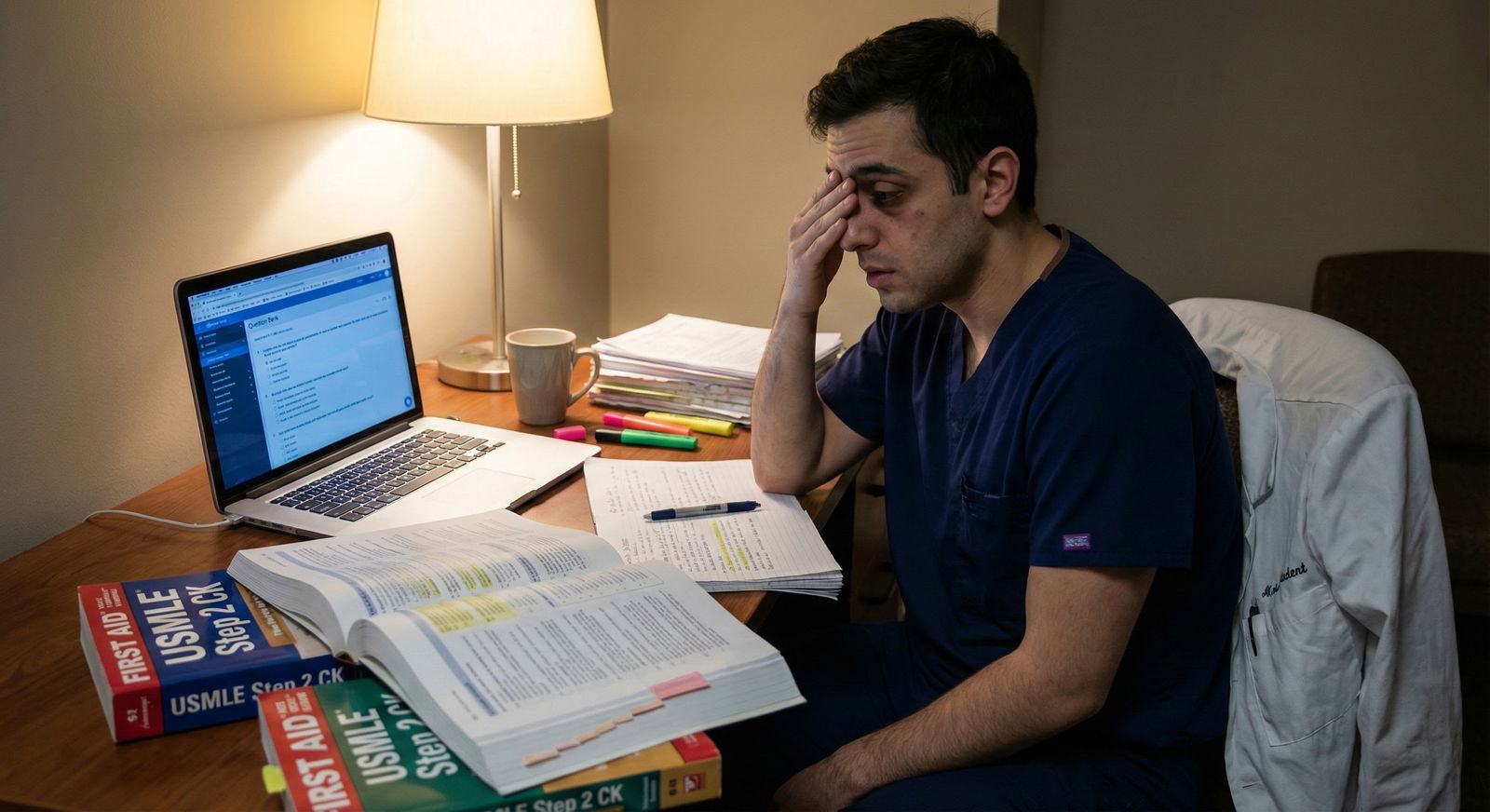
You’re post-call, half asleep in a call room, scrolling through your phone. Step 3 is three months away. Your plan—if you can call it that—is “reuse my Step 2 CK notes and hammer a Qbank.”
You tell yourself:
“I crushed Step 2 CK using these notes. Why reinvent the wheel?”
Here’s the problem.
That exact mindset is why strong Step 2 test-takers quietly get wrecked on Step 3. Not because they’re suddenly dumb. Because they’re using the wrong tool for a different exam and refusing to admit it.
Let me walk you through the landmines so you don’t join the “I underperformed Step 3 and now my confidence is shot” club.
The Core Mistake: Treating Step 3 Like Step 2 CK 2.0
Step 3 is not “Step 2 CK but longer.” It’s a different beast. Different emphasis. Different skill set. And it punishes people who show up with only Step 2 habits.
On Step 2 CK:
- You live in diagnosis and initial management.
- You can get away with algorithm-memorizing if your recall is sharp.
- You’re rarely forced to “own” a patient for multiple steps.
On Step 3:
- The exam wants to know if you can act like an unsupervised physician.
- It cares a lot more about sequencing decisions over time, not just “what’s the next best test right now.”
- It throws CCS cases at you where knowledge is necessary but absolutely not sufficient.
If your Step 3 prep strategy is:
- Re-reading old Step 2 notes
- Repeating old Anki decks
- Doing questions and calling that “good enough”
You’re setting yourself up to:
- Miss clinical nuance
- Mismanage time
- Panic on CCS
- Bleed points on preventable, pattern-based errors
That’s not “bad luck.” That’s a predictable consequence of over-relying on Step 2 CK notes as your foundation.
Why Your Step 2 CK Notes Quietly Fail You on Step 3

| Category | Re-reading old notes | Step 3-style Qbank + review | [CCS practice](https://residencyadvisor.com/resources/usmle-step3-prep/common-ccs-practice-mistakes-that-create-false-confidence) | Guideline refresh (USPSTF/ACLS/etc.) |
|---|---|---|---|---|
| Over-Reliant on Step 2 Notes | 60 | 25 | 5 | 10 |
| Balanced Step 3 Prep | 20 | 40 | 25 | 15 |
Let’s be blunt: your Step 2 CK notes were written for a different question style, different blueprint, and a different version of you.
1. They’re Biased Toward “What,” Not “When” and “How Long”
Most Step 2 notes are:
- Disease summaries
- Work-up checklists
- One-liner “next best step” pearls
Step 3 punishes you for not understanding:
- Timing (when to repeat labs, when to escalate, when to de-escalate)
- Duration (how long you treat, how long you observe, how long you anticoagulate)
- Follow-up strategy (who you admit vs discharge vs refer)
On CCS:
- It’s not enough to know what to order.
- You must know:
- Order now vs later
- ICU vs floor vs outpatient
- Once vs daily vs PRN
- When to stop what you started
Your Step 2 notes probably say:
- “NSTEMI → MONA, beta-blocker, heparin, statin, PCI.”
Step 3 wants:
- “How do you actually sequence and monitor this patient over hours to days, and what do you do when they improve vs deteriorate?”
If your notes don’t reflect time-course thinking, they’re Step 3-weak.
2. They’re Outdated or Misaligned With Step 3 Priorities
I’ve seen people studying off Step 2 notes that:
- Still emphasize older, now low-yield antibiotic choices
- Underplay outpatient chronic disease management
- Barely mention preventive care and screening guideline nuances
Step 3 leans harder into:
- Longitudinal management of diabetes, HTN, CHF, CKD
- Preventive care: vaccines, screening ages, follow-up intervals
- Risk/benefit decision-making in “grey zone” situations
Step 2 notes that were laser-optimized for immediate exam-day recall can be:
- Too detailed in weird pathology
- Too shallow in management nuance
- Completely CCS-useless
You’re not just reusing notes. You’re reusing a blueprint for a different exam.
3. They Encourage Memorization Over Clinical Reasoning
Another trap:
Students fall in love with their Step 2 notes because they represent thousands of pages of “work done.”
The sunk cost is massive.
So instead of upgrading their thinking, they double down on re-reading.
That leads to:
- Recognition-based studying (“oh yeah, I remember this page”)
- Overconfidence without true flexibility
- Very fragile performance when questions shift context or format
Step 3 questions often:
- Stretch the scenario over multiple visits
- Give partial improvement or partial failure to treatment
- Force you to choose between safe vs aggressive vs cheap strategies
No static note set is going to train that properly. That comes from doing Step 3-style questions and especially CCS cases. Not from bathing in old Step 2 PDFs.
The Cost: How This Sabotages Scores in Predictable Ways

When people over-rely on Step 2 notes, their Step 3 score report tends to show the same pattern of damage.
1. CCS Disasters – The Silent Score Killer
This is the most obvious casualty.
People who lived in Step 2 world:
- Underestimate CCS completely
- “Plan” to cram CCS in the last week
- Maybe run 5–10 practice cases at best
Then on test day:
- They freeze on timing
- Forget key orders
- Fail to monitor basic parameters
- Discharge too early or never discharge at all
Classic consequences:
- Missing DVT prophylaxis
- Forgetting pain control or bowel regimen
- Skipping basic labs in a “too narrow” workup
- Not doing counseling or follow-up
- Forgetting to physically move the patient (ICU → floor → home)
These errors are rarely about missing the disease.
They’re about never having practiced managing a living timeline. Step 2 notes have almost no muscle in that area.
2. Over-Testing and Over-Treating
Step 2 success can accidentally train you to:
- Reflexively “click all tests that sound relevant”
- Escalate aggressively because that was often the right board answer
Step 3 punishes:
- Unnecessary imaging and labs
- Overuse of broad antibiotics
- Dangerous polypharmacy in frail or elderly patients
- Ignoring cost-effective and safer options
This is where people with massive Step 2 fact banks still miss:
- You know the rare disease cold.
- But you fail basic risk stratification and resource-use judgment.
That’s a Step 3 problem. Step 2 notes do not fix it.
3. Weak Outpatient and Preventive Care
Step 2 exams and rotations often bias your brain toward:
- Inpatient
- Acute
- “Save the day” medicine
Step 3 leans hard into:
- USPSTF preventive care
- Chronic management
- Monitoring intervals
- Long-term risk reduction
If your notes don’t:
- Drill screening ages, intervals, and when to stop screening
- Clarify step-ups and step-downs in outpatient regimens
- Highlight age/sex/pregnancy-specific management differences
You’ll:
- Underperform in ambulatory medicine
- Miss “soft” but high-yield scoring opportunities
- Walk out thinking the test was “weirdly outpatient-heavy” (it wasn’t; you just trained inpatient-heavy)
Signs You’re Over-Relying on Step 2 CK Notes (Red Flags)
Let’s be concrete. If you see yourself in most of these, you’re making this mistake.
| Red Flag | Why It’s a Problem |
|---|---|
| 70%+ of study time is re-reading old notes | Low-yield repetition, no Step 3 skill-building |
| CCS practice scheduled only in last 1–2 weeks | Not enough time to fix pattern-level errors |
| No dedicated resource for Step 3-specific content | You’re assuming content overlap = exam overlap |
| You feel “comfortable” because Step 2 was high | Overconfidence keeps you from upgrading strategy |
| You haven't looked at updated guidelines | Outdated management choices on a management-heavy exam |
If your “plan” looks like:
- “I’ll do UW once + CCS cases in the last week + skim my Step 2 stuff”
You don’t have a plan. You have wishful thinking wrapped in nostalgia.
How to Use Step 2 Notes Without Letting Them Wreck Your Step 3
I’m not saying burn your Step 2 CK notes. I’m saying stop pretending they’re something they’re not.
Here’s how to use them correctly.
1. Use Step 2 Notes Only as a Quick Patch, Not a Primary Tool
Healthy uses:
- Brief brush-up on weak topics you keep missing in Qbank (e.g., glomerulonephritis types, vasculitides)
- Fast reference for pathophys you haven’t seen since third year
- Targeted review of high-yield micro/pharm gaps
Unhealthy uses:
- Systematically re-reading every page
- Spending hours “organizing” or “updating” your old notes instead of doing questions
- Using notes to avoid facing your current performance data
If you’re going to open those notes:
- Make it problem-driven: “I keep missing SIADH vs CSW cases—let me look just at that.”
- Set a hard time cap per session (e.g., 30–45 minutes).
2. Build a Separate, Lean Step 3 Management & CCS Toolkit
You need a Step 3-specific spine. That means:
- One main Qbank that’s actually written for Step 3
- One solid CCS practice platform (not just glancing at sample cases)
- A short, focused document or resource that emphasizes:
- Preventive care
- Outpatient management
- Common inpatient longitudinal care
Think of it this way:
- Step 2 notes = background knowledge reservoir
- Step 3 toolkit = execution manual
If your “execution” resource is just “I’ll kind of think through it on test day,” you’re gambling with your score.
3. Translate Knowledge Into Orders, Timelines, and Follow-Up
Whenever you review a topic now, ask:
- What orders would I place on CCS?
- What’s day 0 vs day 1 vs discharge planning?
- What needs:
- Monitoring
- Adjustment
- Explicit stop dates
- Specific counseling
Example: Pyelonephritis in pregnancy
Step 2 notes:
- “IV ceftriaxone, hospitalize, switch to oral after afebrile 48h, treat 10–14 days.”
Step 3 mindset:
- Admit vs outpatient?
- What specific labs on admission?
- Fetal monitoring?
- Follow-up urine culture after completion?
- Future prophylaxis?
Same disease. Different level of thinking.
Train the Step 3 level.
A Practical Structure That Doesn’t Let Notes Hijack Your Prep

| Step | Description |
|---|---|
| Step 1 | Start Step 3 Prep |
| Step 2 | Baseline Qbank Block |
| Step 3 | Targeted Step 3 Resource Review |
| Step 4 | CCS Case Practice |
| Step 5 | Brief Look at Old Step 2 Notes |
| Step 6 | Move On to Next Block |
| Step 7 | Identify Weak Areas |
| Step 8 | Still Missing Same Topics? |
Notice:
- Old notes come in late in the loop.
- They support, not define, your studying.
Here’s a more concrete weekly structure to avoid the trap:
- 60–70%
- Step 3-style Qbank blocks + detailed review
- 20–25%
- CCS practice (interactive cases, not just reading scripts)
- 10–15%
- Guideline & outpatient management refresh
- Optional 5–10%
- Tightly targeted Step 2 note consultation when Qbank reveals a true gap
If the pie chart of your study time is flipped—mostly Step 2 notes, little CCS—you’re building a predictable score problem.
Common Rationalizations That Will Burn You

| Category | Value |
|---|---|
| Rely on Step 2 notes | 70 |
| Delay CCS practice | 65 |
| Skip guideline refresh | 55 |
| No dedicated schedule | 60 |
You’ll hear these in group chats and resident lounges all the time:
“Step 3 is just a formality. Programs don’t really care about the score.”
- Reality: Some boards, state licenses, and fellowships do care. And a bad score tanks your self-confidence right when you’re stepping into real responsibility.
“I did great on Step 2—I’ll be fine.”
- Reality: Different test type, different emphasis. I’ve watched multiple 250+ Step 2 students scrape by with mediocre Step 3 results because they coasted.
“I’ll learn CCS the week before.”
- Translation: “I’m afraid to open CCS and find out how bad I am right now.”
“There isn’t that much new content.”
- Maybe. But there’s a new skill set. And that’s where people lose points.
If you catch yourself saying these, that’s your warning siren.
FAQ (4 Questions)
1. I scored high on Step 2 CK. Do I really need to change my approach for Step 3?
Yes. High Step 2 shows you have the knowledge. Step 3 tests whether you can deploy that knowledge in multi-step, time-based, unsupervised scenarios—especially CCS and outpatient management. You don’t need to panic or do an insane overhaul, but you cannot just hit replay on your Step 2 method and expect a similar performance without explicitly training CCS and long-term management.
2. Should I re-do all my Step 2 Anki cards for Step 3?
No. That’s overkill and a poor use of limited time. At best, selectively unsuspend cards in topics you’re actively missing in your Step 3 Qbank (e.g., a cluster of endocrine or rheum mistakes). But if you’re grinding through thousands of old Step 2 cards out of habit or guilt, you’re crowding out time needed for CCS, Qbank analysis, and guideline-tuned thinking.
3. How many CCS cases should I do to avoid getting burned?
More than “a handful.” Aim to complete enough cases to see a wide range of core scenarios—sepsis, chest pain, OB, peds fever, trauma, psych, acute abdomen, etc.—and repeat until your process is smooth: initial stabilization, diagnostic workup, location of care, ongoing monitoring, and discharge planning. You don’t need to do every single case on a platform, but you must do enough that your approach becomes automatic, not improvised.
4. If I’m short on time, what should I cut: Qbank, CCS, or re-reading notes?
Cut re-reading notes first. Then trim overly detailed guideline or textbook reading. Keep:
- Regular Step 3-style Qbank blocks with focused review
- Consistent CCS practice, even if it’s just 1–2 cases per day
Those two are non-negotiable. Notes are supplemental. If you’re spending hours in old Step 2 documents instead of doing active practice, you’re choosing comfort over performance.
Key takeaways:
- Step 3 is not Step 2 CK with more questions. It’s a management and CCS-heavy exam that punishes timeline and follow-up errors your Step 2 notes barely address.
- Old Step 2 CK notes are a supporting tool, not your core resource. Use them surgically for gaps, not as your main study method.
- Protect your score by prioritizing Step 3-style Qbank, CCS practice, and updated management/preventive care—then, and only then, let Step 2 notes fill in the cracks.






















