Wanting to quit residency doesn’t automatically mean you’re not meant to be a doctor.
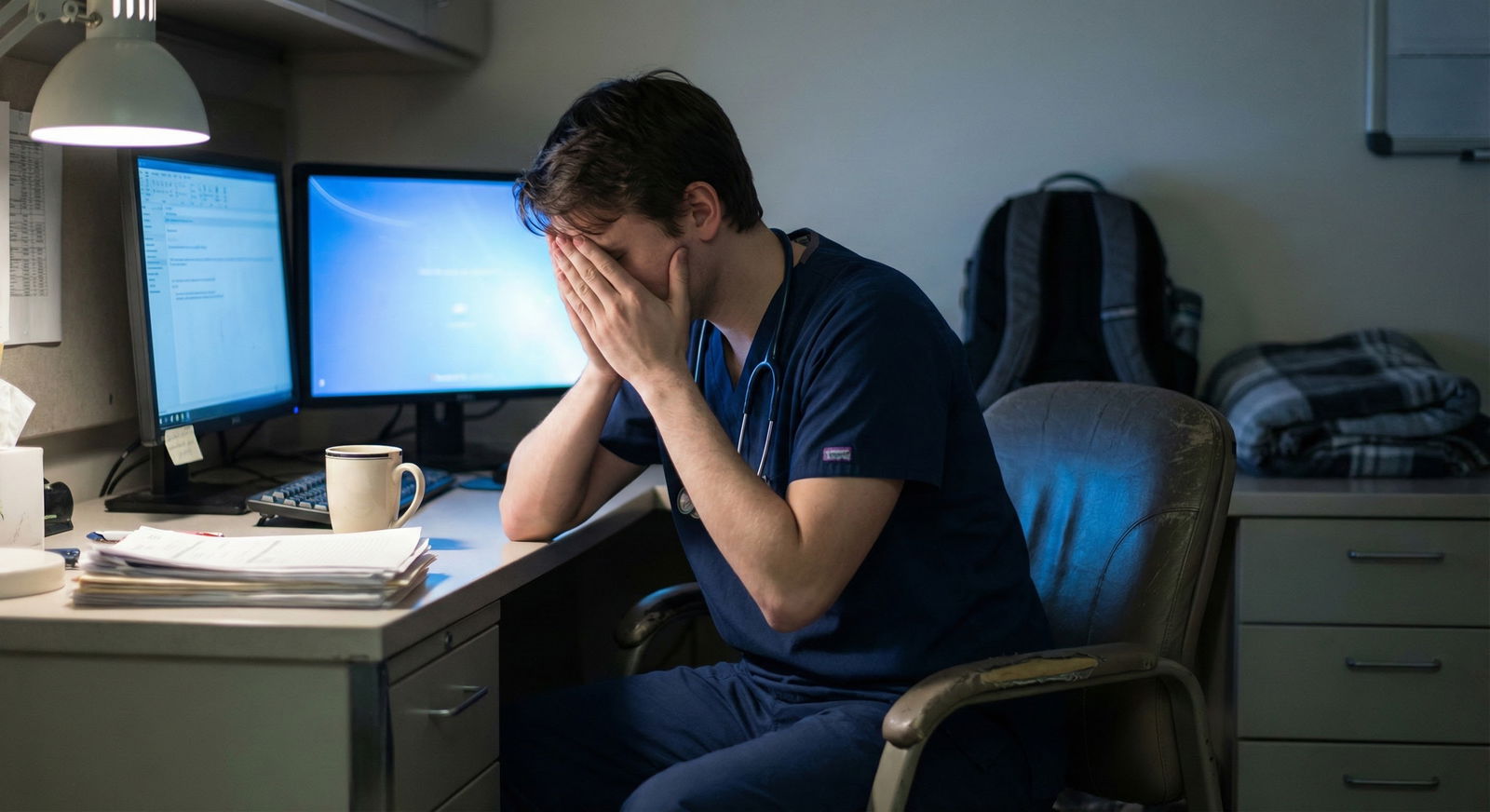
Let me start there, because the shame around this is brutal. You’re dragging yourself to every shift thinking, “I hate this, I dread this, what is wrong with me?” Meanwhile everyone else looks fine on rounds and you’re quietly wondering if you’re the only broken one.
You’re not. I promise you’re not.
But here’s the harder truth: sometimes it is the right move to leave a program. And sometimes you’re in the middle of a horrible but survivable season that will get better if you adjust, get support, and push through.
The real nightmare is not knowing which one you are.
Let’s walk through this systematically, like you’d work up a crashing patient. Because right now, you’re the patient.
First Question: Are You Safe Right Now?
I’m not starting with career strategy. I’m starting with you not falling apart.
If any of this sounds like you, this is not a “think about it for a few months” situation:
- You’re having frequent thoughts like “If I got in a car accident on the way to work, that wouldn’t be so bad.”
- You’ve thought about self-harm, disappearing, or just “not wanting to be alive” anymore.
- You’re making scary mistakes because you’re so exhausted or detached you barely remember your shifts.
- Panic attacks before shifts are so intense you can’t breathe, you’re vomiting, or you’re frozen.
That’s not “normal residency misery.” That’s a crisis.
You still have options, even if it feels like everything will explode if you say a word.
Here’s the harsh reality and the hope side by side:
- Programs do worry about liability and performance.
- But they also know residents burn out and they’ve seen people step back and then return.
If you’re at that edge, your first move is not “Do I quit forever?” It’s: “How do I get myself stabilized enough to even make a rational decision?”
That might look like:
- Talking to someone outside the program (therapist, doctor) this week, not “when things calm down.”
- Using employee health or resident wellness if you trust it even a little.
- Considering medical leave or a brief leave of absence as a bridge, not a failure.
You’re allowed to pause. It’s terrifying to consider, but I’ve seen people step out for a month or two and come back like different humans.
If you’re in active crisis, I’m going to say this bluntly: get emergency help now, not after the next shift. Your license, your career — none of it matters if you don’t survive this.
Is This “Normal Bad” or “Wrong Program/Wrong Path” Bad?
This is the question that keeps spiraling in your head at 3 a.m., right?
“Am I just weak? Or is this genuinely not right for me?”
Let’s break it into categories. Because your brain is lumping everything together and calling it “I suck.”
1. The Pain That Often Does Get Better With Time
These are things that usually improve by PGY2–PGY3 or with better support:
- Constant anxiety about not knowing enough
- Feeling slow on notes and orders
- Dreading specific people (one toxic attending, one malignant senior)
- Exhaustion from new schedules and night float
- Feeling like you have no identity outside the hospital yet
If most of your dread is tied to:
- “I’m scared I’ll miss something.”
- “I feel stupid all the time.”
- “I’m always behind.”
- “I can’t imagine doing this for years.”
That often gets better as competence and confidence grow. Your brain can’t imagine a future version of you that’s more skilled and calmer, but that version usually exists.
2. The Pain That Often Means Deeper Mismatch
These are red flags that you might be in the wrong program or even the wrong specialty:
- You fundamentally don’t like the core work of your field
(e.g., in IM you hate rounding, hate chronic disease, hate talking to patients’ families; in surgery you hate the OR and procedures) - You feel morally misaligned with the culture
(e.g., “work until you drop,” cutting corners, disrespect to patients or nurses, punitive teaching) - You feel no joy, ever, even on the “easier” days
- You’d choose almost any other reasonable career over what you’re doing now if starting fresh
Here’s the pattern I’ve seen too many times:
A resident is miserable but tells themselves, “All residencies suck, suck it up.” They ignore the part of them screaming, “This isn’t just hard. It’s wrong for me.” By PGY3, they’re half-checked-out, burnt to a crisp, and still terrified to make a change.
Residency is supposed to be hard. It’s not supposed to feel like a personality transplant where every day you become a worse version of yourself.

| Category | Value |
|---|---|
| Overload but aligned | 45 |
| Program mismatch | 25 |
| Specialty mismatch | 20 |
| Acute crisis | 10 |
A Blunt Checklist: Stay and Push, or Seriously Consider Leaving?
None of this is perfect. Life isn’t a neat flowchart. But here’s a rough framework.
Signs You Might Want to Try to Push Through (With Changes)
If at least most of these are true, I’d lean toward: don’t nuke everything yet, but change how you’re doing this:
- You used to like this specialty at least a little (med school rotations, early intern year).
- There are some moments you enjoy (a good patient interaction, a procedure, a teaching moment).
- You have at least 1–2 attendings or residents you respect and feel safe with.
- The main issue feels like volume, hours, or specific personalities — not hatred of the actual work.
- When you imagine being an attending in your field, you feel tired but not horrified.
- If someone said, “You could do the same specialty in a more humane program,” your body feels lighter.
In that scenario, the plan isn’t “white-knuckle through it.” It’s: “How do I survive and improve the next 6–12 months without destroying myself?”
We’ll get to tactics in a minute.
Signs You Should Seriously Consider Changing Programs or Leaving the Path
If several of these hit hard, you owe it to yourself to explore an exit or a pivot seriously, not just as a fantasy:
- Thinking about your future self as an attending in this field fills you with dread, not just fatigue.
- You feel depersonalized: like you’re acting through a role, not yourself, most of the time.
- You don’t respect the values you see modeled by most attendings in this specialty.
- You can’t identify any version of the job — academic, community, outpatient-heavy, part-time — that feels sustainably okay.
- When you imagine a totally different path (another specialty, non-clinical, earlier interest), you feel a quiet sense of relief rather than just panic.
- You’ve been this miserable for at least 6–12 months with no real improvement despite trying to cope.
Notice I’m not saying “if you’re sad, just quit.” I’m saying: if the core of who you are and what you value is at war with your training environment or specialty, ignoring that is the fast lane to severe burnout or walking away from medicine entirely later.

| Step | Description |
|---|---|
| Step 1 | Constant dread of shifts |
| Step 2 | Seek urgent help and consider leave |
| Step 3 | Explore switching specialty or leaving |
| Step 4 | Explore transfer or support |
| Step 5 | Adjust coping and stay short term |
| Step 6 | Crisis safety issue |
| Step 7 | Core work misaligned |
| Step 8 | Program vs you |
If You Stay (For Now): How to Make It Less Soul-Crushing
Say you decide, “I’m not quitting. At least not yet.” That doesn’t mean your only option is to grind yourself into dust.
Here’s what I’d look at, step by step.
1. Short-Term: Stabilize the Bleeding
Stuff that helps in days–weeks, not years:
Sleep protection that isn’t fantasy-level perfect
Maybe you can’t get 8 hours every night. But you can:- Stop scrolling in bed until 2 a.m.
- Use earplugs/eye mask on call room naps.
- Guard post-call sleep like it’s a procedure — no errands, no “I can just power through.”
One trustworthy person who sees the unfiltered version of you
One co-resident you text “I’m losing it” to. A partner who knows the real story, not the sanitized version. You need one person who doesn’t respond with “you’ll be fine, everyone’s tired.”A tiny daily anchor that’s not medicine
Ten minutes of something that reminds you you’re a person: a short walk outside before you go home, a podcast you love, one chapter of a dumb novel, a quick workout. Not as a self-care cliché. As a way of telling your brain, “We exist outside of this.”
2. Medium-Term: Make This Program Work For You
If you’re going to stay, squeeze some value out of it:
Find rotations that hurt you less
If you dread ICU but can tolerate clinic or electives, talk to chief residents or the PD about adjusting schedules down the line. You don’t have to say “I hate everything,” you can say, “I feel I’m really growing in X and would love more of that.”Identify one attending who isn’t terrible and ask for advice
Not “I want to quit” on day one. More like:
“I’m really struggling with dread before shifts and I’m not sure if it’s just normal adjustment or something deeper. How did you know you were in the right place back in training?”Dial back perfectionism by 20%
You’re not responsible for fixing a broken healthcare system.
Stop:- Writing the world’s longest notes that no one reads.
- Staying 2 hours past shift every day to catch every micro-detail.
- Taking every bad outcome as proof you’re incompetent.
You will make mistakes. Some will haunt you. That doesn’t mean you’re unfit for medicine.

If You’re Leaning Toward Leaving: What Actually Happens?
This is the part nobody talks about in detail. All you see are horror stories on Reddit or vague anecdotes about “someone who left and disappeared.”
Let’s be concrete.
There are 3 main paths if you decide this program/specialty isn’t it:
- Transfer to another program in the same specialty
- Switch specialties and restart or join a different program
- Step away from residency altogether (temporarily or permanently)
1. Transferring Within the Same Specialty
This is more common than people think, but it’s under the radar.
Pros:
- You keep your general path (e.g., still IM, still peds).
- You may get a healthier environment, location closer to support, or different culture.
- Some of your training time can transfer.
Cons:
- It can be politically messy. You need someone to vouch for you.
- Programs will want to know why you’re leaving. You can’t say, “I hate my PD.”
- Timing can be unpredictable; there’s no centralized match for transfers.
Reality: You usually start by quietly talking to someone you trust: a chief, a mentor, or an attending outside your program. Then:
- Reach out to other PDs explaining your situation in a measured way: “Looking for a program that better matches X/Y,” not “My program is a nightmare hellscape.”
- Expect this to take time. Months, not days.
2. Switching Specialties
People do this. IM to anesthesia. Surgery to FM. Peds to psych. It’s not some forbidden move.
Pros:
- You might land in work that fits your personality and values better.
- You won’t wake up every day thinking, “I chose wrong and then stayed anyway.”
- Prior experience can make you a stronger applicant.
Cons:
- You may have to repeat training years.
- You might feel behind your peers, which sucks if you’re already feeling inadequate.
- Requires explaining your decision to new programs without sounding flaky or unstable.
What programs look for:
- A coherent story of why the new specialty suits you better.
- Evidence you’re not just “running away” from hard work.
- Good evaluations or letters despite your struggles.
You’re allowed to say:
- “I learned X about myself in this program.”
- “I realized I’m more aligned with [new specialty] because of A, B, C.”
- “I’m willing to do the hard work — I just want it to be in the right lane.”
| Path | Main Goal | Biggest Risk |
|---|---|---|
| Stay in current program | Build resilience, finish training | Prolonged burnout |
| Transfer same specialty | Better culture/fit | No open spots/timing issues |
| Switch specialties | Align work with personality | Extra years of training |
| Temporary leave | Stabilize mental health | Re-entry uncertainty |
| Permanent exit from med | Protect long-term well-being | Debt, identity turmoil |
3. Leaving Residency (At Least for a While)
This is the nuclear option in your mind, I know. Your brain probably screams:
“If I leave, I’ll never get another chance. I’ll disappoint everyone. I’ll be in debt forever. I’ll have wasted my entire life.”
I’ve heard all of that. Some of it has teeth. But here’s what’s also true:
Plenty of people take a leave of absence for health or personal reasons and either:
- come back to the same program,
- restart in a different program,
- or decide with a clearer head not to return.
A smaller but real number walk away from clinical medicine and build other careers: industry, consulting, teaching, tech, writing, public health, etc.
Is it easy? No. Does it make you a failure? No.
If you’re seriously considering stepping away, you must:
- Talk to a real lawyer or advisor about contracts, loans, and obligations.
- Get a therapist or counselor who understands medical training culture (this matters — some don’t).
Don’t do the midnight “I’m going to send a rage-quit email to my PD” thing. You deserve a plan, not a meltdown.

How to Talk About All This Without Setting Off Alarm Bells
This is the other fear, right? That the second you hint at struggle, people will label you “unsafe” or “unstable.”
Reality: yes, you have to be smart about what you say, to whom, and how.
Think in layers.
Inner Circle (Therapist, Trusted Friend/Partner)
Here you can say the ugly stuff:
- “I fantasize about quitting every single shift.”
- “I’m starting to hate patients.”
- “I’m scared of what I might do if this doesn’t change.”
No filtering here. You need a place where you’re not managing perceptions.
Semi-Trusted Faculty/Mentor
Aim for:
- Honest, but framed, language.
For example:
- “I’ve been dealing with a lot of dread before shifts, and I’m trying to figure out whether this is something I can work through within this specialty/program, or if it’s a sign I should consider other options.”
- “I’m committed to patient care and safety, but I’m running at a level of burnout that worries me long term.”
Notice:
- You’re not saying “I’m unsafe on the wards.”
- You are signaling distress and asking for guidance.
Program Leadership (PD, Chiefs)
This depends heavily on how safe they feel. Some are genuinely supportive. Some are performatively kind but politically ruthless. You probably already have a sense.
You can say:
- “I’m struggling and I’m getting help outside the program. I want to keep you in the loop because I’m committed to doing this responsibly.”
- “I’m exploring whether a schedule adjustment, leave, or other support might be needed if things don’t improve.”
You don’t have to dump your entire internal monologue on them. You just have to be honest enough that they’re not blindsided if you later request changes.

| Category | Value |
|---|---|
| Stay and improve | 50 |
| Transfer | 15 |
| Switch specialty | 20 |
| Leave medicine | 15 |
The Truth You Probably Don’t Believe Right Now
You’re not stuck in one irreversible path, even though it feels like it.
You can:
- Stay and make it more survivable.
- Leave this program and not be “blacklisted from medicine forever.”
- Pivot specialties and still have a meaningful, respected career.
- Decide medicine as practiced now isn’t compatible with your life and prioritize your health.
None of those options is painless. All of them are allowed.
What’s not sustainable is silently waking up every day thinking, “I dread every shift, I hate my life,” and doing nothing but hoping it magically feels different next month.
You don’t have to decide everything today. But you do have to do something different.
Even if that “something” is just sending one message:
“Hey, can we talk? I’m not okay.”
FAQ (Exactly 6 Questions)
1. How do I know if my dread is just normal intern misery versus a sign I should leave?
Look at pattern and duration. If your dread is mostly about feeling incompetent, overwhelmed, or scared of making mistakes, and you still have small moments of meaning or connection, that’s usually “normal bad” that improves with time and support. If it’s been 6–12 months of hating the core work, no joy at all, and deep misalignment with the specialty or program culture, that’s more “wrong fit” than “rough phase.”
2. Will leaving my program destroy my chances of ever working in medicine?
Not automatically. What matters is how you leave and how you explain it. A planned, documented leave or transition with honest but measured communication is very different from disappearing mid-rotation. People do transfer, switch specialties, or take leaves and still build solid careers. Is there risk? Yes. Is it a guaranteed career death sentence? No.
3. I’m scared to tell anyone I’m struggling. Won’t they see me as unsafe or weak?
Some people will judge you. That’s reality. But staying silent while you’re falling apart is worse. Start with safer people: therapist, trusted co-resident, partner, maybe a faculty mentor you’ve seen be kind to others. You don’t have to open with “I might quit.” You can start with “I’m struggling more than I expected and I need help figuring out what’s normal and what’s not.”
4. What if I stick it out and then regret wasting years in the wrong specialty?
That’s a real risk. The antidote isn’t panicking; it’s being intentional. Don’t just survive day to day. Actively gather data: What parts of the job drain you vs. give even 1% energy back? How do you respond to different rotations? Talk to attendings about their actual lives. If your gut keeps saying “wrong lane,” listen sooner rather than in PGY3 with a mortgage and kids and golden handcuffs.
5. How do I explain wanting to transfer or switch specialties without trashing my current program?
You focus on pull, not push. Less “My program is toxic,” more “I’ve realized I’m most energized by X type of patient/workflow, and I want a program that offers more of that.” You can acknowledge challenges (“I struggled with Y”) without making it a character assassination. Programs want to hear that you’ve thought carefully and you’re moving toward better fit, not just fleeing discomfort.
6. Is it ever “okay” to leave medicine completely after residency starts?
Yes. It’s your life. You’re not a public utility. The debt, the expectations, the sunk costs — they’re all real, but so is the cost of staying in a career that’s destroying your mental and physical health. People leave and go into tech, consulting, writing, business, public health, education. It’s messy. It’s not a fairytale. But it’s allowed. If you get to the point where staying feels like self-destruction, it’s more than okay to choose yourself.
Key points to walk away with:
- Dreading every shift is a warning sign, not a moral failing — and it deserves real attention, not just “pushing through.”
- You have more than two options; it’s not just “suffer in silence or quit forever.” There are middle paths: support, adjustment, transfer, switch, leave.
- You don’t have to solve your entire career this week — but you do need to tell someone what’s actually going on and start making one concrete move toward either support or change.



















