The harsh truth: most people asking “am I too old for medical school?” are asking the wrong question.
You’re not too old. You might, however, be too unprepared, too unrealistic, or too unwilling to change your life in the ways medicine actually demands.
This guide isn’t here to pat you on the head. It’s a structured self‑assessment so you can answer one question honestly: Should I do this — and if yes, how?
1. Age Reality Check: What “Too Old” Actually Looks Like
Let’s get the age piece out of the way first, because that’s what’s screaming in your head.
You are not “too old” for medical school simply because of your age if you’re:
- In your 20s or 30s: You are firmly in the normal-to-common range, even if you feel behind.
- In your 40s: You’re nontraditional, but it’s done every single year.
- In your 50s: It’s rare, but not impossible. You just need a brutally honest plan and clear reasons.
The real question isn’t “Am I too old?”
It’s: What does my timeline look like and do I actually accept it?
Here’s a rough, typical timeline if you’re starting now:
| Age You Start Prereqs | Start Med School | [Finish Med School (MD/DO)](https://residencyadvisor.com/resources/nontraditional-path-medicine/how-many-years-will-it-really-take-me-to-become-an-attending-now) | Finish Residency (Shorter Specialty) |
|---|---|---|---|
| 24 | 26–27 | 30–31 | 33–35 |
| 30 | 32–33 | 36–37 | 39–41 |
| 35 | 37–38 | 41–42 | 44–46 |
| 40 | 42–43 | 46–47 | 49–51 |
| 45 | 47–48 | 51–52 | 54–56 |
So if you’re 34 thinking “I’ll be 42 when I’m done”… yes. That’s roughly right.
The only honest follow‑up:
Do you want to be 42 and a practicing physician, or 42 still wondering if you should’ve tried?
If you’re older than 45, the bar moves:
- You need clearer financials.
- You need realistic expectations about specialty options.
- You need more tolerance for risk and uncertainty.
But you’re not automatically disqualified.
2. A Hard Look at Your Motivation (Not the Instagram Version)
“I want to help people” isn’t enough. Every nursing, PA, PT, and social work applicant says that.
You need to separate “I love science + long training + delayed gratification” from “I like health care and respect.”
Here’s a quick self‑interrogation. Answer these on paper, not in your head:
- What specific physician roles attracted you? (Not “doctor.” Example: outpatient psychiatry, hospitalist in a community hospital, outpatient primary care in underserved areas.)
- What non‑physician roles did you seriously consider? (NP, PA, RN, psychologist, clinical social worker, etc.)
- Why did you reject those paths? Be concrete. “Less autonomy,” “shorter training,” “lower pay,” “not enough physiology,” whatever it is — write it down.
- Can you name three downsides of being a physician that you still accept?
Things like:- Malpractice risk
- 24/7 responsibility for results of your decisions
- Administrative burden and decreasing autonomy
If all your answers are vague and emotional (“I’ve just always wanted to be a doctor” with nothing deeper), you’re not ready. You’re in career‑fantasy mode, not career‑decision mode.
If you’re older, you especially can’t afford fantasy. Your margin for error is smaller.
3. Academic Readiness: Are Your Numbers and Skills Actually Competitive?
This is where a lot of older applicants quietly fall apart: they want it, but they can’t show schools they can survive the firehose.
You need to assess three things:
- Your past academic record
- Your current academic ability
- Your MCAT trajectory
Step 1: Your Existing GPA
Pull every transcript. Calculate:
- Cumulative GPA
- Science GPA (BCPM: Biology, Chemistry, Physics, Math)
If you don’t want to calculate manually, you can use online AMCAS GPA calculators.
Here’s the blunt range:
| GPA Range | How It’s Viewed for Nontrads |
|---|---|
| 3.7+ | Strong, if recent science is also solid |
| 3.4–3.69 | Competitive with strong upward trend |
| 3.1–3.39 | Possible if there’s a clear, recent academic comeback |
| 2.8–3.09 | Needs significant repair and strong narrative |
| < 2.8 | Extreme uphill battle; SMP/post‑bacc almost mandatory |
If your GPA is old but you’ve recently done 20–30 credits of hard sciences (orgo, biochem, upper‑level bio, etc.) with A/A‑, that “recent work” can weigh heavily for you as a nontraditional.
If your last serious science course was 12+ years ago and you squeaked through with Bs and Cs, you cannot skip straight to MCAT. You need fresh coursework.
Step 2: Can You Study at a High Level Again?
Ask yourself:
- When was the last time you learned something complex from a textbook — not YouTube — and had to be tested on it?
- Can you realistically study 15–25 hours/week for 12–24 months on top of your existing responsibilities?
- How do you perform under time pressure and high‑stakes testing?
If you haven’t tested yourself recently, do this within the next 2 weeks:
- Take a timed practice exam in anything standardized: GRE, a full‑length MCAT diagnostic, or a rigorous science midterm if you’re already in classes.
- Don’t prep. Just see where your stamina, focus, and test anxiety actually stand.
This isn’t about the score; it’s about whether your brain and schedule can still handle the grind.
Step 3: MCAT Reality
The MCAT is not “just another test.” It’s 7.5 hours of:
- Dense passages
- Multi‑step reasoning
- Fatigue management
You’re aiming for:
- 510+ to be broadly competitive
- 505–509 workable with strong GPA, strong story, and good school list
- Below 500: expect many doors to close unless compensated by something exceptional and a very strategic list
For older applicants, a strong MCAT is one of your best ways to scream, “Yes, I can still perform at a high academic level.” If you’re not willing to grind for this, medicine isn’t for you.
4. Life Logistics: Can Your Real Life Handle This?
This is where nontraditional applicants either get real or self‑sabotage.
You have to look at:
- Money
- Family and relationships
- Time and energy
- Geographic constraints
Financial Check: Not Vibes — Numbers
Sit down and build a 10–15 year rough financial picture, including:
- Current debt: credit cards, loans, mortgage
- Projected med school debt: $200k–$400k is common in the US
- Years of lost or reduced income during:
- Prereqs / post‑bacc
- Med school (basically zero income)
- Residency (low income relative to effort)
Now ask:
- If you start practicing at 45 or 50, how many earning years do you realistically have left?
- How does that compare to your anticipated debt and lifestyle expectations?
- If you have kids: college costs, health needs, childcare — who covers those?
You don’t need a perfect spreadsheet. But you do need a credible plan that your future self won’t curse you for.
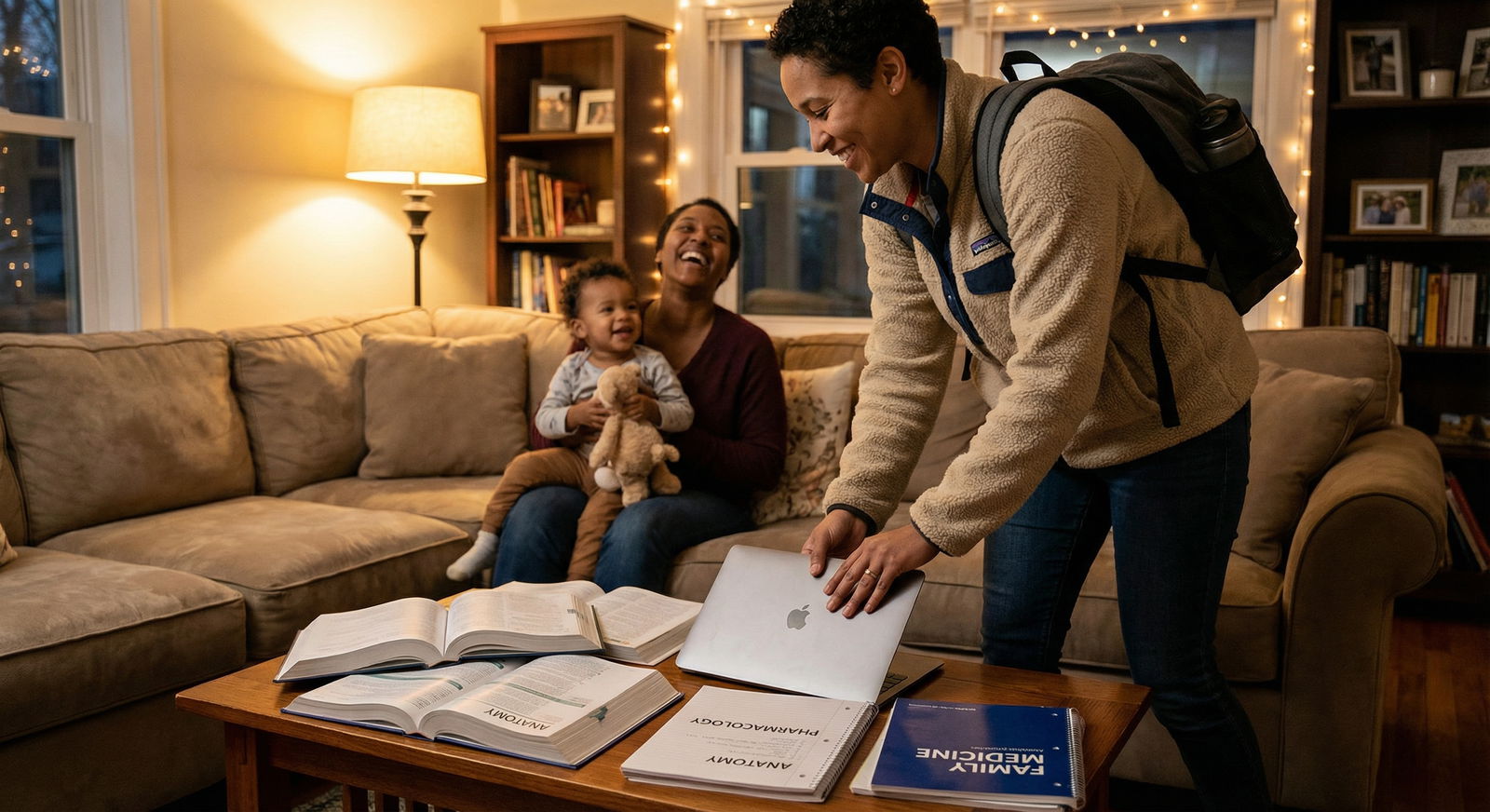
Relationships and Kids
A few ugly truths I’ve watched play out:
- Marriages crack when one partner suddenly disappears into 60–80 hour weeks plus constant stress.
- Kids don’t care that “Mom’s in residency” — they just know you’re gone a lot.
- Partners can say “I’ll support you” now and still resent you later when the reality hits.
So have the uncomfortable conversations now:
- With your partner: “What does a normal week look like for us in med school? In residency?”
- With yourself: “Am I okay missing games, recitals, dinners, and trips for several years?”
- With extended family: “Can I realistically count on childcare / backup help?”
If everyone hand‑waves these away, that’s a red flag. You’re building on fantasy, not structure.
5. Physical and Mental Stamina: Can Your Body Do the Work?
Age itself isn’t the problem. Declining resilience + no plan is.
Ask yourself, with zero sugar‑coating:
- Can I be on my feet for 8–12 hours on clinical days?
- How do I function with 5–6 hours of sleep for stretches of time (not forever, but during rotations)?
- Do I have chronic health issues that would make certain specialties brutal or unsafe?
- What’s my current mental health baseline? Anxiety, depression, ADHD — all manageable, but only if you’re actively managing them.
If you’re already burning out in a standard 9–5 with no kids and minimal stress, residency will eat you alive.
If you’re older but:
- You exercise regularly
- You’ve handled real stress in past roles
- You have strategies for sleep, boundaries, and recovery
…you may actually outperform younger classmates who’ve never been tested.
6. Professional Story: Does Your Background Help or Hurt?
Nontraditional isn’t a liability by default. Done right, it’s an asset.
Your previous career can be:
- Directly relevant (RN, PA, EMT, military medic, clinical research)
- Indirectly powerful (teacher, engineer, business owner, social worker, veteran)
- Or confusing (a string of unrelated jobs with no clear narrative)
Your job is to extract a coherent arc:
- What have you done?
- What did you learn about yourself?
- How did that push you toward physician specifically, not just “health care”?
- How will that experience make you a better doctor and a strong member of a med school class?
If your story is: “I hated my job, I’m burned out, and I’ve always wanted to be a doctor,” that’s not a narrative. That’s escapism in a white coat.
You want something closer to:
- “I worked in X role for 10 years, saw Y problems, tried Z solutions within my scope, and hit clear limits where physician training was necessary to fix the things I cared most about.”
7. Structured Self‑Assessment: A Simple Scoring Framework
Let’s simplify this into a quick, brutally honest self-check. Rate yourself 1–5 in each area:
1 = major problem, 5 = strong
- Academic foundation (GPA, recent coursework)
- Testing ability (MCAT readiness, stamina)
- Financial readiness
- Family/relationship support
- Physical and mental stamina
- Clarity of motivation/story
- Willingness to relocate and sacrifice lifestyle
- Time available for preparation (next 1–3 years)
Add your scores.
- 32–40: You’re in strong shape. Your job now is tactical — prereqs, MCAT, experiences, and applications.
- 24–31: Possible, but you’ve got serious gaps. You need a 1–2 year strengthening plan.
- <24: You’re in “major risk” territory. You either need to delay and rebuild key parts of your life, or seriously consider alternative careers in health.
This isn’t official. But it forces you to stop hiding weak spots under “I’ll figure it out.”
8. If the Answer Is “Yes, I Still Want This” — What Next?
If you’ve gone through all that and medicine still makes sense, here’s the basic sequence.

| Step | Description |
|---|---|
| Step 1 | Decide to Explore Medicine |
| Step 2 | Academic Audit |
| Step 3 | Complete/Repeat Prereqs |
| Step 4 | Clinical & Shadowing Experience |
| Step 5 | MCAT Preparation |
| Step 6 | Apply to Schools |
| Step 7 | Interviews |
| Step 8 | Matriculate to Med School |
Concrete actions for the next 12–24 months:
Academic audit + advising
- Get unofficial transcripts.
- Meet with a premed advisor or post‑bacc program director.
- Decide: DIY post‑bacc, formal post‑bacc, or SMP.
Start/refresh hard sciences
- At least: Gen Chem, Org Chem, Bio, Physics, Biochem, Psych/Soc.
- Aim for A/A‑ to show you’re not the same student you were at 19.
Get real clinical exposure
- Hospital volunteering
- Medical assistant, scribe, CNA, EMT
- Shadowing (including primary care and at least one specialty you think you want)
MCAT with a real plan
- 3–6 months of structured prep
- 4–8 full‑length practice exams
- Study schedule integrated with your actual life, not imaginary free time
Financial & life structure
- Rough 10‑year financial projection
- Plan for childcare, moves, partner career impact if relevant
If at any point during this, you realize: “This is miserable and I hate it,” that’s not failure. That’s success. You avoided a 10–15 year mistake.
9. If the Answer Is “No, This Isn’t Right” — What Now?
If, after honest assessment, medicine looks wrong for you at this age or situation, that does not mean:
- You’re weak
- You wasted your time
- You’ll never work in health care
You can still:
- Pivot to NP/PA/PT/OT or other advanced clinical roles with shorter training
- Move into public health, health administration, or health policy
- Work in clinical research, medical education, or patient advocacy
Plenty of people burn years chasing MD/DO when what they actually wanted was meaningful patient contact, respect, and autonomy — all possible in other roles without reconstructing your entire life.
Here’s your specific, actionable next step:
Tonight, block 60 minutes, no phone. Write down:
- Your current age
- Your best realistic “finish training” age
- Your honest scores (1–5) in the eight categories above
- One concrete step you’ll take in the next 7 days — either:
- Emailing a local premed/post‑bacc advisor with your transcripts, or
- Signing up for a college course to test your academic muscles, or
- Shadowing/volunteering in a clinical setting to confirm you want this life
Then look at that page and ask yourself:
“Knowing all this, do I still want to move one step forward?”
If the answer is yes, you’re not too old. You’re just getting started.




















