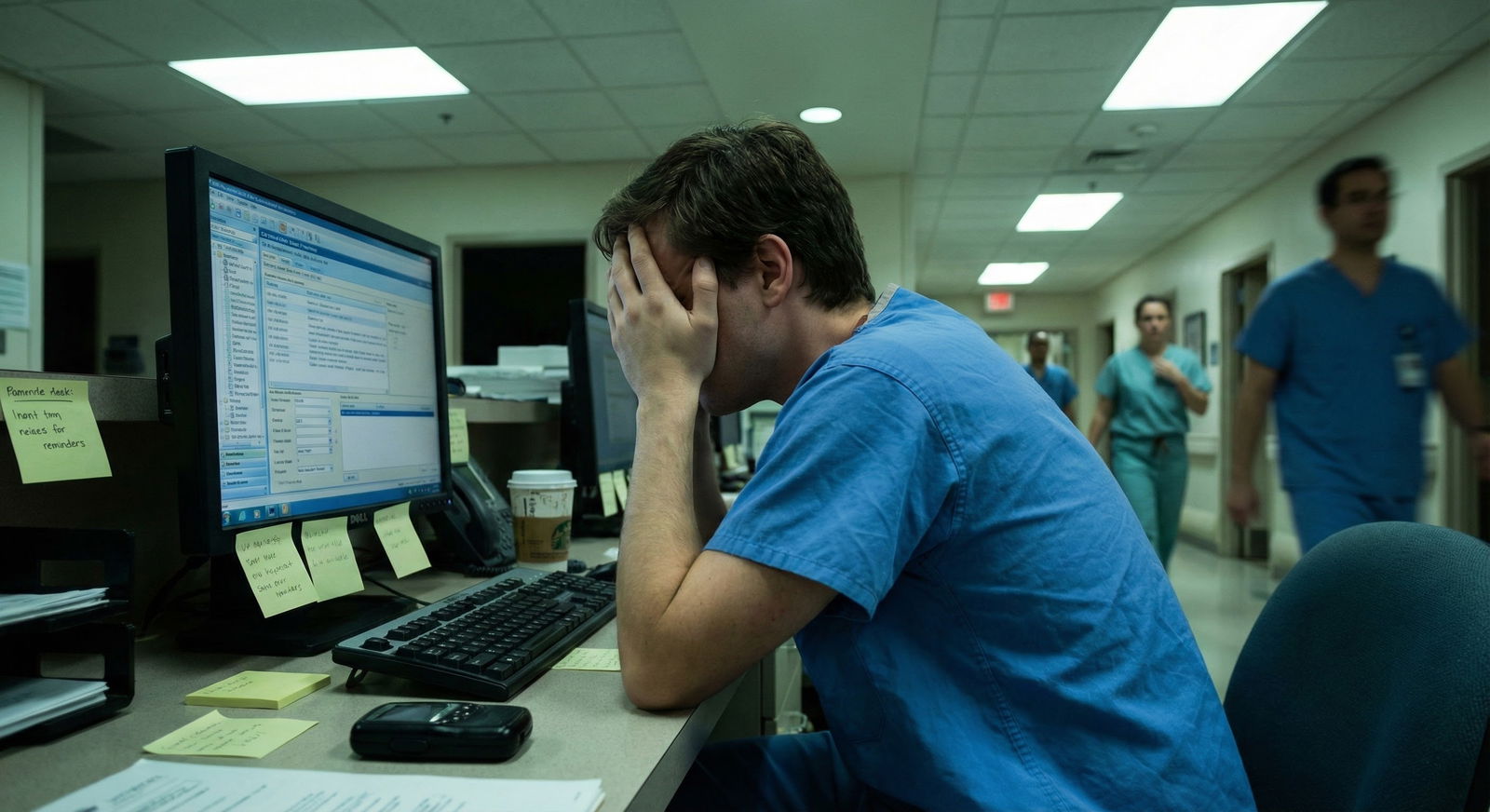
“If I can’t keep up, they’ll figure out I don’t belong here.” No, they won’t. But if you keep doing what you’re doing, you will burn out.
Let me say the quiet part out loud: most new interns are barely hanging on. The ones who look “on top of it” are usually just better at hiding the chaos.
You’re not the only one who’s deleted a page by accident and prayed it wasn’t important. Or stared at your to-do list at 2 pm and realized you never placed the 9 am order. Or gone to bed thinking: “I’m one more missed task away from someone getting hurt.”
That sick, heavy feeling that you’re dropping balls? That’s your brain telling you your current “system” (aka, vibes + panic) isn’t working.
This isn’t a willpower problem. It’s a systems problem.
Let’s fix the system.
First, the awful “what if” you keep replaying
What if I can’t keep up?
What if I miss something important?
What if someone gets hurt because of me?
What if my seniors decide I’m unsafe and shouldn’t be here?
Here’s the ugly truth I’ve watched play out over and over: the interns who get into real trouble aren’t the ones who struggle. They’re the ones who struggle silently, keep pretending they’re fine, and never change how they work.
The bar is not “never make mistakes.” The bar is:
- You notice when you’re slipping
- You put structure in place
- You communicate early
Everything I’m about to walk through is about one thing: pulling your brain out of chaos mode and into something semi-predictable so your actual clinical reasoning can show up.
Because right now, your cognitive bandwidth is getting eaten alive by logistics.
The brutal reality: you cannot remember everything. You need external brains.
If you’re trying to keep your day in your head, you’ve already lost.
You need 3 “external brains”:
- A brain for patients/tasks
- A brain for time
- A brain for communication
No, this is not overkill. The job is overkill.
1. Your patient/task brain: the list that actually saves you
You probably already have a patient list. Epic printout. Cerner list. Whatever. But if you only use it for names and room numbers, it’s not helping you.
You need a working list, not just a census.
Here’s the simple structure that kept me from missing critical stuff:
| Section | Purpose |
|---|---|
| Header | Date, service, your pager |
| Patient Block | One block per patient |
| Critical Flags | Unstable issues, recheck times |
| Task Area | Time-stamped to-dos |
Each patient gets a mini-block on your list with the same 4 lines, written by hand or typed every morning:
- ID line: Name / Room / Code status / Attending
- Today’s goals: 1–2 bullets max
- Critical follow-ups: labs, imaging, consults, re-exams
- Tasks with times: “1400 recheck K, 1500 update family”
That looks like:
Smith, J / 6-412 / Full / Dr. Jones
Goals: Wean O2 if able; clarify dispo with SNF
Follow-ups: F/u CT chest read; F/u pulm note
Tasks: 1100 check ABG; 1400 re-exam after neb; 1700 update daughter
Is it annoying to write this every morning? Yes.
Did it save me from forgetting to follow up a CT angio on a possible PE? Also yes.
The key detail: every follow-up item and every re-exam lives on this list. Never trust yourself to “remember to check that later.” You won’t. Not because you’re incompetent but because intern life is designed to obliterate your working memory.
2. The “time brain”: block your day like a slightly neurotic project manager
Wandering through the day “getting to things when I can” is exactly how you end up at 4 pm realizing you never wrote the transfer summary.
You need rough time blocks. They will get blown up. That’s fine. You still need them.
Think of your day in 5 predictable chunks:

| Category | Value |
|---|---|
| Pre-rounding/Data | 20 |
| Rounds | 20 |
| Orders/Notes | 25 |
| Afternoon Tasks | 25 |
| Sign-out/Admin | 10 |
Something like:
Pre-rounds (e.g., 5:30–7:00)
This is not “wander room to room doing full histories.” This is surgical strike mode:
- Check vitals, overnight events, new labs/imaging
- Update your list and your patient blocks
- Identify 1–2 main issues per patient for rounds
If you don’t have time to see everyone, prioritize: - Anyone unstable or with major overnight change
- New admissions
- Patients likely to leave today
Rounds (e.g., 7:00–10:00)
Stop trying to do 6 things at once. Don’t place every order during rounds. You’ll miss stuff and half-finish everything.
Use rounds to:
- Update your list with new plans in real time
- Mark tasks with clear time anchors (“before noon,” “this afternoon,” “stat”)
- Ask clarifying questions: “Do you want that CT before or after we see GI recs?”
Then, after rounds, you do a quick sort of your tasks:
- STAT/urgent now (call, orders, sick patients)
- Pre-noon must-do (discharges, procedures, time-sensitive orders)
- Afternoon okay (family meetings, non-urgent labs, social stuff)
This 5-minute sort is the difference between “I missed something” and “I knew what I was choosing to delay.”
The scary part: what if I still miss things?
You will. Everyone does.
The actual goal is not never missing anything. It’s catching things earlier and more reliably.
Here’s how you stack the deck:
Build in “audit points” to your day
Instead of trusting your brain, you schedule 3 very short, very specific self-checks. Set phone alarms if you have to (vibrate, short label like “11a TASK CHECK”).
I used 3 anchors:
Late morning check (11:00):
Quick scan of list:- Any labs/imaging ordered but not checked?
- Any “before noon” tasks unfinished?
- Any pending consults not called?
Mid-afternoon check (15:00):
- Any critical re-exams still not done?
- Any dispo stuff that will block a discharge if you wait (scripts, transport, DME)?
- Any notes that must be done before sign-out?
Pre-sign-out check (30–45 min before sign-out):
- Are overnight issues and “watch” items clearly written in sign-out?
- Any tasks I can safely finish before handing off?
Those 3 pauses are where a lot of “I almost missed that” stuff gets rescued.
The pager: where your brain goes to die
You know that feeling when you’re actually focused on something and then you get 6 pages in 4 minutes and your entire nervous system lights on fire? Yeah.
You can’t control the volume, but you can reduce the chaos.
One rule that changes everything: every page becomes a written item
Never handle a page entirely in your head. When you get a page:
Write a tiny note on your list (or a separate “pager scratchpad”):
“Rm 624 – pain; Rm 610 – BP 80s; RN Sarah – call back re: 5W”Then triage on paper:
- “Stat now”
- “Soon”
- “Can wait 30–60 min”
A lot of interns try to immediately fix every page in real time. That’s how you end up half-doing five different things and fully finishing none of them.
It’s not unsafe to call back and say:
“Got your page, I’m currently managing a hypotensive patient. I’ll be there in about 20 minutes for the pain med adjustment. If anything changes before then, page me again.”
It is unsafe to forget they paged at all.
EMR overload: use it like a tool, not a maze
Intern brain at 2 pm: “I know I saw that lab somewhere.”
EMR: 46 open tabs, 19 alerts, 3 half-started notes, 0 mercy.
Two fixes that actually help:
1. Standardized note templates (even if your program gives you crappy ones)
You are allowed to make your own. You should.
Have a soap/H&P/discharge template that includes:
- A “Problems Today” section (top 3 active issues)
- A “Follow-ups Pending” section: labs, imaging, consults
- A “To-do Before Discharge” section for transitions
You’re not just making your notes look pretty. You’re forcing your brain to think in the same structure every time. That repetition is where speed and safety come from.
2. EMR favorites and filters
This sounds tiny. It’s not.
Spend 20–30 minutes once setting up:
- Favorite order sets for your most common things (pneumonia, CHF, DKA, post-op, etc.)
- Favorite labs (CBC/BMP/Mg/Phos/lactate) so you’re not searching 40 times a day
- A “my patients” filter so your census view is clean
That half-hour on a calmer day will save you hours when you’re drowning.
Communication: the thing that terrifies you but saves your reputation
Here’s the nightmare:
You’re behind. You’re embarrassed. You’re scared your senior will think you’re incompetent. So you keep your head down and “try to push through.”
Then at 6 pm: multiple unfinished notes, families not updated, discharge not done, overnight team left with a mess. Now you do look unsafe.
Counterintuitively, the interns who own their limits early look more competent, not less.
You want phrases you can steal. Use them verbatim:
With your senior, before it’s a disaster:
- “I’m running behind on notes and haven’t gotten to two discharges yet. Can you help me prioritize what absolutely needs to be done before sign-out?”
- “I’m worried I’m missing something. Here’s my list—can you quickly look at my active tasks and see if I’m overlooking anything high-risk?”
- “My system clearly isn’t working. Can I show you how I’m organizing my day and get your feedback?”
With nurses:
- “I’m juggling a few urgent things. I hear your concern, and I’m planning to come see him in about 20 minutes. If his pain worsens or vitals change before that, page me again right away.”
- “Can you help me by letting me know which issues you see as highest urgency so I can triage appropriately?”
The difference between “overwhelmed but safe” and “dangerously behind” is almost always how early you loop people in.
The emotional spiral: “Everyone else is handling this. Why can’t I?”
They’re not. Some are coping better. Some are absolutely not. A lot are just better at looking calm while internally screaming.
I’ve seen interns with:
- 260+ Step 1 scores
- Honors everything
- Glowing letters
…break down on night float because they couldn’t keep a running task list and lost track of two critical labs.
This is not an intelligence test. It’s an endurance and systems test.
And honestly? A poorly designed one.
So if your brain feels like it’s short-circuiting, it doesn’t mean you’re not cut out for this. It means you’re trying to brute-force a job that requires structure.
A simple “rescue plan” for days you feel like you’re drowning
You know those days where you’re so behind you don’t even know where to start? Here’s a 10–15 minute reset I’ve walked people through at the workstation when they were on the verge of tears.
Step 1: Hard stop (2 minutes)
Stop clicking. Stop half-writing a note. Take a literal pause. If needed, tell your senior:
“I’m really behind and I’m worried I’m missing things. I need 10 minutes to get organized so I can be safer.”
They’d rather you do that than quietly drown.
Step 2: Rebuild your task list from scratch (8–10 minutes)
Grab your list. For each patient:
- Write their name and room
- Write today: 1–2 goals
- Underneath, list every active task you can think of (orders, follow-ups, calls)
Then add:
- Pages you haven’t completed
- Notes still unwritten
- Discharges pending
It will look horrifying. That’s okay. At least now the monster is on paper where you can see it.
Step 3: Mark things with three symbols (3 minutes)
Next to each task, mark:
- “!” for urgent/safety-critical issues (hypotension, concerning labs, unstable patients)
- “D” for dispo/time-dependent (discharge scripts, transport, important family calls)
- “N” for things that truly can be done later or tomorrow if needed
Now look at your “!” items. Those are non-negotiable. If there are too many “!” for one person in the remaining time, this is when you must pull in your senior:
“Here is my list of urgent things. I don’t think I can safely complete all of these before sign-out. Can you help me redistribute or decide what to hand off?”
This is what safe practice looks like when the system is unreasonable. Not martyrdom.
You’re not failing. You’re under-resourced.
You keep asking yourself: “What if I can’t keep up?”
The real question is: “What if I keep trying to do this job with no real system?”
That’s when interns burn out. That’s when mistakes compound.
You’re allowed to:
- Use timers and alarms
- Write things down obsessively
- Ask for help before you implode
- Tell your senior your brain is maxed out
None of that makes you weak. It makes you functional in an environment that’s frankly hostile to human cognition.
You’re not supposed to keep every patient, every lab, every family, and every order in your head. If you could, you’d be a liability, because you’d be relying on memory instead of checks.

| Step | Description |
|---|---|
| Step 1 | Overwhelmed |
| Step 2 | Hard stop 10 minutes |
| Step 3 | Rebuild task list |
| Step 4 | Mark urgent vs later |
| Step 5 | Talk to senior early |
| Step 6 | Safer prioritized plan |


| Category | Value |
|---|---|
| Too many tasks | 90 |
| Poor system | 80 |
| Pager chaos | 75 |
| EMR overload | 70 |
| Fear of asking help | 65 |


Here’s your next step. Don’t overthink this.
Today, before your next shift (or on your next break), do exactly one thing:
Create a one-page patient template and decide on your three daily audit times (for example: 11:00, 15:00, 30 minutes before sign-out). Write them down. Set alarms if you need to.
Then tomorrow, use that template and those three checks for every single patient.
Not forever. Just for one week.
If after that week you’re not missing fewer things and feeling even slightly less panicked, fine—throw it out and we’ll try something else.
But start by opening a blank sheet of paper right now and writing:
“Patient name / Room / Goals today / Follow-ups / Tasks with times”
That’s the first brick in a system that can actually carry the weight you’re under.




















