The usual advice about residency letters is dangerously simplistic when you are targeting more than one competitive field.
If you treat letter selection like a generic checkbox exercise, you will quietly sink your chances in all of your target specialties.
You are trying to do three hard things at once:
- Look like a serious candidate to each field.
- Avoid looking unfocused or “shopping” around.
- Not burn bridges with any department.
That requires actual strategy. Not vibes.
Below is the playbook I have seen work for students chasing multiple competitive options: derm vs medicine, ENT vs prelim surgery, rads vs anesthesia, EM vs IM, etc.
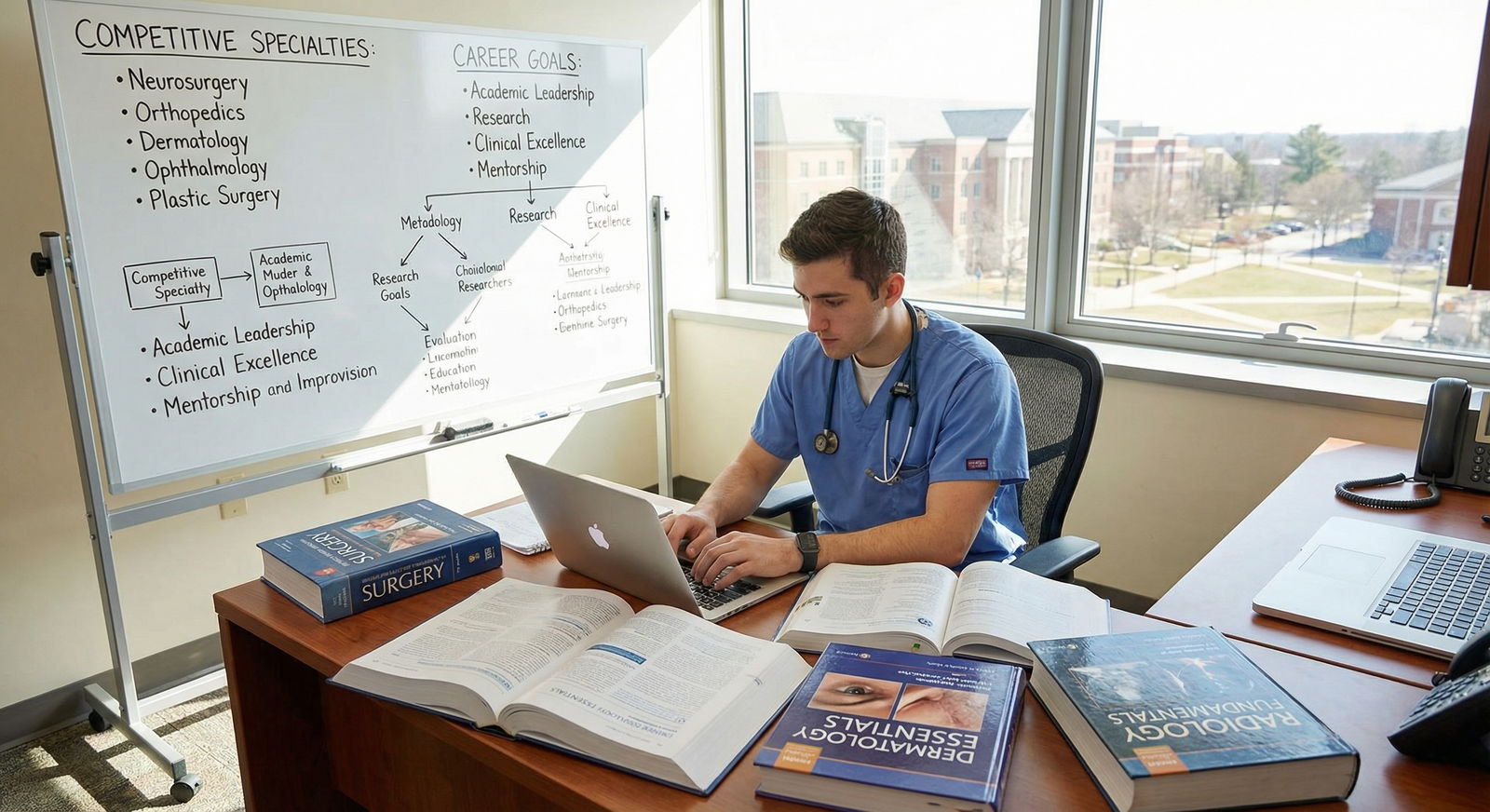
1. First, Get Real About Competitiveness and Risk
You cannot design a good letter strategy if you lie to yourself about how competitive your targets are.

| Category | Value |
|---|---|
| Top Tier (Derm/Plast/NSurg/ENT/Optho/Ortho) | 9 |
| Upper Mid (RAD, Gas, EM) | 7 |
| Mid (IM, Peds, OB/GYN) | 5 |
| Lower (FM, Psych, Neuro) | 3 |
This is not a perfect ranking, but it matches what PDs actually say behind closed doors:
- Tier 1: Dermatology, Plastic Surgery, Neurosurgery, ENT, Ophthalmology, Orthopedics
- Tier 2: Radiology, Anesthesiology, Emergency Medicine (varies by region), some surgical subs
- Tier 3: Internal Medicine, Pediatrics, OB/GYN, General Surgery at many programs
- Tier 4: Family Med, Psych, Neuro, Path (though top programs can still be brutal)
Your letter strategy changes based on:
- How high your Step scores are relative to these fields
- How strong your home department support is
- Whether you have a realistic “safety” specialty you would actually be willing to match into
If you are aiming at:
- Two Tier 1’s (Derm + Plast). Very tough. You must commit your letters per application, and programs will smell hedging quickly.
- One Tier 1 + one Tier 2 or 3 (Derm + IM). Manageable with a sharp plan.
- Two mid-tier fields (IM + EM, OB/GYN + Peds). Common and fixable with structure.
The risk: if your letters make you look “half in,” you will get filtered out in the busiest applicant piles. I have heard PDs say “If I sense they are not all in, I move on; I have 800 other files.”
So we design your letters to tell a coherent story for each field.
2. Understand What Programs Actually Want from Letters
Programs care about three things, in this order:
- Signal of commitment to the field
- Credible assessment from someone they trust
- Evidence that you will not be a problem (work ethic, professionalism, teamwork)
They do NOT care that:
- You got letters from the “fanciest” names if the content is generic
- You collected maximum possible letters “just in case”
- You had a Nobel laureate who barely knows you sign something boilerplate
Here is the basic letter expectation by specialty type:
| Target Field Type | Ideal Letter Mix (for that application) |
|---|---|
| Surgical (ortho, ENT, gen surg) | 2+ surgeons (field-specific), 1 medicine/peds or research |
| Medicine-like (IM, neuro, peds) | 2 IM/peds/neuro, 1 wildcard (research or subspecialty) |
| Lifestyle/Procedure (rads, gas, derm) | 1–2 field-specific, 1–2 strong IM/surg/EM backing |
| EM | 2 SLOEs if possible, 1 other clinician who knows you well |
When you apply to more than one field, you cannot show every program this whole mix. ERAS caps how many letters you can assign per program (usually 3–4). Which forces choices.
The rule: each field must see at least:
- 1 letter clearly anchoring you to that field
- 1 letter proving you are a solid, reliable physician in broader terms
- 1 “power” letter from someone who knows you extremely well
Sometimes one letter can check two boxes. That is where strategy lives.
3. Design Your Overall Letter Portfolio First
Before you ask anyone for anything, map out your portfolio of letters like you would plan a chess match.
Step 1: Define your field mix
Common combos I see:
- Derm + IM
- EM + IM
- Ortho + Gen Surg (or prelim surgery)
- Anesthesia + IM
- Radiology + IM
- OB/GYN + Peds
- ENT + Gen Surg
Write down your combos explicitly. Not in your head. On paper.
Step 2: Build a target letter grid
Create a grid of “ideal” letters you would assign to each field if you could get everything you want.
Example: Student targeting Derm + IM
For Derm programs:
- Derm attending (away rotation) – field commitment + performance
- Derm attending (home) – field commitment + continuity
- IM attending – shows you can manage complex medicine, reliable resident
- Research mentor (ideally derm-related) – scholarship, work ethic
For IM programs:
- IM ward attending (sub-I) – core bread-and-butter evaluation
- Another IM attending or subspecialist – consistency
- Derm attending (if letter is framed as “excellent future internist with an interest in skin”) or research mentor – academic potential
Now mark:
- Which letters will exist in reality
- Who is likely to write strong vs lukewarm letters
- Which ones you can reuse safely across fields
You are aiming for 5–6 total letters in your ERAS pool, not 9. Beyond that, it becomes chaos and you start forgetting who said what.

| Category | Value |
|---|---|
| Too Few (≤3) | 10 |
| Optimal (4–6) | 70 |
| Too Many (≥7) | 20 |
4–6 letters gives you enough flexibility to customize per field without looking scattered.
4. How to Ask for Letters Without Broadcasting You Are “Shopping”
You need to manage optics. Departments are small; attendings talk.
Here is the move that works:
A. Anchor yourself to one “primary” field in each conversation
When you ask an attending for a letter, you do not lead with “I am applying to three specialties and still deciding.” That is how you get a generic letter.
Instead:
- For a derm attending: “I am applying dermatology and internal medicine, but dermatology is my primary goal. I would be very grateful if you could comment on my strengths that would make me a strong dermatology resident.”
- For an IM attending: “I am applying internal medicine and dermatology. Regardless of ultimate field, I know I will be an internist first, and I would value your assessment of me as a future internal medicine resident.”
The attending hears: commitment. Clarity. Respect for their field.
B. Be explicit about multi-field use when needed
Some letters should be multi-purpose. For those, say so:
“I plan to use your letter for both internal medicine and dermatology applications. Would you be comfortable writing a letter that focuses on my clinical reasoning, reliability, and growth on the team, which would be relevant to both fields?”
Do NOT:
- Ask someone to tailor different versions to different fields. Most will not do this, and it often backfires.
- Hide that you are applying broadly if the letter is obviously generic. If they find out later, it damages trust.
Pick 1–2 letters that are explicitly field-specific, and the others are “core doctor” letters.
5. Field-by-Field Strategy: Common Multi-Target Scenarios
Let me walk through practical letter setups for some of the most common combos.
Scenario 1: EM + IM
Very common. EM wants SLOEs. IM wants IM heavy letters. They read each other’s letters differently.
Ideal letter pool (total 5–6 letters):
- 2 EM SLOEs (one home, one away if possible)
- 2 IM attendings (ward, sub-I, or ICU)
- 1 research or longitudinal mentor (could be EM, IM, or something else)
For EM applications (assign 3–4 letters):
- EM SLOE #1 (home)
- EM SLOE #2 (away)
- IM attending who can speak to clinical reasoning + reliability
- Optional: research mentor if they know you clinically or on work ethic
For IM applications:
- IM attending #1 (sub-I if you can)
- IM attending #2
- EM SLOE that comments on your intern-level readiness and team function
- Research mentor letter
Key trick: When you do your EM rotations, tell your SLOE writer:
“I am primarily applying EM but also internal medicine. I would appreciate it if you could comment on my ability to function in a medicine-heavy, inpatient setting as well.”
That makes the SLOE less “EM-or-bust” and more generally useful.
Scenario 2: Derm + IM
Derm wants derm-specific enthusiasm and academic potential. IM wants proof you will not crumble as an intern.
Ideal letter pool (5–6 letters):
- 2 derm attendings (home + away if possible)
- 1 IM sub-I attending
- 1 additional IM attending or subspecialist
- 1–2 research mentors (at least one derm-related if you can)
For Derm applications (3–4 letters):
- Derm attending #1 (who saw you day-to-day)
- Derm attending #2 OR derm research mentor
- IM attending who can say “this person will be an excellent intern”
- Optional: non-derm research mentor if known very well
For IM applications:
- IM sub-I attending
- Another IM attending or subspecialist
- Derm research mentor reframed: “has skills that will make them an excellent academic internist with a focus on skin disease”
- Optional: derm clinical attending only if they are willing to speak to your general medicine skills and work ethic, not just “they like derm”
Critical error I see: students send two derm letters to IM programs that basically say “future dermatologist” and nothing about intern performance. IM PDs read that as: “Will transfer out the second they get a derm spot.”
So when you ask the derm research mentor, say:
“I will use this letter for both dermatology and internal medicine. Could you please comment on my ability to handle data, follow through on projects, and communicate with the team — not just my interest in dermatology?”
You are giving them a blueprint.
Scenario 3: Ortho or ENT + General Surgery / Prelim
Surgical people are blunt. They care about work ethic, resilience, technical potential, and how you behave at 2 a.m. during a messy consult.
Ideal letter pool (5–6 letters):
- 2 letters from the target field (ortho or ENT attendings, including away rotations)
- 1–2 general surgery attendings who saw you grind
- 1 research letter (ideally in related field, but not mandatory)
For Ortho/ENT applications:
- Field attending #1 (home)
- Field attending #2 (away)
- Gen surg attending who will say you work like a resident already
- Optional research mentor
For Gen Surg or Prelim:
- Gen surg attending #1
- Gen surg attending #2
- Ortho/ENT attending reframed: “hard worker, reliable, technical potential”
- Research mentor if academic track matters
When you ask a general surgery attending and you are primarily aiming for Ortho, you say:
“I am applying to orthopedic surgery, but I am also applying to categorical and prelim general surgery programs. If you feel comfortable, I would be grateful for a letter that focuses on my ability to function on a busy surgical service and potential as a surgical resident, regardless of subspecialty.”
They respect that.
6. Avoid These Common, Quietly Fatal Mistakes
Mistake 1: Over-indexing on research letters
One strong research letter is plenty for most fields. Two is sometimes useful for derm, rad onc, plastics if they are truly powerhouse letters.
But three research letters and one lukewarm clinical letter? That screams: “Unproven clinician.”
If you have:
- 1 superstar PI letter (R01, known name)
- 1 clinical letter that is merely “fine”
Do not assume the famous PI cancels out the mediocre clinical evidence. Programs value reliable day-1 intern over “future Nobel” almost every time.
Mistake 2: Using obviously mismatched letters
Example:
Sending a gushing EM SLOE to a dermatology program where the narrative is all about “handles chaos in the ED; thrives in high-acuity emergencies.”
Derm PD reads this and thinks: “So why are you here?”
Letters do not have to be tailored to the field, but they should not contradict your story. If the tone, examples, and language scream a different specialty, do not attach it to the wrong programs.
Mistake 3: Too many total letters in ERAS
Nine letters in your file looks like:
- You could not decide what you are doing
- You begged everyone for a letter without discernment
- Half of them are probably weak
More letters do not mean more strength. They mean more risk.
Target:
- 4 minimum
- 5–6 ideal if you are truly multi-field
Stop there.
7. How to Decide Which Letters to Attach Program by Program
You will face this annoying ERAS reality:
You might have 6 letters uploaded but can only assign 3–4 to each program.
Here is a clean, mechanical decision rule that works.
Step 1: Identify your “universal” letter
Pick one letter that will go to almost every program:
- The best all-around clinical evaluator who saw you work hard
- Ideally not tied strongly to a niche field narrative
- Speaks to: reliability, clinical judgment, communication, professionalism
This becomes your anchor letter.
Step 2: For each field, define your must-have
For each specialty, what is the non-negotiable “must attach” letter?
- For EM: at least one SLOE
- For Derm: at least one derm attending or derm PI
- For IM: at least one strong inpatient IM attending
- For surgery fields: at least one surgeon in that specialty
Those are your field anchors.
Step 3: The “swing” slot(s)
The remaining 1–2 slots are your flexible positions:
- Research letter if they care about academic potential
- Second field-specific letter for top-tier programs
- Strong cross-field clinical letter (e.g., EM SLOE used for IM at community programs that value workhorse interns)
So at each program you attach:
- Universal anchor
- Field anchor #1
- Field anchor #2 (if needed for that field’s norms)
- Best remaining letter that strengthens your specific story (academic, workhorse, sub-I, etc.)

| Step | Description |
|---|---|
| Step 1 | Program in Target Field |
| Step 2 | Attach Universal Anchor Letter |
| Step 3 | Attach Field Anchor Letter |
| Step 4 | Choose Strongest Clinical Letter |
| Step 5 | Add Best Research or Extra Clinical Letter |
| Step 6 | Done |
| Step 7 | Field Requires Specific Letter Type |
| Step 8 | Slots Remaining? |
You do not overthink every single program. You apply this simple structure consistently.
8. Timing and Logistics: Do Not Sabotage Yourself with Chaos
Letter strategy falls apart if you mismanage timing.
Concrete timeline

| Period | Event |
|---|---|
| Early MS3 - Feb-Mar | Identify target fields |
| Early MS3 - Mar-Apr | Plan rotations and potential letter writers |
| Late MS3 - May-Jun | Ask first wave of letter writers |
| Late MS3 - Jul-Aug | Complete key sub-I and away rotations |
| Early MS4 - Aug-Sep | Confirm letters uploaded, assign per field |
Practical moves:
- Ask for letters while you are still fresh in the attending’s memory (within 1–2 weeks of finishing rotation).
- Give them a short CV + bullet list of what you did on their service.
- State clearly: “I will use this letter for X and possibly Y. Is that acceptable to you?”
Keep a simple spreadsheet:
- Who you asked
- Date you asked
- Field focus (EM, IM, derm, etc.)
- Whether they agreed
- Whether the letter is uploaded
Do not rely on ERAS alone to tell you who has or has not submitted.
9. What To Do If You Are Late Deciding Your Field
Common scenario: You thought you were 100% EM, then halfway through fourth year you realize you really prefer IM. Or you were sure about anesthesia, then discover rads is a better fit.
You are not doomed, but you must act deliberately.
If you already have field-specific letters
Example: You have 2 strong EM SLOEs and now you want to apply predominantly IM.
You:
- Keep 1 SLOE as a demonstration of strong clinical performance and team function.
- Aggressively secure 2–3 IM letters ASAP (sub-I, wards, ICU).
- Ask EM SLOE writer if they are comfortable with you using the letter for IM as well, and if it broadly reflects your clinical abilities, not just EM enthusiasm.
Then in your personal statement for IM, you explain your shift clearly. PDs will reconcile the EM letter with your new narrative if it makes sense and your IM letters are solid.
If you do not have enough field-specific letters
Worst case: You decided on derm in August of MS4 with no derm letters. Right as ERAS opens.
Brutal, but here is the salvage plan:
- Get on any available derm elective ASAP, even later in the fall.
- Use IM + research letters to apply broadly this cycle, acknowledging your late decision.
- Recognize you might not match derm this year and mentally prepare to do a strong prelim year or research year and reapply.
In ultra-competitive fields, you cannot letter your way out of a structurally weak application in one month. Better to be realistic and create a two-year plan than pretend.
FAQ (Exactly 3 Questions)
1. Is it bad if a letter clearly states I am applying to multiple specialties?
Not necessarily. What matters is framing. “This student is applying to both emergency medicine and internal medicine; I would be happy to train them in either field” is fine. It shows you are strong and versatile. The bad version is: “The student is still undecided and exploring options,” which reads as unfocused and non-committal. Your ask and your personal statement should give attendings a clear, confident story to echo.
2. Should I prioritize a famous name who barely knows me or a mid-level faculty who knows me well?
Take the mid-level faculty who knows you, almost every time. PDs can smell a templated “I supervised this student briefly” letter from an academic celebrity. A detailed, specific narrative from an associate program director or busy ward attending carries more weight. The only exception is when the “famous” person truly knows your work in depth and is willing to write a very specific, personalized letter.
3. How many non-clinical letters (research, volunteer, leadership) is too many?
More than one or two, and you are overdoing it for most specialties. A single outstanding research or leadership letter can be a big asset, especially in academic programs. But if half your letters are non-clinical, PDs will question how you perform on the wards. Aim for at least two strong clinical letters for any field, then add one high-impact non-clinical letter if it genuinely strengthens your story.
Key points to walk away with:
- Map your fields and build a deliberate 4–6 letter portfolio, not a random pile.
- Give each field at least one clear “anchor” letter plus a universal clinical letter that proves you are a safe, hardworking resident.
- Control the narrative when you ask for letters and when you assign them — programs forgive multiple interests but rarely forgive looking unfocused or half-in.





















