Attendings do not push you to finish Step 3 early because they “care about your long‑term learning.” They push you because of scheduling, money, and risk. For them. Not for you.
Let me walk you through what actually gets said in closed‑door meetings and faculty chats, because students almost never hear this part.
What Attendings Say vs What They Mean
On the wards you hear the same script over and over:
- “Get Step 3 out of the way early.”
- “You’ll thank yourself later.”
- “Programs really like when you’re done by intern year.”
Sounds supportive. Looks like mentorship.
Now let me translate.
When an attending tells you, “You really should take Step 3 before PGY‑2,” what they’re usually thinking is some version of:
- “Our program had a near‑miss with a Step 3 failure and it screwed up our schedule for months.”
- “My chief had to redo the entire call grid because one PGY‑2 couldn’t get a full license.”
- “The GME office chewed us out last year about low Step 3 completion rates.”
So yes, the pressure is “for your own good,” but the real driver is that a delayed or failed Step 3 makes life harder for the program and the faculty. And faculty remember pain.
They do not want to live through that again.
The Ugly Administrative Side You Never See
Here’s what you are not in the room for: the GME and clinical leadership meetings where your name is a line item on a problem list.
I’ve sat in rooms where the agenda literally had:
- “Step 3 completion – PGY1 IM residents”
- “Licensing delays – impact on RVUs”
Nobody on that call is talking about your wellness. They’re talking about coverage, FTEs, and billing.
Here’s how it actually works behind the curtain.
Step 3 and licensing: follow the money
Hospitals want you fully licensed as early as possible because once you are:
- You can bill as an independent provider in some settings.
- You can take more responsibility without an attending constantly co‑signing.
- You look better on paper for accreditation metrics.
Until you pass Step 3, you’re capped. Functionally and financially.
Most states require Step 3 for an unrestricted license. Programs don’t want you stuck on a “training license” longer than necessary because:
- It complicates moonlighting.
- It complicates credentialing at affiliated hospitals.
- It limits what they can have you do in clinic.
So when an attending tells you, “You’ll have more flexibility once Step 3 is done,” the unspoken part is: “I can staff clinics and call more easily if all of you are fully licensed.”
They’re not lying. They’re just leaving out the part where your exam score is now part of their operations problem.

| Category | Value |
|---|---|
| Scheduling/Coverage | 90 |
| Licensing/Billing | 80 |
| Accreditation Metrics | 60 |
| Resident Wellness | 25 |
The Risk No One Wants to Talk About: Step 3 Failure Fallout
The whispered fear in every program: “What if one of our residents fails Step 3? Or worse, fails twice?”
I’ve watched that happen from the program side. It’s ugly.
Here’s the chain reaction when a resident fails Step 3 late:
- Their unrestricted license is delayed or denied.
- Moonlighting plans? Gone.
- Certain rotations (especially at outside hospitals that require full licensure) suddenly become impossible.
- Program has to swap residents, rebuild schedules, beg favors from other services.
- GME starts asking the PD what the heck is going on with Step 3 pass rates.
That last part matters. A lot.
Program Directors get evaluated on:
- Board pass rates
- Step 3 completion timelines
- “Remediation events”
When someone fails Step 3:
- The PD has to write formal documentation.
- They may need to report it to GMEC.
- It potentially affects future accreditation reviews.
So the PD goes back to the faculty and chiefs and says, “We are not doing this again. Push them harder to get Step 3 done early, before life gets too complicated and they’re distracted.”
And then that trickles down to you as, “Hey, you should just knock Step 3 out early, it’s easier.”
The message has been sanitized. The urgency is not.
Why Early Step 3 Actually Does Help You (When Done Right)
I’m not going to pretend there isn’t a selfish institutional motive. There is. But here’s the twist: this is one of the few things where their selfish needs actually line up with your best interests—if you’re smart about it.
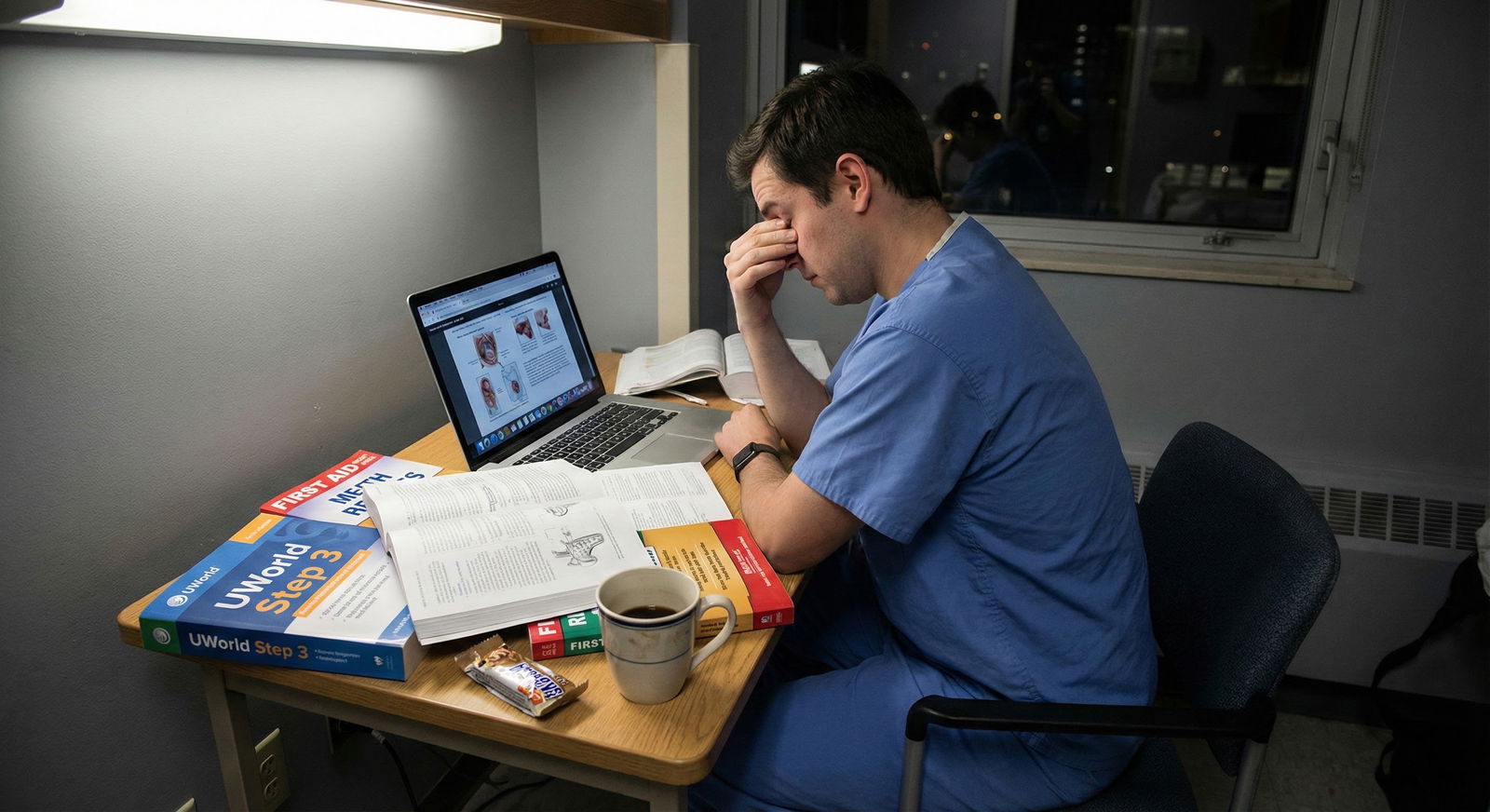
You’ve seen the residents taking Step 3 in PGY‑3 who are:
- Exhausted
- Chief or fellowship‑applicant level busy
- Trying to review CCS cases between pager alerts
They always say the same thing: “I should have just taken this intern year.”
They’re not wrong.
Early Step 3 is ideal for you when:
- Your clinical brain is fresh.
- You’re still in “exam mode” from Step 2.
- You haven’t yet taken on big leadership roles or heavy outside responsibilities.
- You’re not burned out to the point that you resent every UWorld question.
But there’s a line.
Too early, and you walk into the exam underprepared, especially for CCS. Too late, and you’re trying to learn from scratch with adult responsibilities stacked on top of you.
Most attendings who push “early” actually mean “PGY‑1 or very early PGY‑2, once you’ve seen enough real medicine to not be a walking question bank parrot.”
They’re right about that timing. They’re just terrible at explaining why.
How Programs Quietly Track You
Residents think nobody’s watching their Step 3 prep. That’s cute.
Behind the scenes, here’s what I’ve seen more than once:
- A spreadsheet with each resident’s Step 3 status: “Not scheduled / Scheduled / Passed”
- Emails from GME: “We expect 80% of your PGY‑1s to have Step 3 done before starting PGY‑2 year.”
- Chiefs getting pulled aside: “You need to remind your class. Too many people delaying Step 3.”
Your name gets mentioned when:
- You’re one of the last in your class who hasn’t scheduled.
- You failed once and have not yet re‑scheduled.
- You’re in a “borderline” performance category already (struggling on in‑service exams, performance concerns).
Nobody writes this in your formal evaluation as “red flag: delayed Step 3.” But people remember the residents who were constant admin headaches. The ones they had to chase for paperwork and licensing and exams.
Those are the same faculty who will be writing your letters later. That “soft” memory matters more than you think.

| Step | Description |
|---|---|
| Step 1 | Start PGY-1 |
| Step 2 | Program relieved |
| Step 3 | Monitoring but ok |
| Step 4 | Chiefs + PD start asking |
| Step 5 | Close file, move on |
| Step 6 | Schedule disruption, remediation, GME attention |
| Step 7 | Scheduled Step 3? |
| Step 8 | Fails Step 3? |
The Script Attendings Use – And What You Should Hear
Pay attention to the exact wording your attendings use. You’ll start to hear the subtext.
When an attending says:
“You don’t want this hanging over your head.”
They mean both: your mental load and their scheduling headache if you push this into late PGY‑2.
“Program Directors like seeing Step 3 done early.”
They’re really saying: PDs fear people who procrastinate high‑stakes requirements. It signals risk. Risk of failing, risk of licensing delays, risk of future paperwork.
“Trust me, life doesn’t get easier later.”
They’re right. But they’re also remembering the PGY‑3 who was supposed to be chief, failed Step 3, had their license delayed, and suddenly became a problem instead of an asset.
You need to hear both.
The One Group That Gets Screwed by “Take It Early” Advice
Here’s the part most attendings never think through: their Step 3 pep talk isn’t tailored to you. It’s generic.
The resident who barely passed Step 2 on the second try? The IMG who’s never seen a CCS case format? The person who just had a massive personal crisis? They do not need “take it early.” They need “pass on the first attempt, whenever that is.”
A failed Step 3 is a much bigger problem than a delayed Step 3.
From the program’s standpoint, both are annoying. From your standpoint, failure sticks to you forever.
So you have to be blunt with yourself:
- If you crushed Step 2 and you’re clinically solid: early Step 3 is usually smart and safe.
- If your Step 2 score is marginal, you’ve struggled with clinical reasoning, or you barely passed in‑training exams: you do not rush Step 3 just to make your PD happy.
You give yourself enough runway to pass. First attempt. No drama.
How to Time Step 3 So It Works For You And Them
Let’s get specific. This is what attendings and PDs actually want, even if they never say it this clearly:
- Most IM, peds, EM, FM programs: Step 3 done by the end of PGY‑1 or very early PGY‑2.
- Some surgical specialties: a bit more flexibility, but still before PGY‑3 if possible.
- Transitional/prelim years: they really want you to have a plan, because your next program will absolutely care.
The sweet spot for most residents is:
- 6–12 months after starting residency.
- After you’ve done at least a couple of core rotations (wards, ICU, or ED).
- Before you’re on nights for months straight or taking on heavy leadership roles.
Here’s what that looks like in reality:
| Timing Choice | What Residents Think | What Actually Happens |
|---|---|---|
| Late MS4 / pre‑residency | “I’ll be free as an intern.” | Many underprepare, CCS is weak, risk of failure. |
| Early PGY‑1 (first 3 mo) | “I’ll get it over with immediately.” | Overwhelmed by transition, poor depth of knowledge |
| Mid PGY‑1 (months 4–8) | “Good balance of experience/time.” | Usually optimal if you’re reasonably prepared. |
| Late PGY‑1 / early PGY‑2 | “I’ll do it when rotations are lighter.” | Fine if you actually commit; programs start nudging. |
| Late PGY‑2 / PGY‑3 | “I keep putting it off.” | Max stress; programs anxious; higher burnout risk. |
If you want to keep both your future and your PD happy, you aim for that mid‑PGY‑1 to early PGY‑2 window, but only if your foundation and mental bandwidth are there.
What Attendings Wish You Understood About Step 3
Here’s the candid version I’ve heard in faculty rooms:
- “Step 3 is not a brilliance exam. It’s a responsibility exam.”
- “If they can’t pass Step 3, I worry about them managing real patients independently.”
- “I don’t want someone applying for hospital privileges with two Step 3 fails on their record and my name on their letters.”
Once you see it that way, their obsession makes a bit more sense. By pushing you early, they’re trying to limit the scenario where:
- You’re late in training
- You fail Step 3
- Someone has to seriously question your progression or even your graduation
Programs hate remediation for senior residents. It’s politically messy and emotionally brutal.
So yes, they want you coded as “Step 3: passed” as soon as reasonably possible, to remove a landmine from their future.
How To Use Their Pressure Without Letting It Wreck You
You cannot change the fact that your attendings, chiefs, and PD care a lot about your Step 3 timing. That’s baked into the system.
What you can do is use that pressure strategically instead of letting it drag you into a dumb decision.
Here’s how the smart residents I’ve seen do it:
They treat “take Step 3 early” as a nudge, not a command.
They:
- Pick a realistic window (usually mid PGY‑1 to early PGY‑2).
- Back‑plan 8–10 weeks of steady, not insane, studying.
- Tell their PD or chief, “I’m scheduled for [month]. I’ve started UWorld. I’ll be done before PGY‑2.”
- Then actually follow through.
Notice what that does:
- It reassures the program. They stop chasing you.
- It frees you from constant Step 3 nagging.
- It gives you structure without rushing you into a death‑march.
And if you’re not ready?
You say something most residents are afraid to say:
“I had some trouble on Step 2 and I’m making sure I pass Step 3 on the first attempt. I’ve already started studying and will schedule for [slightly later but concrete date].”
Programs would rather hear a sane, honest plan than watch you spin your wheels and fail.
Step 3 Myths Attendings Accidentally Spread
Let me clear up a few lies that get repeated so often they sound like fact:
- “Programs don’t care about your actual Step 3 score, only pass/fail.”
Mostly true, but incomplete. For fellowships, some PDs absolutely look at Step 3 scores, especially in competitive fields. And multiple attempts matter more than the number itself.
- “You can wing Step 3 because it’s easier than Step 2.”
Dangerous. Yes, the pass rate is higher. But the people taking it are residents, not random applicants. The denominator is stronger. Plenty of bright residents underestimate CCS and get burned.
- “You’ll never use this stuff in real life.”
Nonsense. Step 3 is directly tied to real outpatient and inpatient decision making: chronic disease management, triage, next‑best step, safe dispo decisions. It’s not abstract like Step 1 was.
- “Everyone at this program takes it intern year.”
Flat‑out false at many places. What they mean is: “We prefer you do it intern year.” There are always outliers. They just like to pretend those people are mythical creatures.
The Bottom Line: Their Agenda vs Your Agenda
Strip away the nice language and here’s the core truth:
- Their agenda: get you to pass Step 3 as early as safely possible so you’re licensed, fully functional, and not a ticking accreditation or scheduling problem.
- Your agenda: pass Step 3 on the first try, at a time that doesn’t destroy your sanity or undermine your performance.
Those two goals overlap more than they conflict. But in any fight between “early” and “safe,” you prioritize safe.
Do not fail this exam to make someone happy about a timeline.
The smartest move is to:
- Acknowledge the pressure.
- Understand the real reasons behind it.
- Choose a timeline that serves your long‑term career, not just this year’s call schedule.
Use their urgency as momentum. Not as your master.
FAQ
1. Is taking Step 3 during MS4 actually a good idea?
Usually not. I’ve seen a handful of rock‑stars pull it off, but most MS4s don’t have enough clinical seasoning or CCS familiarity to do this safely. You’re also juggling interviews, sub‑Is, and the emotional fatigue of the Match. If your Step 2 was extremely strong and you’re still very much in exam mode, maybe. But for the average student, it’s an unnecessary risk.
2. How much does a failed Step 3 attempt really hurt me long‑term?
It hurts more than people admit. One failure isn’t automatically career‑ending, but it does raise questions for future PDs and credentialing committees. They’ll look at the pattern: prior scores, in‑service exams, clinical performance. What you absolutely want to avoid is multiple failures. That’s when people start quietly saying, “Is this person safe to practice independently?” Fair or not, that’s the reality.
3. What’s a realistic study timeline if I take Step 3 mid‑PGY‑1?
For most residents: 6–10 weeks of consistent, not insane, study is enough. That looks like 1–2 hours most weekdays, a bit more on one weekend day, with focused UWorld, CCS practice, and quick review of weak systems. You’re not re‑learning medicine from scratch; you’re organizing and sharpening what you use every day. The mistake people make is doing three weeks of nothing and then trying to brute‑force 10 days straight. That’s how you burn out and forget half of what you crammed.
4. What should I say if my attending keeps pushing me to schedule and I’m genuinely not ready?
Be direct but structured. Something like: “I really appreciate the push. I didn’t perform as well as I wanted on Step 2, so I’m being careful to make sure I pass Step 3 on the first attempt. I’ve already started UWorld and plan to test in [month].” That tells them you’re not avoidant; you’re strategic. Most reasonable attendings back off once they hear a clear, time‑bound plan. The ones who don’t are thinking only about their schedule, not your career—take their pressure with a grain of salt.






















