The belief that a preliminary year automatically turns into a PGY‑2 spot is dangerous—and wrong.
If you are counting on “I’ll just do a prelim and slide into a PGY‑2 later,” you are setting yourself up for one of the ugliest surprises in residency training: finishing a grueling year with no categorical position, no clear path forward, and a CV that suddenly looks unstable.
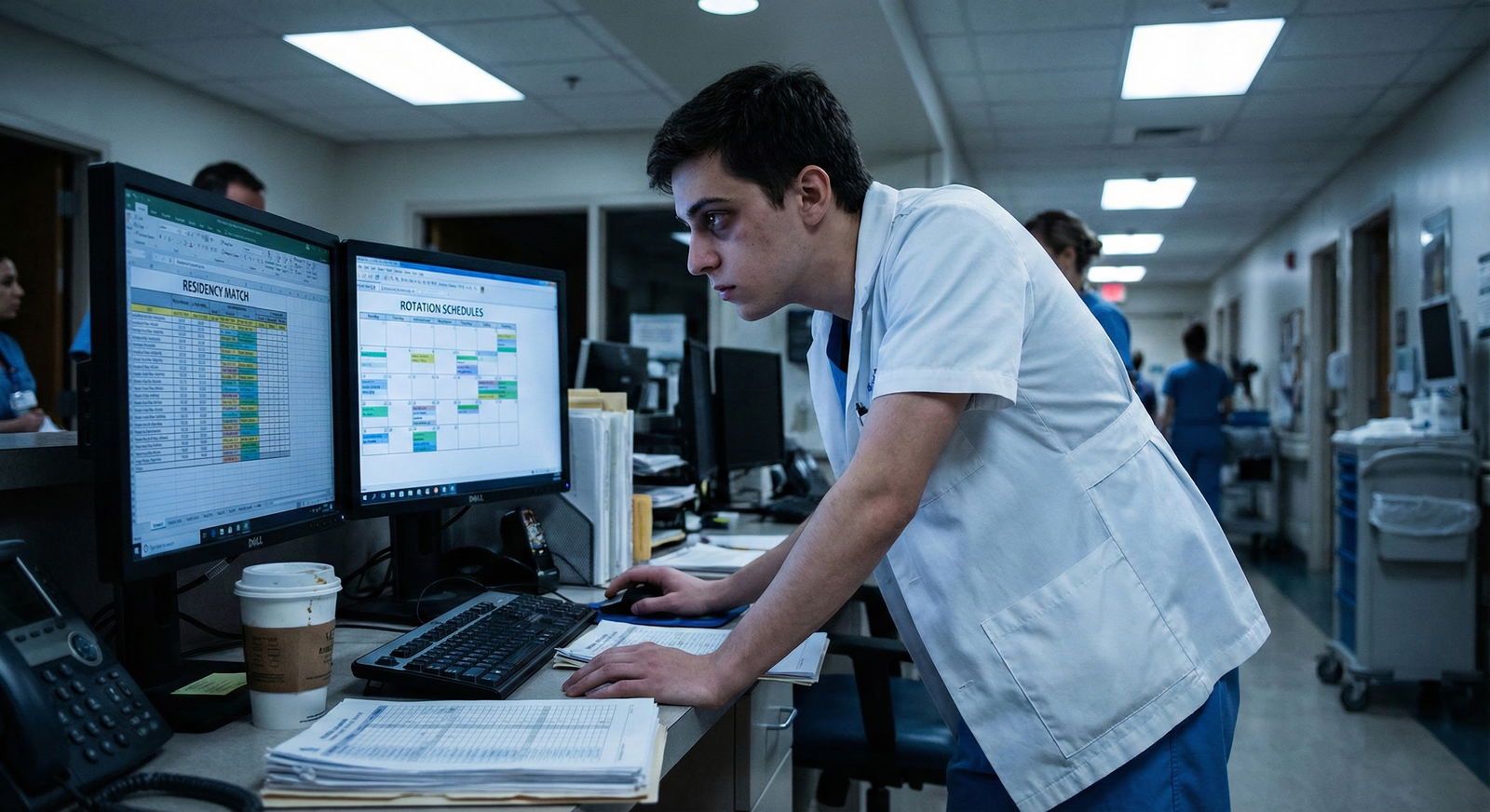
Let me walk you through the mistakes I see over and over—and how to avoid becoming the cautionary tale people whisper about in the call room.
What a Preliminary Year Actually Is (And What It Is Not)
A preliminary year is a one‑year residency position. Usually in internal medicine, surgery, or transitional year. It is designed to provide foundational clinical training.
The three most common purposes:
Required clinical base year for advanced specialties
Anesthesiology, radiology, dermatology, PM&R, radiation oncology, neurology, and similar fields often start at PGY‑2. They require you to complete either a prelim year or a transitional year first.Gap filler for unmatched applicants
Some people who do not match into their desired specialty take a prelim year hoping to “re‑enter” the Match stronger.Pure service positions for the hospital
Harsh, but true. Some prelim spots exist primarily to cover admissions, cross‑cover, and floor work with no guarantee of anything beyond July 1 to June 30.
Here is the crucial point:
A prelim year is a contract for one year of training. Not a promise of promotion. Not a backdoor into categorical PGY‑2.
You are hired for one PGY‑1 year only. Unless you match separately into a categorical or advanced position, that is all you are guaranteed.

The Central Misread: “If I Do Well, They’ll Keep Me”
The most common and costly error is mental:
“I’ll match a prelim year now, prove myself, and they will definitely take me into PGY‑2.”
No. They might. They often will not. And you have almost no leverage.
Here is what people forget:
- Many prelim programs do not even have corresponding open PGY‑2 categorical spots.
- Some have categorical spots, but they are already filled for the next 3–4 years.
- Others only occasionally have “unexpected” PGY‑2 openings—which are competitive and not automatically offered to the prelims.
I have heard interns say in June:
“I thought if I worked hard they’d just convert my prelim to a categorical spot.”
Their program director: “We never promised that. We do not have a position available.”
This is not a misunderstanding in the program’s eyes. It is your misread.
You avoid this by treating a prelim year exactly as it is: a fixed‑term job that ends in June, with zero default continuation.
Types of Prelim Years—and Their Hidden Risks
Not all prelim years are created equal. And choosing the wrong one, for the wrong reason, can cost you years.
Internal Medicine vs Surgical vs Transitional
At a high level:
Prelim Internal Medicine
Heavy on floor work, admissions, cross‑cover, ICU, consults.
Common for anesthesia, radiology, derm, PM&R candidates, and unmatched students.Prelim Surgery
Rougher hours, more call, a lot of scut, limited OR autonomy.
Used by those trying for categorical surgery or some surgical subspecialties.Transitional Year (TY)
Mix of medicine, outpatient, electives. Often cushier.
Popular for anesthesiology, radiology, derm, ophtho, radiation oncology.
The mistake: picking one purely because “it will be easier to land a PGY‑2,” without verifying if those PGY‑2s actually exist.
| Prelim Type | Typical Purpose | PGY-2 Guarantee? |
|---|---|---|
| Prelim Medicine | Base year or gap year | No |
| Prelim Surgery | Trying to reapply to surgery | No |
| Transitional Year | Required for advanced specialties | No |
| Categorical IM | Full residency to completion | Yes (if in good standing) |
Notice the only one with consistent progression? Categorical. Because it is designed that way.
The “Safety Plan” That Is Not Actually Safe
A lot of applicants approach prelims with this internal logic:
“I did not match categorical this year. I will take a prelim spot, work incredibly hard, get strong letters, and then either:
- slide into a PGY‑2 at the same institution, or
- reapply and be much more competitive next cycle.”
That can work. But many people sabotage themselves by neglecting one of the following:
- They do not secure an advanced PGY‑2 position in the same Match cycle.
- They do not confirm whether their prelim program ever converts prelims into categorical residents.
- They assume letter writers will rescue them without explicitly discussing timing, wording, and specialty targets.
- They underestimate how exhausted they will be during intern year and overestimate how much extra “application work” they can handle.
The worst‑case scenario is not theoretical. It looks like this in real life:
- You match into a prelim IM year only.
- You start residency in July. You are on nights by week 3.
- You barely have bandwidth to shower, much less polish a new personal statement.
- You miss some application deadlines or submit a rushed ERAS.
- Your letters go out late or generic.
- You do not match again. January comes. Your PD says, kindly but firmly, “We cannot offer you a PGY‑2.”
Now you are jobless in July with a single prelim year, no board certification path, and a large question mark on your CV.
The Structural Reality Programs Will Not Spell Out
You need to internalize something programs might not emphasize in the rush of recruitment:
Most prelim spots are created for service, not as a deliberate “trial year” for future categoricals.
From the hospital’s perspective:
- They need warm bodies to cover the night float, the busy medicine service, the surgical floor.
- Prelims are often cheaper and more flexible than adding categorical slots.
- Turning a prelim into a categorical means someone else (often a home medical student) might not get that spot.
Programs are not malicious. They are just not building their staffing model around your hope for a PGY‑2.
If you see a program with:
- 20 prelim IM spots
- 10 categorical IM spots per year
- No history of regularly converting prelims
You should assume: you are there to work one year and leave. Unless told otherwise explicitly and backed by numbers.

| Category | Value |
|---|---|
| Prelim IM | 18 |
| Categorical IM | 10 |
| Prelim Surgery | 6 |
| Categorical Surgery | 5 |
Look at that ratio. Where exactly do you think your “automatic” PGY‑2 is supposed to appear from?
Questions You Must Ask Before Ranking a Prelim Program
If you remember nothing else, remember this: If it is not explicit, it does not exist.
When interviewing or emailing programs, you need to ask direct, uncomfortable questions. Otherwise you are gambling with years of your life.
Here are the minimum questions:
“In the last 3–5 years, how many prelims have stayed on here as PGY‑2 categorical residents?”
Do not accept vague answers. Ask for actual numbers.“Do you ever convert prelim positions to categorical positions by design, or only in rare cases when someone leaves?”
If they say “only when someone leaves,” understand that you are waiting for a resignation, dismissal, or disaster. That is not a plan.“Do your prelims typically match into PGY‑2 positions elsewhere after their year here? What proportion?”
If many prelims finish and then disappear into non‑clinical limbo, that is a red flag.“For advanced applicants (e.g., radiology, anesthesia), do you have a shared process to coordinate our prelim year with our PGY‑2 start?”
Integrated planning is safer than you trying to patch it together alone.
Document these answers—because your memory will get fuzzy when you are stressed and on call.
The Timing Trap: Overlapping Match Cycles
Another critical misread: assuming you will “figure out” your PGY‑2 during intern year.
By the time you start a prelim year in July, you are already behind for the very next cycle’s PGY‑2 applications. The ERAS and Match timelines do not care that you are on nights.
Basic reality:
- Personal statement updates, new CV, program research: should be started before July 1.
- Identifying letter writers and explaining your plan: also before July 1.
- Many programs like to see late MS4 letters or early intern performance—but they will not wait forever for them.
If you walk into a prelim year with no plan for the coming Match, you are not “staying flexible.” You are walking straight into a timing ambush.

| Period | Event |
|---|---|
| Before Prelim Starts - Jan-Mar | Plan strategy and target specialties |
| Before Prelim Starts - Apr-May | Draft ERAS, ask for letters |
| Prelim Year - Jul | Start prelim PGY1 |
| Prelim Year - Sep | ERAS applications due |
| Prelim Year - Oct-Feb | Interviews while working full-time |
| Outcome - Mar | Match results |
| Outcome - Jul | Potential PGY2 start or gap year |
Notice how ERAS opens and interviews happen while you are drowning in intern duties. That is why “I’ll apply later once I settle in” is fantasy.
When a Prelim Year Makes Sense—and When It Is a Mistake
A prelim year can be a smart move. I am not telling you to avoid them entirely. I am telling you to stop treating them as guaranteed stepping stones.
Reasonable uses of a prelim year:
- You have an advanced PGY‑2 position already secured in the same Match, and the prelim is simply your base year.
- You truly need more clinical exposure and fresh letters to reapply in the same or a different field, and you have a concrete application plan and mentor buy‑in.
- You are willing to accept the risk of not matching again and pivot out of clinical training if needed.
Bad reasons to do a prelim:
- “I just need to be inside a hospital; they will see how good I am and want to keep me.”
- “Any residency is better than no residency.” (No. A dead‑end residency can be worse.)
- “I will figure out my specialty once I start.”
- “My advisor said prelim is a good safety net.” Without spelling out the risk.
If you are not emotionally prepared to finish the year with no PGY‑2, pause. A research year, an MPH, or a structured reapplication strategy might be safer for you than a random prelim.
How to Protect Yourself If You Accept a Prelim Spot
Let us say you have thought this through and still choose a prelim year. Fine. Then do it like an adult who understands the risk, not like a passenger hoping the plane lands itself.
Safeguards:
Get clarity in writing
Check your offer letter and any follow‑up emails. There will almost never be an explicit promise of PGY‑2. Do not pretend there is one.Build relationships early
By September, your PD and at least one APD should know your career goals and your PGY‑2 application plan. Not in a vague “I like cards or maybe GI” way. Specific.Secure letters early and explicitly
Ask attending physicians directly:
“I am reapplying to [specialty]. Would you be comfortable writing a strong letter supporting me this fall?”
Do not assume they will remember on their own.Protect your reputation ruthlessly
A prelim year amplifies any concern: professionalism flags, poor communication, repeated lateness. Programs see you as “temporary” already. You do not have slack.Have a backup to your backup
If you do not match into a PGY‑2 after this year, what then? Research? Additional non‑ACGME fellowship? Non‑clinical role? You may never need it. But you will sleep better if you know your contingencies.

Red Flags in Prelim Programs That Should Make You Pause
There are some patterns I have seen that correlate strongly with unhappy prelims:
- A large number of prelim residents and very few categorical residents in the same department.
- Programs that dodge your questions about past prelim outcomes: “Our residents do well!” with no specifics.
- Prelims consistently doing the worst rotations, the heaviest call, with minimal teaching or mentorship.
- No official advising system for prelims at all. You are just extra bodies.
- Residents telling you off the record: “Most prelims have to scramble or go elsewhere. It is rough.”
If you hear phrases like “we treat prelims just like categoricals” but cannot find any prelim who actually stayed on to PGY‑2 in the last few years, believe the actions, not the script.
Summary: The Key Things You Must Not Misread
You can make a prelim year work for you. But only if you stop lying to yourself about what it guarantees.
Two or three things to keep front and center:
- A prelim year is one year only, with no automatic PGY‑2—if you want continuation, you must secure it separately.
- Programs use prelim spots primarily for service, not as an unofficial try‑out for categorical positions, unless explicitly structured that way.
- If you choose a prelim, treat it as a high‑risk, high‑effort bridge, not a safety net; plan your next Match cycle and your backup plan before July 1, not after.
Protect yourself. Ask the hard questions now, instead of standing in June as a tired intern, realizing the “guarantee” you were banking on never actually existed.
FAQ
1. If I match a prelim internal medicine year and do really well, what are the realistic chances I can stay for PGY‑2?
It depends entirely on the specific program’s structure and vacancy history. Some programs regularly convert a small number of prelims (for example, 1–2 per year) when categoricals leave or extra funding appears. Many never convert prelims at all. You should ask for concrete numbers from the last 3–5 years: “Out of your prelim class each year, how many typically continue here as PGY‑2 categoricals?” If the answer is “almost never,” you must assume your chances are extremely low regardless of performance.
2. Is a transitional year safer than a prelim medicine or surgery year for getting a PGY‑2 spot?
Transitional years are not inherently safer; they are simply more flexible and often less grueling. They do not by themselves increase your probability of landing PGY‑2 unless they are paired with an already secured advanced position (for example, TY + advanced anesthesia). If you do not have an advanced spot locked in, a TY still ends after one year with no guarantee. Your chances depend more on your specialty competitiveness, application strength, and program support than on the prelim vs TY label.
3. If I do not match into PGY‑2 after a prelim year, is my career over?
No, but your path becomes more complex and narrower. You may pursue research positions, non‑ACGME fellowships, additional degrees, or non‑clinical roles while reassessing whether another Match attempt is realistic. Some individuals eventually re‑enter training; others transition fully out of clinical medicine. The key is to anticipate this possibility before starting the prelim year, so you are not blindsided and paralyzed if it happens. A thoughtful contingency plan can turn a setback into a pivot instead of a dead end.




















