The timing of your Step 3 is not neutral. Program directors read it like a personality test you did not realize you were taking.
Let me tell you what really happens behind those closed-door rank meetings and CCC (Clinical Competency Committee) reviews when your file pops up and someone says: “By the way, when did they take Step 3?”
Why Step 3 Timing Matters More Than Anyone Tells You
Faculty love to pretend Step 3 is just a formality. “You’ll pass, don’t stress, just get it done sometime intern year.” That’s the public line.
Behind the scenes, your Step 3 timing is treated as a crude but surprisingly useful signal of three things:
- How you plan and prioritize under pressure
- How much risk you create for the program
- How serious you are about fellowship or future mobility
No one’s announcing this on the residency website. But I’ve watched PDs in IM, surgery, EM, and peds comment on Step 3 timing with a tone that told me it absolutely influenced their judgment.
Does it usually make or break your career? No.
Does it tilt marginal decisions and color how they interpret everything else about you? Absolutely.
To understand how they read you, you need to know what each common timing pattern whispers (or screams) to a program director.
The Hidden Calculus: What PDs Actually Worry About
Before we dissect timing patterns, understand the frame of mind of a PD looking at Step 3.
They’re not thinking: “Is this resident smart?”
They’re thinking: “Is this resident going to blow up my life at the worst possible time?”
A resident failing Step 3 is not just “bummer, they’ll retake it.”
It’s:
- Credentialing delayed or blocked
- Moonlighting shut down (money, coverage holes)
- Visa and licensing complications
- Extra remediation time
- Potential gap in coverage if you have to be pulled from rotations
You are not a student anymore. You are workforce. Anything that threatens that workforce is a problem.

| Category | Value |
|---|---|
| Licensing Delays | 80 |
| Visa/Credentialing Risk | 60 |
| Extra Faculty Time | 70 |
| Schedule Disruption | 65 |
| Bad Board Pass Stats | 50 |
So when programs look at timing, they’re reading it through that lens:
Is this person someone who creates problems or solves them early?
The Classic Patterns: What Your Timing Says About You
Let’s go through the main Step 3 timing strategies I see and what PDs quietly infer from each.
1. Early Bird: Step 3 Before Residency or Very Early PGY-1
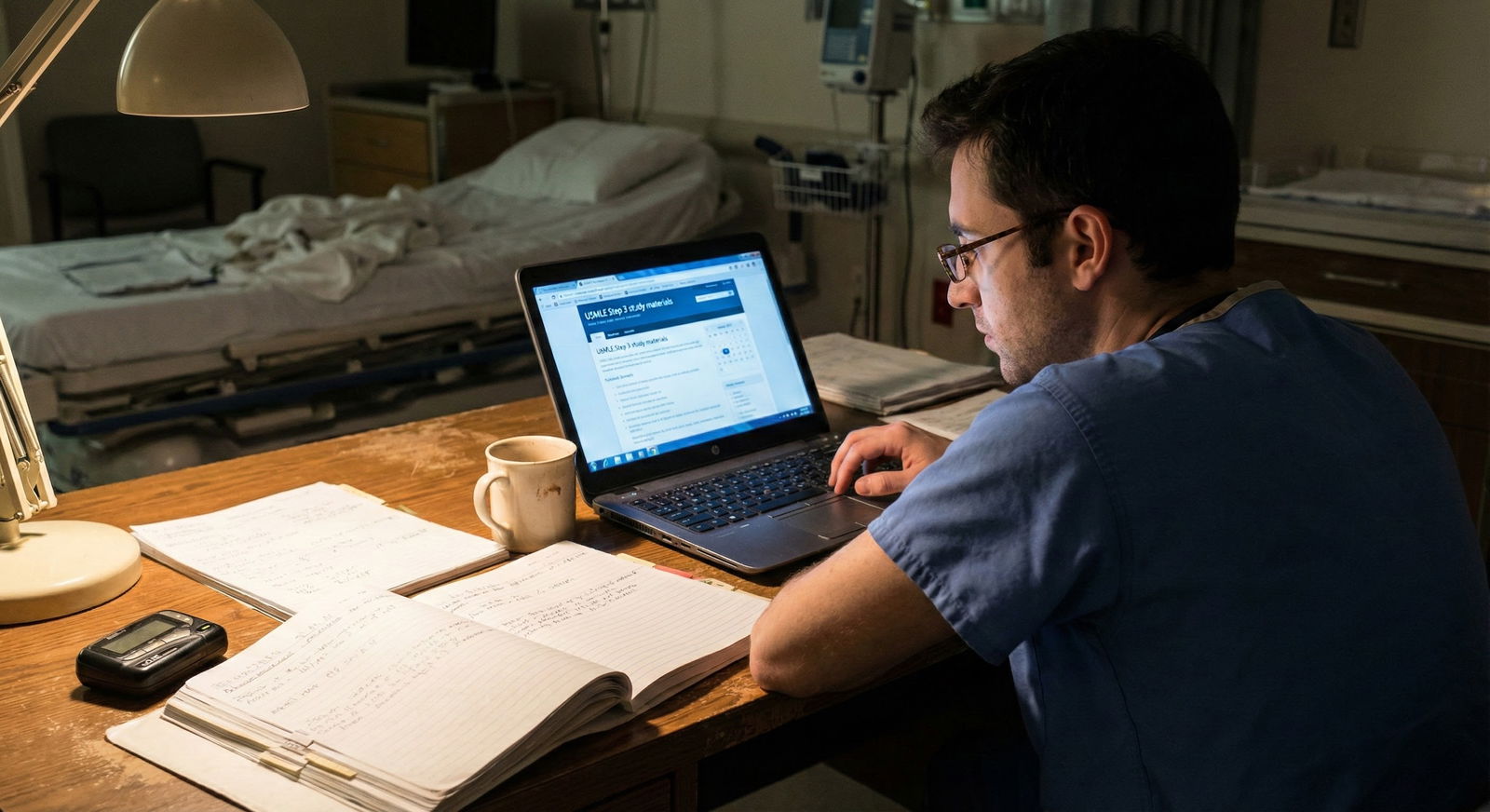
This is the med student who takes Step 3 during 4th year or first few months of intern year, often before most peers have even opened a Qbank.
What PDs often infer:
“This person is a planner.”
They see someone who thinks ahead, wants things off their plate, and understands that future flexibility is power. Especially true if your Step 1/2 trajectory was strong.“They’re low administrative risk.”
Having Step 3 done when you start or very early means the program never has to schedule around it, negotiate coverage, or worry about deadlines for state boards or fellowship applications.“Are they running away from clinical responsibility?” (this one’s quieter)
If you pushed hard to take Step 3 in the first 1–2 months of internship and demanded lighter schedules, some attendings will see that as “test first, patients later.” It depends heavily on how you performed clinically during that time.
If you scored solidly or well on Step 3 with early timing, this tends to land as a net positive. They see you as organized, and for fellowship-heavy fields (GI, cards, heme/onc, pulm/crit), it’s a strong subtle signal of ambition and planning.
When it backfires:
- You took it way too early, bombed it, or barely passed, after stellar Step 1/2.
Now the conversation is: “Why did they rush this? Judgment problem.” - You’re an IMG who clearly crammed it in just to meet visa/eligibility timelines, then scraped a low pass. That raises both risk and stamina concerns.
2. Standard Planner: Late MS4 or Mid–Late PGY-1
This is the resident who uses late 4th year or a manageable part of intern year (elective, lighter block) to knock out Step 3.
This is the most comfortable pattern for PDs.
What they infer:
“They understand timing and bandwidth.”
Someone who waited until they had enough clinical exposure to not drown, but did not wait so long that Step 3 became a fire to put out.“They respect program needs.”
If you schedule Step 3 during a lighter rotation and handle your responsibilities without dumping on your co-residents, senior residents notice. And senior residents talk to the PD.“They’re likely to be fine for any state licensure/fellowship.”
Most competitive fellowships want Step 3 done by the time applications go in (summer of PGY-2 for IM, for example). Doing it in this window shows you understand the timeline.
In rank meetings, this timing rarely even gets mentioned—because it’s the default “no drama” choice.
3. Late and Sweaty: End of PGY-1 or Squeezed into Early PGY-2
This is where the whispers start.
You waited and waited, then suddenly you’re begging for two days off on a heavy rotation, trying to cram UWorld between night floats, and everyone can feel the panic.
What PDs infer:
“They procrastinate under pressure.”
They know every resident is overloaded. The ones who still carve out time to schedule Step 3 in a rational window send one message. The ones punting to the last minute send another.“We might get a licensing headache.”
For IM, EM, psych, peds, etc., many states expect Step 3 passed by a certain point for full licensure. If you’re cutting it close, PDs start thinking about credentialing delays, inability to moonlight, or blocked future contracts.“Will this be how they handle fellowship applications, QI projects, research?”
PDs love pattern recognition. If you push Step 3 to the edge, they assume you’ll push other deadlines too.
There’s a difference, though, between “late but fine” and “late and chaotic.”
If you took it late but passed comfortably and your evaluations are glowing, programs usually shrug and move on.
If you took it late, barely passed, and you already have borderline evaluations? That combination is what worries them.
The Red Flag Zone: Very Late or Repeated Failures
Let’s be blunt. The deepest conversations about Step 3 happen around delays plus problems, not delays alone.
Here’s where PDs really start dissecting you.
Very Late Timing: Mid–Late PGY-2 or Beyond (Without a Clear Reason)
If you show up on a PD’s radar as PGY-2 and still haven’t sat for Step 3 — and there’s no pregnancy, medical leave, transfer, or visa complication — here’s what they start saying in meetings:
“Why are we still dealing with this?”
Administrative frustration. Because now they’re fighting with rotation schedules, fellowship timelines, and sometimes the GME office.“Are we going to be able to promote them?”
In some institutions, promotion and renewal decisions get tied to Step 3 progress. If you’re running way behind, your name now shows up on lists PDs get from GME—never a good thing.“What happens if they fail now?”
If you fail Step 3 late, the program has very little runway to fix the mess. That’s the scenario that keeps them up at night.
Failing Step 3: What They Really Think
Most residents think a Step 3 fail is a massive scarlet letter. It is serious, but the narrative they attach to it depends heavily on the context.

Here’s the real calculus:
If you had:
- Strong Step 1/2
- Good in-training exam performance
- Consistently solid evaluations
and then you failed Step 3 once, early, and then passed solidly on a retake?
The read is usually: “Bad timing, bad test day, maybe life stress. But they corrected it.” The concern fades—especially if you handled the remediation like an adult and did not play the victim.
But if you had:
- Marginal Step 1/2
- Borderline in-training scores
- Hesitant or weak clinical performance
- Delayed Step 3
- Then failed it
Now the story becomes brutally simple in the room: “This is not a fluke. This is who they are.” And they start talking about remediation plans, whether you’ll be able to pass boards, and how much risk you are to program board pass stats.
Yes, programs care about their board pass rates. A lot more than they’ll admit to your face.

| Category | Value |
|---|---|
| Isolated Event (Strong Record) | 20 |
| Mild Concern (Mixed Record) | 35 |
| Serious Risk (Weak Record) | 45 |
So it’s not “fail = death.” It’s “fail + timing + pattern = story.”
Special Case: IMGs and Step 3 Timing
For IMGs, Step 3 timing isn’t just a preference. It’s sometimes a survival requirement.
PDs look at your Step 3 timing differently if:
- You needed it for visa reasons
- You used it to strengthen a weak Step 1/2 for residency apps
- You took it pre-residency to look more competitive
If you’re an IMG who knocked out Step 3 before residency with a strong score, that’s often seen as a big plus:
- Shows stamina and commitment
- Reduces future visa/licensure administrative complexity
- Reassures them you can clear the final standardized test hurdle
Where IMGs get into trouble:
- Taking Step 3 very early, scoring barely above passing, after marginal Step 1/2
Now you’ve confirmed a negative pattern instead of disproving it. - Delaying Step 3 despite visa or licensing pressure, then barely passing or failing late
That’s when PDs start questioning not just your knowledge, but your insight and planning skills.
Fellowship-Bound vs Generalist: Different Interpretations
You cannot understand Step 3 timing without factoring in your long-game.
If You’re Fellowship-Bound
Cards, GI, heme/onc, pulm/crit, allergy, rheum, ICU, EM fellowships — these PDs notice Step 3 timing more than the average community hospital.
Why?
- They want to avoid anyone still wrestling with exams when fellowship boards roll around.
- They want evidence that you can manage multiple timelines: residency duties, research, applications, exams.
Taking Step 3 in a clean, earlier window (late MS4 or early–mid PGY-1) sends a strong message:
“I clear hurdles early so they’re not in the way when the stakes are higher.”
I’ve literally heard a cardiology PD say:
“If you’re applying to me without Step 3 done, it’s not a hard cut, but it’s a different file. Shows me you’re either disorganized or over your head.”
If You’re Likely to Be a Hospitalist or Outpatient Generalist
Community programs and hospitalist-heavy institutions care more pragmatically:
- Can you be fully licensed on time?
- Will your delay/failure block them from hiring you or renewing you?
- Will you be able to moonlight to fill service gaps?
They don’t need early Step 3 for prestige reasons. They need it out of the way so you can function as independently as possible by the time you’re a senior.
But even here: the resident who quietly took Step 3 during a lower-stress rotation and passed comfortably is always a more attractive future hire than the one who barely scraped through on the third try in PGY-3.
What PDs Notice Beyond the Date: Context and Behavior
They don’t just look at when. They look at how you handled it.
Here are the pieces they actually discuss in closed meetings:
Did you schedule Step 3 responsibly or dump call coverage on others?
Residents who constantly swap out of hard shifts “because of Step 3” but are mysteriously free for weekends off create enemies. Those enemies talk.Did you communicate early and professionally?
The resident who emails the chief/residency coordinator months in advance: “I’d like to take Step 3 during X rotation; can we coordinate?” reads very differently from the one who says two weeks before: “I need two days off, sorry.”What were you like on the rotation when you studied?
You can absolutely study on an easier elective and still be a strong team member. Or you can disappear and become “that resident who doesn’t help because they’re always ‘studying.’”How did you frame any setbacks?
If you failed, and your narrative is always: “The test was unfair, the schedule was bad, nobody helped me,” that immaturity does more damage than the fail itself.
This is the part nobody prepares you for. Step 3 timing is not just an entry in your CV. It’s a story of how you behave under competing responsibilities.
Strategic Advice: If You Haven’t Taken Step 3 Yet
Let me be concrete.
If you’re still in med school
Best move if you can swing it: late MS4 when you’re relatively free and still in test mode. Especially if:
- You’re US grad, strong Step 1/2, and want high-flexibility for future state licenses or fellowships
- You’re IMG trying to look rock-solid for residency
You want it done before life as an intern punches you in the face.
If you’re PGY-1 and it’s not done
Target: mid–late intern year on a lighter rotation, before you’re writing fellowship personal statements or acting as a full senior.
Do not push it to the absolute last block of the year. That’s how you become “the late one” in email threads the PD sees.
If you’re already late
Own it. Build a plan that looks like this to your PD:
- Clear written timeline
- Honest acknowledgment that the delay was suboptimal
- Specific protections to avoid repeating the same pattern
Then execute. No drama. No excuses.

| Step | Description |
|---|---|
| Step 1 | Have you started residency? |
| Step 2 | Take in late MS4 if possible |
| Step 3 | Schedule Step 3 during that block |
| Step 4 | Pick least intense month, start Qbank now |
| Step 5 | High priority: meet with PD, set date within 3 months |
| Step 6 | Light rotation available in next 6 months? |
That’s how you convert a potential red flag into a “late but they handled it like an adult” impression.
How Programs Quietly Compare You: A Snapshot
Here’s how three archetypes land in a PD’s mind when discussed side by side.
| Profile | Timing & Behavior | Unspoken PD Interpretation |
|---|---|---|
| Early Finisher | Late MS4 / early PGY-1, solid pass | Planner, low risk, probably ambitious |
| Standard Planner | Mid–late PGY-1 on light rotation | Normal, reliable, no drama |
| Late and Scrambling | End PGY-1 / PGY-2, last‑minute scheduling | Procrastinator, potential liability |
It’s not always this neat, but it’s closer to reality than what anyone admits publicly.
FAQ: Step 3 Timing, As PDs Actually See It
1. If I get a high Step 3 score, does timing still matter?
Yes, but differently. A strong Step 3 taken in a reasonable window (late MS4 to mid PGY-1) reinforces a positive story: strong test taker, good planner. A high score taken very late with a messy narrative still raises eyebrows about why you delayed it, even though the test-taking concern goes away. For fellowships, they care that it’s done and looks consistent with your prior performance; they’re not ranking people purely on Step 3 numbers.
2. Is it better to take Step 3 early and risk a mediocre score, or later with more prep?
If “early” means before you can realistically pass comfortably, that’s dumb. Programs are far more spooked by a failure than by a slightly later test date. Ideal: take it early enough that it doesn’t interfere with senior responsibilities or fellowship apps, but not so early that you’re gambling your first attempt. A clean pass in a sane window beats an early risky attempt every time.
3. How much should I tell my PD if I’m behind on Step 3?
More than you think, but with a plan attached. Do not show up with “I’m behind and anxious” as your message. Show up with: “I know I’m behind, here’s why, here’s the exact date I’m registering for, here’s my specific preparation plan, and here’s how I’ll protect my clinical duties.” PDs hate surprises and vague anxiety. They respect residents who own problems early and come in solution-first.
Key points: Your Step 3 timing is a signal, not a footnote. Programs are reading it for planning ability, risk, and maturity under pressure. Do it in a sane window, communicate like an adult, and avoid turning a simple exam into a narrative about chaos and procrastination.






















