The idea that “night float is always worse for burnout” is lazy, wrong, and not what the data shows.
Night float can wreck you. It can also quietly save your sanity compared to brutal 28‑hour call. Whether it burns you out depends less on “night = bad” and a lot more on how your program structures it, how often you flip schedules, and whether you ever get real recovery.
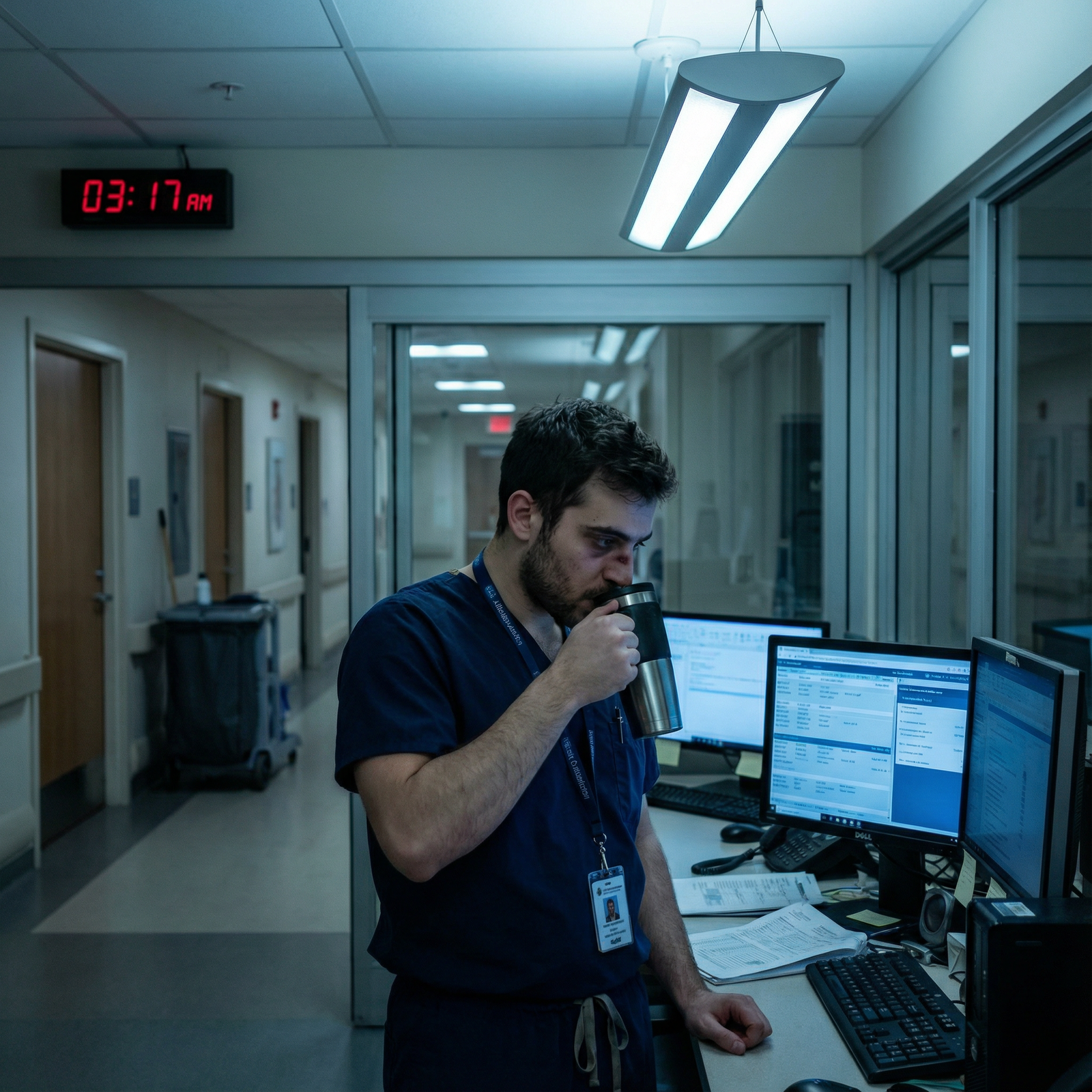
Let me walk through what the actual duty‑hours research says, not what people yell in workrooms at 2 a.m.
What We Think Is True About Night Float
You have heard all of this:
- “Night float residents are always more burned out.”
- “Humans aren’t nocturnal, so night float is inherently terrible.”
- “Day‑night switching is better because at least you do not live in vampire mode.”
- “Duty‑hour limits and night float just made everything worse.”
These are half‑truths, repeated so often they’ve become gospel. The problem is, when you actually look at the big duty‑hours trials and sleep studies, the picture is more complicated. Sometimes the exact opposite is true.
Let’s get specific.
What Major Duty‑Hour Studies Actually Show
Everyone loves to wave around “the duty‑hour literature” as if it clearly says one thing. It doesn’t. But there are patterns—especially when you compare traditional 24–30‑hour call to night float and other “shift‑based” systems.
The big picture: call vs shift, not day vs night
Most large studies compare:
- Traditional extended call (e.g., q4 28‑hour in‑house) vs.
- Shift‑based or night‑float heavy schedules (capped shifts, more handoffs)
When you zoom out, three repeated findings show up:
- Extended-duration shifts (24+ hours) blow up sleep, performance, and safety.
- Removing those marathon shifts reduces errors and serious fatigue, but…
- There’s often no massive, consistent improvement in “burnout” scores across the board.
So you get residents who are less dangerously exhausted but not magically “unburned out.” Why? Because burnout isn’t just hours; it’s workload density, culture, support, and feeling disposable.
But here’s the key myth bust: night float itself is not consistently the villain. In many of these systems, night float is the instrument used to kill 28‑hour call.
A quick reality check in numbers
Here’s the kind of pattern you see across multiple studies (Ball et al., Landrigan’s groups, the FIRST and iCOMPARE ecosystems, etc.):

| Category | Value |
|---|---|
| 24+ hr Call | 4.5 |
| Night Float / Shifts | 6.5 |
On average, residents on shift‑based or night‑float systems:
- Sleep more per 24 hours (often 1.5–2 hours more)
- Report fewer attention lapses
- Have fewer catastrophic errors tied to fatigue
But “burnout score”? Often flat. Nights aren’t a magic cure, but they’re also not automatically worse.
Night Float vs 24‑Hour Call: Who Actually Has It Worse?
If you make me choose between a well‑built night‑float system and true q4 28‑hour call for months? I’ll take night float and not blink.
And the data largely backs that up.
Sleep and cognitive performance
Extended shifts (24+ hours) are a disaster from a sleep science perspective. Controlled studies on interns show:
- Staying awake >24 hours produces cognitive impairment equivalent to being legally drunk.
- Each 24‑hour in‑house call can cut total sleep time to 2–4 hours, often fragmented and low‑quality.
- Residents on extended call systems have higher rates of serious medical errors and near‑misses.
Night float, even when tiring, usually means:
- Shorter maximum continuous work time (9–14 hours vs 28+)
- More predictable sleep windows off‑shift
- Potential to anchor your circadian rhythm (if rotations aren’t constantly flipping you back to days)
Is being awake all night ever “healthy”? No. But compared to the biochemical train wreck of 30 hours straight? It’s the lesser evil.
Burnout outcomes: not what the myths say
When burnout has been measured (Maslach Burnout Inventory and similar), a few patterns pop up:
- Replacing 24‑hour call with night‑float blocks sometimes lowers emotional exhaustion.
- More often, emotional exhaustion stays similar, but residents feel less acutely destroyed and safer.
- Depersonalization and sense of accomplishment barely budge just from swapping call for nights.
Translation: night float usually doesn’t worsen burnout compared with old-school call. It just doesn’t fix the rest of residency being overloaded, under‑resourced, and bureaucratically absurd.
When Night Float Turns Toxic
Now let’s be honest: some night‑float systems are absolutely burnout accelerators. But not because nights are cursed. Because the design is bad.
Common self‑inflicted disasters:
Rapid day–night flipping.
Example: 3 nights on, 2 days off, back to days, then nights again the following week. This crushes your circadian system. Sleep becomes short, fragmented, and misaligned. That’s when depression scores and burnout spike.No protected recovery.
Programs love to sneak in “mandatory” didactics or meetings right after a run of nights. Or they flip you to a 7 a.m. day after your last night without 24 hours off. That is how you turn “tough but survivable” into “I hate medicine.”Night = dumping ground.
Some services intentionally load census and tasks onto the night team:- All the cross‑cover for half the hospital
- Zero ancillary support after 6 p.m.
- “Just put orders in, the day team will fix it” culture
You end up with high volume, low control, and zero recognition. That is textbook burnout fuel.
No team identity, no feedback.
Nights can feel invisible. You rarely see attendings. You never get real teaching or feedback. You never see your patients improve, only catch them crashing. That chronic “nothing I do matters” sentiment is much more corrosive than the hour you woke up.
It’s not “night float = bad.” It’s “garbage schedule design + poor support = bad.”
Comparing Common Schedules: Which Is Actually Worse?
Let’s compare a few realistic patterns you’ll see in residency.
| Schedule Type | Relative Burnout Risk | Main Problem Driver |
|---|---|---|
| Q4 28-hr Traditional Call | Very High | Sleep deprivation, errors |
| 6+ Consecutive Night Float | Moderate | Social isolation |
| Flipping Day–Night Every Few Days | Very High | Circadian chaos |
| 2-Week Stable Night Block + Recovery Day | Lower | Still tough, but predictable |
The one that reliably comes out worst in both data and lived experience? Constant flipping and old‑school 24–30‑hour call.
A two‑week straight night block with:
- A protected post‑nights recovery day
- Stable timing (same start/end each shift)
- Reasonable census and some support
…is hard, yes. But not automatically worse for burnout than a “normal” ward month with 70–80 daytime hours, administrative bloat, and your phone never stopping.
What the Circadian Science Actually Says
Let’s bring sleep biology into the room instead of pretending “nights vs days” is just vibes.
Humans aren’t nocturnal—but we can adapt
Baseline, yes, we’re diurnal. But:
- The circadian system can partially adapt to night schedules in ~3–7 days.
- The main killers of adaptation are:
- Rotating shifts too frequently
- Bright light at the wrong times
- Totally inconsistent sleep windows
A stable night‑float block where you:
- Keep sleep timing roughly the same every day
- Use blackout curtains and light discipline
- Avoid flipping back and forth on your days off
…will usually leave you less destroyed than:
- Constantly alternating between early pre‑round days, 28‑hour calls, and random late stays.
It’s the whiplash, not the darkness, that does a lot of the damage.
Social jet lag is real—and fixable
Social isolation on nights is a problem, but it’s not pure biology, it’s design:
- Programs that schedule all conferences at 7 a.m. obviously exclude night residents.
- Services that never loop the night team into patient follow‑up create that “I don’t matter” feeling.
- Chiefs who pretend nights don’t exist unless a code blue happens are telegraphing: you’re expendable.
Those are fixable culture problems. Not some immutable law of the circadian universe.
What Residents Actually Report on Night Float
Let me translate the pattern I’ve heard (and seen) over and over, in med‑peds, IM, surgery, OB:
On a well‑run night float:
- “I’m tired, but in a predictable way.”
- “I actually sleep during the day most days.”
- “I see interesting acute pathology and feel useful.”
- “I’m less anxious than on long call because the time horizon is clear.”
On a disaster night system:
- “I never fully switch to nights before they flip me back.”
- “I’m either exhausted or wired all the time.”
- “Everything gets dumped on us and no one in the day really knows what we do.”
- “I feel like an invisible code monkey, not a doctor.”
Same clock hours. Totally different burnout trajectories.
Design Features That Make Night Float Less Burnout‑Inducing
You want evidence‑aligned night float that doesn’t torch your psyche? Focus on structure, not just total hours.
Features that actually help:
Stable, contiguous blocks.
Two weeks of nights in a row beats “3 nights here, 2 there, then back to days” every time for circadian and mood.True protected recovery after the block.
One full calendar day with no clinical work at the end of nights. Not post‑call clinic. Not “come to noon conference, it’ll be quick.”Cap on cross‑cover insanity.
Reasonable cross‑cover ratios. Clear triage rules. No “you cover every medicine and neuro patient in the hospital, good luck.”Built‑in connection to days.
- Short overlap with day team for teaching and feedback
- Clear sign‑out structure where your decisions are seen and not erased
- Some chance to follow a subset of patients over your block
Respect for sleep on off days.
Chiefs and PDs not scheduling 7 a.m. mandatory sessions on your “day off” mid‑nights. This shouldn’t be controversial, yet here we are.
Programs that implement these see fewer complaints, more stable sleep reports, and no worse burnout than their day‑only blocks.
So, Is Night Float Always Worse for Burnout?
No. That statement is just wrong.
Here’s what the data and real‑world experience actually support:
- Extended 24–30‑hour call is almost always worse for fatigue, safety, and often for burnout, than a sane night‑float system.
- Night float does not automatically increase burnout—and can be equal or sometimes better if it is stable, predictable, and backed by real recovery time.
- The biggest burnout drivers are:
- Circadian chaos from rapid flipping
- Unreasonable workload and cross‑cover
- Being treated as invisible and disposable at night
If you want less burnout, you do not start by banning night float. You start by banning stupidity: constant flipping, fake “days off,” and using nights as the universal dumping ground.
How to Think About Your Own Night Float Experience
If you’re in residency now, ask yourself:
- Am I consistently sleeping at least 5–6 hours in a consolidated block most days on nights?
- Is my night block stable, or do I keep flipping between days and nights?
- Do I feel like my work at night is seen, valued, and connected to patient care, or does it vanish at 7 a.m.?
If the answers are:
- “No sleep, constant flipping, invisible work” → that’s a design problem, not an inevitable feature of nights.
- “Sleep is decent, block is stable, work is heavy but meaningful” → you’re tired, but not necessarily more burned out than your miserable friends on q4 call.
The Short Version
Night float is not inherently worse for burnout. It can be better than the old marathon‑call model, or it can be a dumpster fire, depending on how it’s built.
Key truths to keep in mind:
- The real enemies are 24–30‑hour shifts and chaotic day–night flipping, not night float itself.
- Stable, well‑designed night blocks with real recovery time often produce less dangerous fatigue and no worse burnout than heavy day services.
- If your night float is destroying you, blame schedule architecture and culture—not the clock striking midnight.



















