pulse but the patient is hypotensive, hypoxic, altered, or all of the above: now you layer structure on top.
The Night‑Shift Crash Algorithm: A Structured Mental Model
You do not want ten unrelated mnemonics. You want one master framework that you can adapt to any crash.
The framework I teach residents is:
“Two loops: RESCUE loop, then DIAGNOSTIC loop.”
RESCUE loop = stabilize the dying physiology.
This is about buying 10–30 minutes of life.DIAGNOSTIC loop = figure out why and fix cause.
This is about preventing re‑crash.
The RESCUE Loop: What You Do in the First 5–10 Minutes
Think of this as “ICU ACLS + common sense.”
You cycle rapidly through:
- Airway
- Oxygenation / Ventilation
- Circulation / Perfusion
- Bedside data
- Call for help / parallel tasks
1. Airway and Immediate Oxygenation
Examples:
Intubated patient suddenly desats to 70s:
- Check ETT depth at teeth. Compare to documented depth.
- Listen quickly over epigastrium and both axillae. Unilateral breath sounds? Suspect mainstem vs pneumo.
- Suction aggressively. Plugged tube is common at 3 AM.
- If ventilator looks suspect, disconnect from vent, bag with 100% FiO2, feel compliance.
- If bagging improves sats, the problem is either the ventilator or a partial obstruction.
Non‑intubated patient obtunded and hypoxic:
- Jaw thrust. Oral or nasal airway if needed.
- 15 L non‑rebreather immediately while you think.
- Position: sit them up, not flat, unless hypotensive to shock levels.
- Decide fast: do they need to be intubated in the next 5–10 minutes? You can call anesthesia/airway team early and cancel later.
2. Ventilation and CO₂
You can crash from CO₂ problems alone: severe metabolic acidosis, over‑sedation, COPD retention.
- Look at respiratory rate and tidal volumes (on vent).
- Check last blood gas. If the patient was running a PaCO₂ of 25 for metabolic acidosis and someone “normalized” it, you have trouble.
- If apneic or severely hypoventilating, bag and prepare for intubation.
- Turn off any newly started sedatives or opioids. Yes, actually order them off.
3. Circulation and Perfusion: Structured Response to Hypotension
Now the real ICU work.
You want to rapidly categorize shock. You will never finish a textbook workup during the first crash minutes, but you can reasonably ask:
- Is this tank problem (hypovolemia/vasodilation)?
- Is this pump problem (cardiogenic/obstructive)?
- Is this pipe problem (massive sepsis, anaphylaxis, neurogenic)?
The fastest way to cut through is bedside ultrasound, but you still need basic steps.
Here is your move sequence:
Confirm the BP:
- Check NIBP manually if reading is bizarre.
- Check arterial line:
- Zero it.
- Flush it and see the waveform.
- If damped and low in radial, quickly check cuff on upper arm or femoral pulse to see if this is real.
Simple interventions you do while assembling the bigger picture:
- 500 mL crystalloid bolus for most undifferentiated hypotension, unless obvious cardiogenic overload (flash pulmonary edema, known severe HFrEF with JVD, wet lungs).
- If they are already on pressors, consider bumping by 0.02–0.05 (norepi) temporarily while you figure out etiology. Do not be shy about this.
- Check all lines: is the pressor actually going central? Did someone accidentally connect norepi to a peripheral lock that got stopped?
Quick shock type triage with ultrasound (if you can):
- IVC small and collapsing, RV normal, LV hyperdynamic → underfilled → more volume.
- RV huge, LV tiny, septum bowing → RV failure / PE / high PEEP / tension pneumo.
- LV poor squeeze, big, global hypokinesis → cardiogenic.
- Normal-ish but distributive picture, warm, high output → septic / vasodilatory.
If you do not have ultrasound skills yet, you use cruder markers, but the basic principle stands: do not treat all hypotension as “one more liter.”
The DIAGNOSTIC Loop: H’s, T’s, and ICU Reality
After the first 5–10 minutes, you must stop mindlessly pushing fluids and pressors. You pivot to a focused differential, still under the same structural lens.
I prefer to translate ACLS H’s and T’s into ICU‑specific buckets:
- Device / line / ventilator problems
- Iatrogenic screwups
- Sudden primary pathology events
- Slow‑burn issues that become visible at night

| Step | Description |
|---|---|
| Step 1 | Patient looks bad |
| Step 2 | Run ABC check |
| Step 3 | Call code and start ACLS |
| Step 4 | RESCUE loop |
| Step 5 | Airway and oxygen |
| Step 6 | Ventilation and CO2 |
| Step 7 | Circulation and perfusion |
| Step 8 | Bedside ultrasound and labs |
| Step 9 | DIAGNOSTIC loop |
| Step 10 | Device or line issue |
| Step 11 | Iatrogenic cause |
| Step 12 | Primary new event |
| Step 13 | Slow chronic issue decomp |
| Step 14 | Targeted fix and re-eval |
| Step 15 | Pulse present |
1. Device / Line / Ventilator Problems
These are embarrassingly common. That is why good night residents always run a device checklist before they order exotic tests.
Endotracheal tube:
- Too deep (mainstem intubation) after repositioning or sedation.
- Too shallow / self‑extubation.
- Cuff leak: sudden loss of tidal volume and low airway pressures.
Ventilator:
- Disconnection from patient side or machine side.
- Incorrect mode or settings changed accidentally.
- Auto‑PEEP in severe obstructive patients: sudden hypotension and tachycardia.
Lines:
- Pressor on peripheral line infiltrated: patient now effectively off pressor.
- Arterial line transducer slipped below level of heart → false high reading; above heart → false low.
- Bleeding from central line removal or dislodgement under the gown.
Drains and tubes:
- Chest tube kinked or disconnected → tension physiology if pneumo or hemothorax.
- NG/OG in wrong place (rare but deadly).
If the crash followed any manipulation (turning patient, imaging trip, line placement, procedure), the default assumption should be “we did this” until proven otherwise.
2. Iatrogenic Screwups
These are the things no one likes to say out loud on rounds but every ICU sees:
- Wrong‑rate insulin or heparin infusion.
- Two pressors running in one lumen, third hanging but not actually connected.
- New medication:
- Propofol bolus → hypotension.
- Beta‑blocker in someone already tenuous.
- Opioid or benzo given twice because of communication failure.
- Dialysis:
- Aggressive ultrafiltration → hypotension and arrhythmia.
- Electrolyte shifts causing arrhythmia.
So during your diagnostic loop, you literally say to the bedside nurse:
“Walk me through every drip change, new med, and procedure in the last 60–90 minutes.”
You will catch a lot that way.
3. Sudden Primary Events: The “Big Killers” You Cannot Miss
These are the ones that will haunt you if you do not explicitly consider them for every crash:
- Massive PE
- MI / arrhythmia
- Tension pneumothorax
- Tamponade
- Massive hemorrhage
- Sepsis explosion / abdominal catastrophe
- Acute neurologic event (massive stroke, herniation, seizure)
Your thought process should be structured, not random guessing.
Example 1: Intubated patient, septic, suddenly hypotensive and hypoxic after turning.
- First suspicion: pneumothorax or auto‑PEEP.
- Clues:
- Peak pressures increased?
- New unilateral absence of breath sounds?
- Neck veins distended?
- POCUS: lung sliding on both sides? RV huge?
- Action:
- Drop PEEP temporarily, bag and feel resistance.
- If high suspicion for tension, needle decompression before waiting on CXR.
Example 2: Post‑operative patient, day 2 after major abdominal surgery, tachycardic, hypotensive, rising pressor needs.
- Consider:
- Intraabdominal catastrophe: leak, bleeding.
- PE.
- Sepsis from anastomotic leak.
- You:
- Check lactate, Hgb, bedside ultrasound for free fluid.
- Discuss with surgeon early about CT vs straight back to OR if peritonitic.
Example 3: Long‑term ventilated ARDS patient, suddenly bradycardic, hypertensive, blown pupils.
- Think:
- Herniation from uncontrolled ICP (esp. neuro ICU).
- Severe hypercarbia?
- You:
- Call neurostat.
- Elevate head of bed.
- Ensure adequate ventilation, consider hyperventilating temporarily if known ICP issue.
- Get emergent CT head if not obviously non‑survivable.
4. Slow‑Burn Issues That Decompensate at Night
These are the quiet killers that show up as “soft signs” on days, then blow up at 03:00.
- Progressive delirium → self‑extubation, pulling lines.
- Rising creatinine and fluid overload → flash pulmonary edema.
- Slow GI bleed not taken seriously on day team → now hypotensive, melena, dropping Hgb.
- Poor nutrition, frailty, and under‑recognized sepsis → vasoplegia.
This is where good sign‑out matters. If you know at 19:00 that “bed 8 has borderline belly pain but CT was ‘ok’,” and at 01:00 they are more tachycardic and hypotensive, you do not casually add 500 cc and walk away. You re‑interrogate the original concern.
Using Bedside Data: Labs, Ultrasound, and Monitoring With Intention
The worst thing you can do at night is order a broad panel (CBC, CMP, coags, lactate, troponin, BNP, procalcitonin, VBG, ABG, 5 cultures) on every crash without a question in mind. You drown in noise.
You want targeted, high‑yield data that feeds back into decisions.
| Situation | Highest-Yield Tests / Tools |
|---|---|
| Undifferentiated shock | Bedside echo, lactate, ABG/VBG |
| Suspected PE | Echo RV strain, DVT ultrasound |
| Vent desat in ARDS | ABG, vent graphics, lung ultrasound |
| Possible hemorrhage | Hgb, rapid TEG/ROTEM, type & screen |
| Arrhythmia / MI concern | EKG, troponin, electrolytes |
Bedside Ultrasound Priorities
If you have basic POCUS skills, your crash exam at night is not a full fellowship‑level exam. It is a triage scan:
Cardiac:
- Is there gross pericardial effusion with tamponade physiology?
- LV squeeze: decent / poor / hyperdynamic?
- RV huge or not?
IVC:
- Flat and collapsing → more volume likely safe.
- Full, non‑collapsing → volume less likely to help; consider pressors/inotrope.
Lungs:
- Lung sliding or not?
- Bilateral B‑lines (pulmonary edema)?
- Large effusion?
You do not need measurements. You need direction.
Labs and Blood Gases
ABG/VBG is your friend on night crashes. You are looking for:
- pH trend: is this a mounting metabolic acidosis?
- PaCO₂: are you under‑ventilating a severe acidosis?
- Lactate: is this distributive or cardiogenic shock intensifying?
If lactate is 7 and rising with pressors climbing, you push for deeper interventions: source control, echo, maybe mechanical circulatory support in some centers.
Communication and Leadership During a Crash
The most underrated skill for night ICU survival: controlling the room with your voice.
You do not need to sound like an attending, but you must sound like somebody in charge.
Use closed‑loop communication. Use names. And narrate your thought process enough that others can help you catch errors.
A Practical Script
Here is what I actually say in these moments:
- “Okay team, this is hypotension and desaturation in bed 10. I will run this. Sarah, please keep me updated on vitals every minute.”
- “Airway is secure, tube at 22, bilat breath sounds. We are on 100% FiO2, bagging now.”
- “We have a pulse. This is not a code yet. I want a 500 mL bolus wide open now, and norepi up from 0.08 to 0.12. Please repeat BP every 2 min.”
- “I am looking at the heart on ultrasound now. LV is hyperdynamic, IVC is small. This looks underfilled or septic, not cardiogenic.”
- “Next steps: check lactate, ABG, blood cultures, and broad‑spectrum antibiotics. Let us call the attending while we do this.”
It sounds almost theatrical when you read it, but this sort of running commentary:
- Focuses your own thinking.
- Reassures the nurses that you are not flailing.
- Gives junior staff and RT clear roles.

| Category | Value |
|---|---|
| Sepsis worsening | 30 |
| Arrhythmia/MI | 20 |
| Device/line issue | 25 |
| Pulmonary event | 15 |
| Hemorrhage | 10 |
Escalation: When and How to Call for Backup
If you are a resident, here is the truth: you should call for help earlier than you think. Attendings are not impressed by “I waited until they arrested.”
Clear rules of thumb that usually work:
- Any patient needing a second pressor at night → attending aware.
- Any new need for intubation in a previously non‑intubated patient → attending aware.
- Any suspicion of:
- Massive PE
- Tamponade
- Abdominal catastrophe
- Uncontrollable bleeding
- Herniation event
→ attending and relevant consultants aware immediately.
When you call, do not say “The patient is crashing.” Say:
“Hi Dr. X, this is Y in the ICU. Bed 12, 65‑year‑old male with septic shock, was stable on norepi 0.08, now acutely hypotensive to 70 systolic and more hypoxic. I have confirmed tube placement, bagged with 100% O2, increased norepi to 0.16, given 500 mL bolus, and I am seeing a hyperdynamic LV and small IVC on ultrasound. Lactate pending. I think this is worsening distributive shock and may need escalation of pressors and source control. Can you come in or guide next steps?”
That call gets a very different response than “He doesn’t look good.”
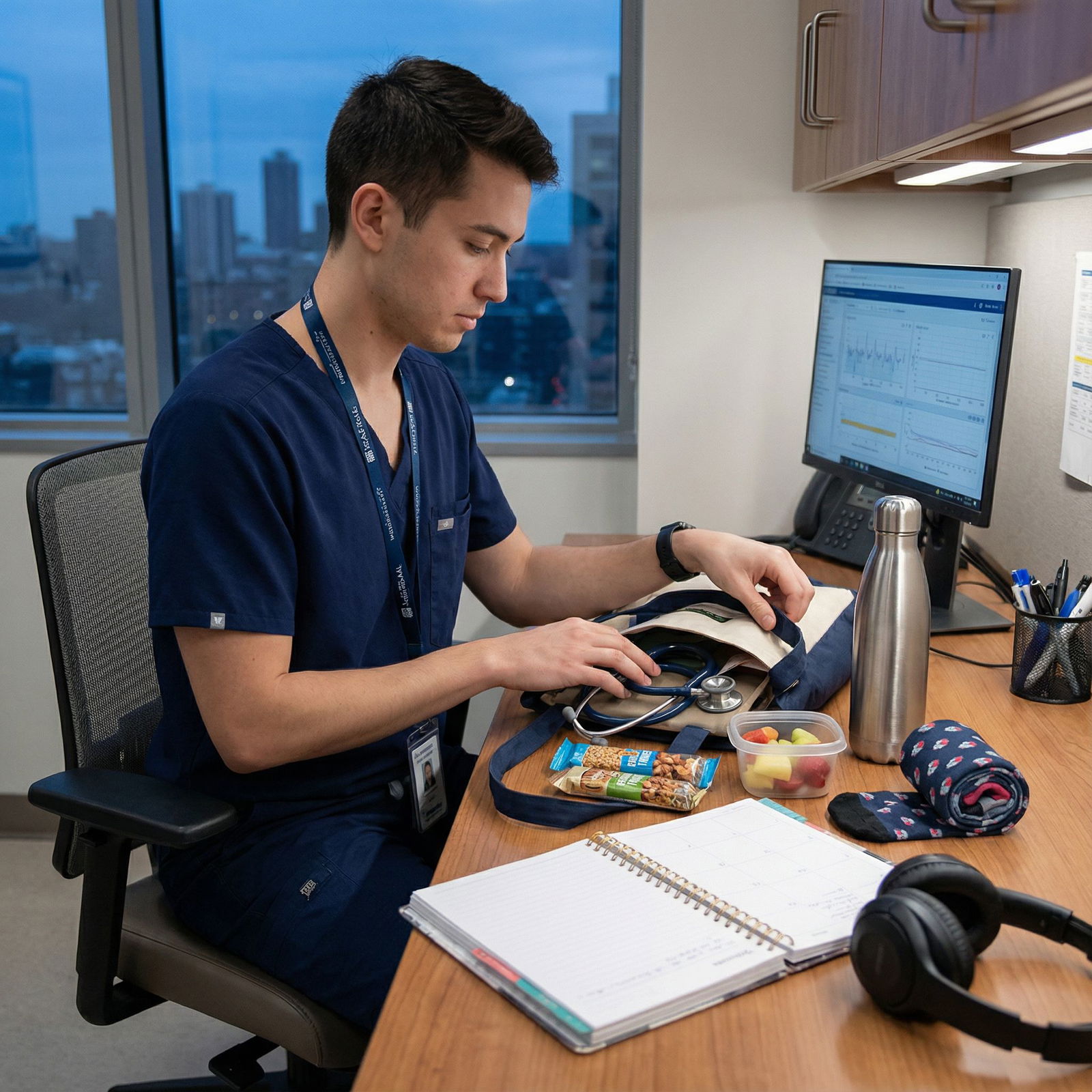
Pre‑Emptive Work: How to Reduce Night Crashes Before They Start
This part is boring. Which is exactly why it prevents disasters.
There are four habits that separate safe night residents from the ones always in firefights.
Aggressive, honest sign‑out.
- Identify “watch” patients explicitly:
- “If anyone is going to crash, it is bed 3 and bed 7. Here is why…”
- Know the plan if they deteriorate: when to intubate, when to add second pressor, where not to give fluid.
- Identify “watch” patients explicitly:
Early night rounding with intent.
- Do not just “eyeball” them. For each high‑risk patient, ask:
- “What will kill this person in the next 8 hours?”
- “If they became hypotensive right now, what would I do first?”
- Adjust orders proactively: PRN bolus ranges, pressor targets, sedation, respiratory weaning.
- Do not just “eyeball” them. For each high‑risk patient, ask:
Hard lines about dangerous orders.
- Do not start new beta‑blockers or high‑dose sedative regimens at 23:45 on tenuous patients unless you have a compelling reason.
- Clean up medication lists: stop duplicate antihypertensives; clarify hold parameters.
MENTAL rehearsal.
- I am absolutely serious about this. On a quiet night, mentally run:
- “Tube dislodgement scenario.”
- “Sudden PEA in a septic patient.”
- “Dialysis hypotension with arrhythmia.”
- That way, at 02:00, your brain is not doing it for the first time.
- I am absolutely serious about this. On a quiet night, mentally run:
A Final Note on Emotional Fallout
Night crashes feel personal. Especially the ones that end badly. I have seen good residents spiral after a rough code.
You need two things:
A post‑event structure
- Brief hot debrief at bedside: what worked, what did not, anything we should have done differently in the moment.
- A short review next day with attending: walk through timeline, decisions, and physiology in a calm setting.
A psychological rule
- You are responsible for process and structure.
- You are not omnipotent, and not every crash is survivable, especially in an ICU population.
The goal is not to prevent every death. The goal is to make sure that when a patient crashes at night on your watch, the response is swift, structured, and rational, not chaotic.
FAQs
1. What is the single most important thing to do first in a night‑time ICU crash?
Look at the patient and run a hard ABC check before you touch the computer or order anything. Confirm airway, breathing, and circulation with your own eyes and hands. Many “mysterious” crashes are actually tube issues, ventilator disconnections, or loss of pulse that monitors have not caught yet.
2. How much fluid should I give in undifferentiated hypotension at night?
A reasonable starting move is a single 500 mL crystalloid bolus while you evaluate, unless there is obvious cardiogenic shock or gross volume overload. Beyond that, you should be using bedside ultrasound, physical exam, and labs to guide further fluid. Blind 2–3 L boluses in the ICU at 02:00 cause as many problems as they solve.
3. When should I intubate a crashing patient rather than “wait and see”?
If you are bagging to maintain oxygenation, if mental status is not compatible with airway protection, or if the work of breathing is clearly unsustainable, you should move toward intubation. Err on the side of controlled intubation with preparation rather than emergent crash intubation after arrest. Call your attending or airway team early; it is easy to cancel if the patient improves.
4. How do I quickly distinguish septic from cardiogenic shock at the bedside?
Use a combination of clinical picture and basic ultrasound. Warm extremities, wide pulse pressure, hyperdynamic small LV, and collapsible IVC suggest distributive/septic shock. Cool clammy extremities, JVD, poor LV squeeze, B‑lines in lungs, and full IVC point toward cardiogenic. These are not perfect, but they are far better than guessing.
5. What should I absolutely communicate to the attending when a patient crashes at night?
Give a tight, structured report: who the patient is, baseline status, what changed (vitals and timing), what immediate actions you took (fluids, pressors, airway moves), what you are seeing on exam/POCUS, and your leading hypothesis. Then explicitly ask for what you need: bedside evaluation, order guidance, or approval for escalation like second pressor or OR/CT transfer.
6. How do I get better at running these events without constant panic?
Deliberate practice. Review each crash with an attending, walk through what happened minute by minute, and build a personal script. Practice mental rehearsals. Get comfortable with basic POCUS views. And standardize your first 5–10 minutes (RESCUE loop) so you are never improvising the basics at 03:00. Pattern plus structure is what turns panic into controlled urgency.
Key points:
Use a rigid, rehearsed structure (RESCUE loop then DIAGNOSTIC loop) for every night‑time ICU crash.
Assume devices and iatrogenesis first, then hunt for the big killers with targeted data and bedside ultrasound.
Lead the room with clear, concise communication and call for help early, not after the patient is unsalvageable.



















