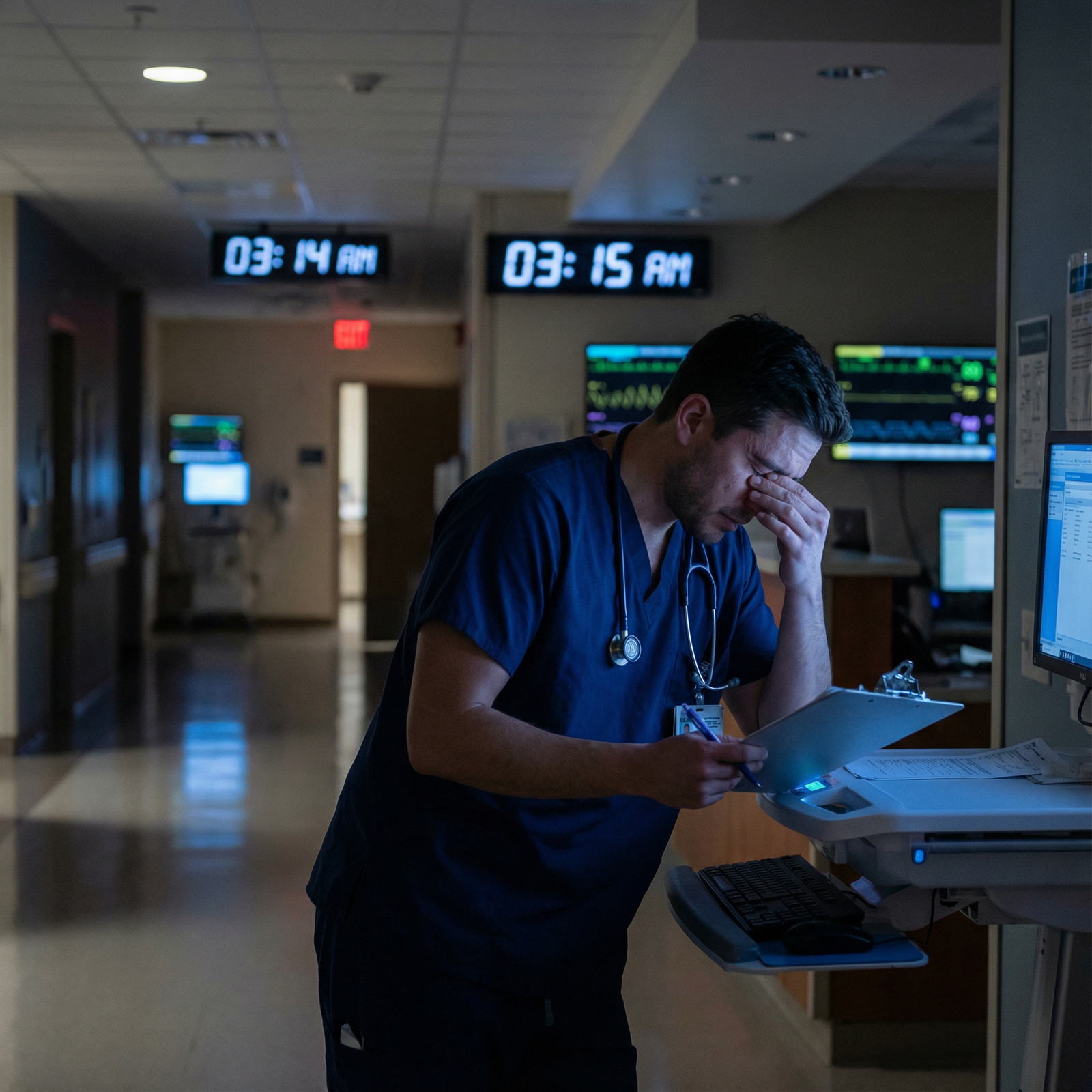
The way most residents handle night float is broken. They treat it like a brutal rite of passage instead of a system they can engineer and control.
You are not at the mercy of the pager. You are at the mercy of your systems— or your lack of them.
This is a blueprint to fix that.
1. Rebuild Your 24-Hour Clock: The Night Float Schedule That Actually Works
The biggest mistake I see? People think night float is “just staying up late.” It is not. It is a controlled time-zone shift that you either execute deliberately or suffer through.
Here is the principle:
Treat your week of nights like you just flew 6–8 time zones away. You would not keep your old schedule there. Stop trying to keep your “day” life alive while you are on nights.
The Core Night Float Sleep Template
Target for a standard 12-hour night shift (e.g., 7 pm–7 am):
Baseline template (for a 7 pm–7 am shift):
- 12:00–13:00: Wake up
- 13:00–14:00: Food, caffeine, move your body
- 14:00–17:00: Errands / study / admin / family
- 17:00–18:00: Nap
- 18:00–18:30: Pre-shift routine, commute
- 19:00–07:00: Shift
- 08:00–09:00: Wind-down, light snack, shower
- 09:00–13:00: Main sleep block
Most residents do the exact opposite: they wake mid-morning, run around all day, skip the pre-shift nap, slam caffeine at 21:00, and then wonder why they are hallucinating by 05:00.
You fix this with clear rules.

| Category | Value |
|---|---|
| Main Sleep (Daytime) | 60 |
| Pre-shift Nap | 15 |
| Awake before shift | 20 |
| Post-shift wind-down | 5 |
Non-Negotiable Sleep Rules
Main sleep block is sacred.
- 3.5–4.5 hours minimum, every “day.”
- Blackout curtains, white noise, earplugs, phone on “Do Not Disturb.”
Pre-shift nap is mandatory, not optional.
- 45–90 minutes. Set an alarm.
- If you skip the nap, your last 3 hours of the shift will be garbage.
Caffeine cut-off:
- Last real caffeine 5–6 hours before your planned main sleep.
- For a 09:00 bedtime: no caffeine after 03:00.
On your first night on:
- Sleep in late that morning (until 10–11:00).
- Take a 2–3 hour nap in the late afternoon (16:00–18:00).
- Go into the first night already partially shifted.
Post-call transition after your last night:
Do not “nap until 18:00 and ruin your reset.” That is how you drag the misery out for days.Use this pattern after your final night:
- 07:00–09:00: Go home, light snack, shower, sleep
- 09:00–13:00: Sleep (4 hours max)
- 13:00–20:00: Stay awake (sunlight, activity, no naps)
- 21:00–23:00: Go to bed for a normal night
You will feel like a zombie that afternoon. Tough it out one day. You get a faster reset instead of 3 days of half-functional fog.
2. Structure the Night: Block Your Time, Do Not Chase Tasks
If you let the night “happen to you,” you will spend 12 hours in low-grade chaos. Same pages, different names.
The fix: run the night in time blocks with clear priorities.
The Standard Night Float Time Blocks
Assuming a 7 pm–7 am shift:
- 19:00–20:30 – Front-load & stabilize
- 20:30–23:00 – Orders, cross-cover, batched work
- 23:00–02:00 – High-value tasks + sleep opportunities
- 02:00–05:00 – Defensive medicine and energy management
- 05:00–07:00 – Pre-round, tidy, and handoff prep
Let’s break what actually goes in each block.
19:00–20:30 – Front-load & Stabilize
Your job in the first 90 minutes is not to “ease into the night.” It is to eliminate landmines.
Handoff triage (5–10 minutes):
- Ask directly: “Who are you actually worried about between now and 07:00?”
- Write those MRNs on your “watch list” for the night.
See the unstable / high-risk patients early:
- New admissions that came in right before shift change
- Patients on pressors, non-ICU high-flow, borderline sats, GI bleeds, DKA, etc.
- Post-op patients < 12 hours out, especially big surgeries
Order anticipatory stuff while things are calm:
- PRN pain, nausea, insomnia meds
- Night-time bowel regimens for constipated post-ops
- Respiratory treatments for the wheezy COPD patient who always desats at 02:00
- Extra labs for patients trending the wrong way (electrolytes, H/H, lactate)
The question you should be asking: “What can I do now so I do not get paged at 03:00 for something predictable and dumb?”
20:30–23:00 – Orders, Cross-cover, Batched Work
This is usually your highest productivity window.
You:
- Return non-urgent pages in batches every 20–30 minutes instead of one-at-a-time every 2 minutes.
- Do admission orders with templates and checklists.
- Knock out cross-cover stuff while you are still sharp.
Paging rule:
When a non-emergent page comes in:
- Write it down immediately.
- Finish your current thought/task (unless it is a rapid response / real emergency).
- Call back during your next “batch page” interval.
You are not a vending machine. You do not need to answer every page in 3 seconds to be a good doctor. You need to be safe and efficient.
3. Create a Pager Strategy Instead of Just “Answer Faster”
The pager is not the enemy. Randomness is.
You cannot control when it goes off. You can control:
- How you capture interruptions
- How you triage them
- How you batch your responses
The 4-Level Triage System
Use a simple, explicit mental triage. I used to write a letter next to each page on my list.
- A – Drop everything (Code / RRT / obvious crash)
- B – High priority (needs action in 10–20 minutes)
- Acute chest pain, new hypoxia, real mental status change
- C – Routine (can wait 30–90 minutes if needed)
- Tylenol order, sleep med, low K in a stable patient
- D – Administrative / FYI (deal with when caught up)
- “Can we change this diet?” or “Family wants an update in the morning”
You can scribble something like:
- “Rm 534 – BP 80/40 – A”
- “Rm 612 – no bowel movement x3d – C”
Then handle A and B first, batch C and D.
The 3-Question Call-Back Script
Nurses are your best early warning system. You just need a clear, efficient way to get the information you need without 10 minutes of back-and-forth on every call.
When you call back, use the same script every time:
“What is the main thing worrying you right now?”
Cuts through noise. Forces focus.“How does this compare to this patient’s usual?”
New vs baseline is everything at 02:00.“What are the vitals and latest relevant labs?”
For:- SOB: O2 sat, respiratory rate, O2 device, CXR or ABG if done
- Hypotension: BP trends, HR, I/Os, most recent H/H, creatinine
- Confusion: Glucose, Na, recent meds, UTI workup, pain scores
If the situation sounds unstable or your gut feels off → go see them. You rarely regret laying eyes on a patient; you often regret not doing it.
4. Run Admissions Like a Production Line, Not Art
Night float admissions are where time disappears. One sloppy admission can cost you 45 minutes of rewriting wrong orders and answering fires all night.
The solution is boring and extremely effective: standardize.
Use a Rigid Admission Workflow
For every admission, run the same steps:
Skim quickly for danger:
- Chief complaint, vitals, triage note, initial labs/imaging.
- Ask: “Is this a sick admit who needs me now or a stable admit who can safely wait 30–60 minutes while I stabilize others?”
Bedside visit with a goal:
- Confirm the story in 3–5 minutes:
- “What brought you in tonight?”
- “Any chest pain, shortness of breath, fever, or new weakness now?”
- Focused exam: heart, lungs, volume status, mental status, focal neuro if relevant.
- Confirm the story in 3–5 minutes:
Order set first, details later:
- Use your EMR admission order sets.
- Hit:
- Diet
- VTE prophylaxis
- Bowel regimen
- PRNs (pain, nausea, fever, sleep)
- Monitoring level (tele vs floor)
- Critical labs / imaging
Then document:
- Structured note: Chief complaint, pertinent positives/negatives, clear assessment with 3–5 active problems max.
- Each problem gets a simple 1–2 line plan.
You are not writing a textbook case report at 01:30. You are creating a functional, comprehensible plan that the day team can pick up without hating you.
Admission Time Target
Make this your mental benchmark:
Routine admit (e.g., COPD mild flare, UTI, cellulitis)
- Goal: 25–35 minutes from pager to completed orders + note
Complex but stable (e.g., CHF exacerbation, DKA, new cancer diagnosis but stable)
- Goal: 40–50 minutes
Unstable (e.g., sepsis with hypotension, GI bleed, acute neuro change)
- No time goal. Stabilize first, chart later.
You will not always hit these numbers. That is fine. The goal is to have a yardstick so you recognize when an admission is dragging and ask: “What is bogging this down and can I simplify?”
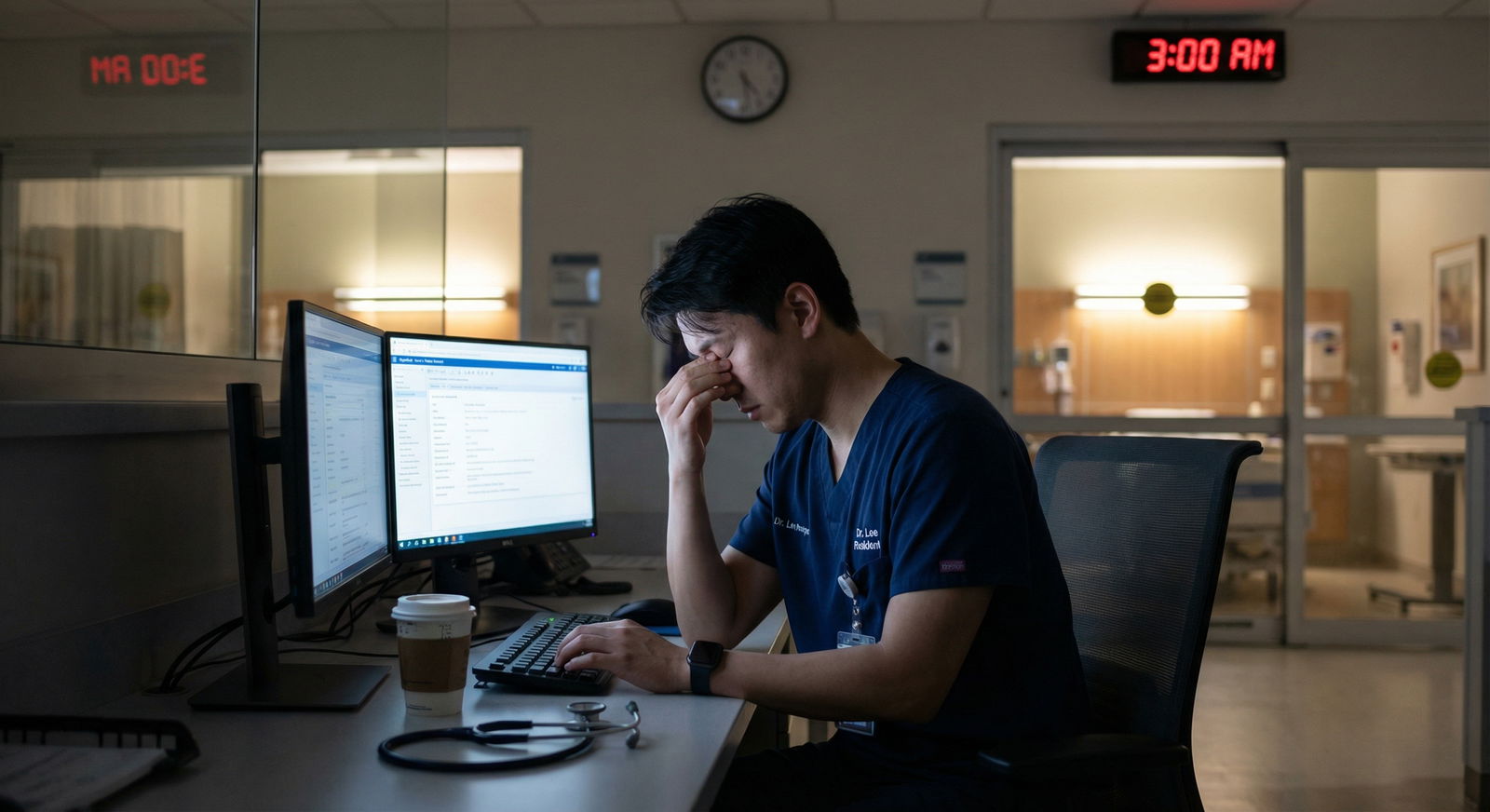
5. Protect Small Pockets of Rest Without Being Unsafe
No, you probably will not sleep 4 hours straight on night float. But you can often get 3–4 micro-blocks of 20–40 minutes if you plan for them.

| Category | Value |
|---|---|
| 19:00 | 0 |
| 21:00 | 10 |
| 23:00 | 20 |
| 01:00 | 35 |
| 03:00 | 30 |
| 05:00 | 15 |
| 07:00 | 0 |
Where the Rest Opportunities Usually Are
On most services, if the world is not on fire:
- 23:30–01:00
- 02:30–04:00
These are your “defend this time” windows.
How to Actually Make Rest Happen
Front-load and close loops before you try to sleep.
- Pending CT results you promised to check? Look before you lie down.
- Unaddressed C-level pages? Knock out 2–3 first.
Tell the nurse or operator how to reach you for real issues.
- “I will be in the call room for 30 minutes. If anything urgent / not routine comes up, page me twice.”
Double-page or phone call = get up.
- “I will be in the call room for 30 minutes. If anything urgent / not routine comes up, page me twice.”
Aim for multiple short blocks, not one huge block.
- Even 20–30 minutes of eyes-closed horizontal time helps.
- You are not weak for resting when you can. You are smart enough to maintain cognitive function.
Use the “4 am rule” for yourself: Ask: “How would I feel about performing this task or making this decision at 04:00 with no rest vs with 30 minutes of rest now?”
If the answer is obvious, you know what to do.
6. Use Checklists and Tools Instead of Your Tired Brain
Night float is not the time to prove how much you can keep in your head. It is the time to offload as much as possible to systems.
The Night Float Pocket Checklist
You want a 1-page reference you can keep folded in your pocket or on your phone. Here is what that should include:
High-yield “things that will get you burned if you forget”
- Anticoagulation plan (start/hold? indication?) on new admits
- VTE prophylaxis on all inpatients
- Home meds reconciliation (especially insulin, beta blockers, antiepileptics)
- Code status documented and communicated
- Telemetry indication (and when to stop)
Quick reference for common cross-cover issues
- Hypoglycemia treatment protocol (numbers + doses)
- Hyperkalemia STAT treatment bundle
- Common insulin adjustment rules
- Delirium basics (non-pharm, med review, when to actually use antipsychotics)
Red flag triggers
- “If SBP < 90 or MAP < 65 and not chronic, I will see the patient.”
- “If RR > 24, sats < 90% on baseline O2, I will see the patient.”
- “Any sudden change in mental status = go to bedside.”
You can build this once, refine it over a couple of months, and then never wing it again.
| Category | Item to Confirm on Every New Admit |
|---|---|
| Safety | VTE prophylaxis ordered |
| Medications | Home meds reconciled |
| Monitoring | Telemetry need documented |
| Code Status | Discussed and charted |
| Symptom Control | PRNs for pain, nausea, sleep |
7. Communicate So the Day Team Does Not Hate You (and You Sleep Better)
You know the feeling of walking in at 07:00, reading the night note, and thinking: “What was this person doing all night?” Do not be that person.
Build a Structured Handoff
Your goal from 06:00–07:00 is to hand the day team a clean board, not a mess.
Stepwise:
Update the sick list.
- For each high-risk patient, one line:
- “Rm 412 – GI bleed, Hgb from 9→7.6, transfused 1U, stable now, repeat Hgb at 10:00.”
- For each high-risk patient, one line:
Close the loop on outstanding tests with significant impact.
- If you ordered a head CT for new confusion at 01:00, try to know the result before sign-out.
- If pending, at least state:
- “CT head pending, ordered at 01:10 for new confusion; neuro exam non-focal at that time.”
Do not hide the near-misses or complications.
- “Rm 523 had SBP in the 70s at 03:00, got 1L LR, now 100/60. Lactate down from 4.0 to 2.6. Needs re-eval this morning.”
This builds trust. And protects the patient.
- “Rm 523 had SBP in the 70s at 03:00, got 1L LR, now 100/60. Lactate down from 4.0 to 2.6. Needs re-eval this morning.”
Keep notes short and functional.
- The best night notes are short, time-stamped, and specific.
- Example:
- “02:15 – Rm 315 acute SOB, sats 82% RA → 94% on 4L. CXR: pulm edema. 40 mg IV lasix, 2 doses nitrate paste, I/O strict, repeat BMP at 06:00.”

| Step | Description |
|---|---|
| Step 1 | Start 05 -30 |
| Step 2 | Review admissions |
| Step 3 | Update sick list |
| Step 4 | Check key pending results |
| Step 5 | Summarize overnight events |
| Step 6 | Face to face handoff at 07 -00 |
You are not writing a novel. You are arming the day team to keep these people alive and moving.
8. Protect Your Body So Your Brain Still Works at 04:00
You cannot time-manage your way out of physiology. If your body is wrecked, your decision-making is trash.
Baseline Physical Rules on Nights
Stop pretending you will “eat when you can.”
That always becomes: “I ate one donut at 02:30.”Do this instead:
- Bring real food:
- Protein + complex carbs + something with fiber.
- Example: chicken + rice bowl, bean salad, Greek yogurt with nuts, hummus + veggies.
- Schedule 2 small meals:
- 19:30–20:00 and 01:00–02:00.
- Bring real food:
Micro-movement > gym heroics.
- 2–3 times per night, pick 5–10 minutes to:
- Walk a lap of the unit.
- Do 10–15 slow squats or calf raises in a stairwell.
- This is not about fitness. It is about blood flow and staying awake.
- 2–3 times per night, pick 5–10 minutes to:
Hydration with a plan.
- Keep one refillable bottle at your workstation.
- Aim to finish 1 bottle by midnight, 1 by the end of shift.
- Avoid chugging water right before trying to sleep post-shift.
Guard your eyes and light exposure.
- Blue light is your friend at 02:00, your enemy at 09:00.
- Use bright light in the workroom during the night to stay awake.
- On the way home, sunglasses. Dark room at home. You are telling your body: “This is night.”
9. Mental Game: How to Not Let Night Float Break You
Time management on nights is not just logistics. It is mood, resentment, and mental load.
If you ignore this part, everything else becomes harder.
Set Clear Boundaries Outside the Hospital
During night float:
- You are unavailable for most daytime social events. Full stop.
- You do not take on extra projects or committees.
- Your main job:
- Do not harm patients at night.
- Protect your sleep.
- Keep your life from falling apart.
If you have a partner or family:
- Before your block starts, say plainly:
- “I will be on nights from [dates]. I will be basically jet-lagged. Let’s plan 1–2 anchor times we can actually connect, and give me permission to disappear the rest of the time.”
Then stick to it.
- “I will be on nights from [dates]. I will be basically jet-lagged. Let’s plan 1–2 anchor times we can actually connect, and give me permission to disappear the rest of the time.”
Use Simple Decompression Rituals
You do not “just fall into bed” and suddenly feel fine. Your nervous system is still in fight mode.
Use a 10–20 minute post-shift ritual:
- Quick shower
- Light snack or tea
- 5–10 minutes of something that is not a screen:
- Short guided breathing, a few pages of low-stakes reading, journaling a few lines about the night.
That last one is not soft BS. I have seen it prevent residents from bringing the entire hospital to bed with them.
10. Put It All Together: A Model Night on Float
Let me show you how this actually looks when it works.
Resident on medicine night float, 7 pm–7 am shift, 8th night in a 14-night block.
- 13:00 – Wake up. Quick breakfast + coffee. 10 minutes of light.
- 14:00–16:00 – Errands, light reading for boards, 20-minute walk.
- 16:30–18:00 – Nap. Dark room. Phone off.
- 18:00–18:30 – Shower, pack food, commute. No big caffeine now.
- 19:00 – Arrive, sign-out. Ask: “Who are you worried about between now and 07:00?”
- 19:15–20:15 – See 3 “sickest” patients, adjust a few orders, place PRNs.
- 20:15–20:30 – Eat meal #1 at workstation while scanning labs.
- 20:30–23:00 – Knock out 2 new admissions using standard workflow, batch pages every 20–30 minutes.
- 23:00–23:20 – Quick walk around the unit, check in with nurses: “Anyone making you nervous?”
- 23:20–00:00 – Calls / routine pages. Start identifying a 30-minute window for rest.
- 00:00–00:30 – Eyes-closed time in call room, pager on loud.
- 00:30–02:30 – 1–2 more admissions, check on sick list, review critical labs, eat meal #2 around 01:00.
- 02:30–03:00 – Another brief rest if pages allow.
- 03:00–05:00 – Defend cognitive function: walk a lap once an hour, hydrate, answer cross-cover issues, reassess anyone you were marginal on earlier.
- 05:00–06:30 – Start tidying charting, check labs on sick patients, place a few “morning labs” you know day team will want.
- 06:30–07:00 – Face-to-face handoff. Clean, specific.
- 07:30 – Home. Sunglasses.
- 07:45–08:05 – Shower, snack, 10 min wind-down, then bed by 08:30–09:00.
Is every night that clean? Of course not. You will have codes, absolute chaos, 8 admissions back-to-back. But if you have this as your default map, you bend the night toward order instead of surrendering to chaos.
11. Quick Blueprint Recap
You do not “survive” night float. You run it like a system.
Key points to lock in:
Engineered schedule, not vibes.
Treat nights like a time zone shift. Protect a daytime main sleep block and a pre-shift nap. Respect caffeine and light.Run the night in blocks with triage.
Front-load stabilization, batch pages, standardize admissions, and carve out small protected rest windows.Use tools so your tired brain is not the bottleneck.
Checklists, structured handoffs, simple scripts for nurse calls, and a nightly routine that protects both your patients and your sanity.
If you implement even half of this blueprint, your next night float block will feel completely different. Less chaos. Fewer dumb mistakes. More control.



















