The usual way DO students judge residency programs is backwards. Step 1: “Do they take DOs?” Step 2: “What's the board pass rate?” Then people stop thinking. That is not how you find high‑quality ACGME training for osteopathic physicians.
If you care about actually becoming an excellent, employable DO––not just matching somewhere––you need to look under the hood. Deep. Because two programs with identical “DO friendly” reputations can produce very different graduates.
Here is what actually matters for DO training quality in ACGME programs, and how to evaluate it without wasting years of your life.
1. DO Culture vs. DO Tokenism
The first filter is not “Do they accept DOs?” It is “How are DOs treated once they get there?”
You want programs where DOs are normal, not exceptions.
Red flags:
- 1 DO in a sea of 40 MDs
- Everyone still says “AOA” when they mean “ACGME”
- Faculty repeatedly confuse COMLEX with old osteopathic boards
- Residents joke about “you guys having different anatomy” (I’ve heard this more than once)
Green flags:
- Multiple DOs in each PGY class
- DOs in chief positions in the last 3–5 years
- DO attendings on core faculty (especially PD or APD)
- Explicit mention of COMLEX/osteopathic pathways in orientation materials or website
Here’s how programs tend to break down:
| Level | DO Presence | Signal You’ll See |
|---|---|---|
| Strong | ≥25–30% residents are DOs | Recent DO chiefs, DO faculty |
| Moderate | 10–25% DOs | DOs present but not in leadership |
| Token | ≤10% DOs | 1–2 DOs per program, no leaders |
| Hostile | Almost no DOs | PD vague or defensive about DOs |
You want Strong. Moderate is acceptable if other factors are excellent. Token is risky unless you have a very specific reason. Hostile? Keep walking.
On interview day, literally count DO badges on the residents. Ask: “Have DOs been chiefs here in the last few years?” If they dodge, that’s your answer.
2. COMLEX vs. USMLE: What Actually Matters Now
You already know the party line: “Just take USMLE too.” Reality is more nuanced.
For DO training quality, the key questions are:
- Does the program truly understand COMLEX?
- Do they have objective score cutoffs for DOs?
- Do they use COMLEX for promotion/board readiness, or pretend it does not exist?
Ask specific questions:
- “Roughly what COMLEX Level 1/2 scores are typical for your incoming DO residents?”
- “Do your DO residents also take USMLE, or is COMLEX alone common here?”
- “How do you track board readiness for DOs vs MDs?”
If they say:
- “We do not really know COMLEX; we just multiply by ~10”… that’s lazy and sloppy.
- “We require USMLE from DO applicants” but current DO residents did not all take it… that’s two standards. Bad sign.
What you want:
- A clear statement: “We’re comfortable with COMLEX alone; our typical DOs have Level 1 around ___, Level 2 around ___.”
- An honest recognition that USMLE helps for some fellowships but is not mandatory for solid training.
Here’s the practical translation:

| Category | Value |
|---|---|
| Mid-tier IM | 215 |
| Competitive IM | 225 |
| Community EM | 210 |
| University EM | 220 |
Roughly:
- COMLEX Level 2 score ~ 240–250 = comfortable for solid academic IM/EM/FM programs
- COMLEX Level 2 score ~ 260+ = opens doors at more competitive or “MD-heavy” programs
Do not obsess about “conversion formulas.” Instead, figure out if the program has validated real DO success with COMLEX-only residents. Ask them.
3. Osteopathic Recognition and OMT: Overrated but Not Useless
A lot of DO students chase “Osteopathic Recognition” like it’s a quality seal. It is not. It’s a targeted accreditation focused on osteopathic principles and OMT. That does not automatically mean better overall training.
What matters:
- Do you personally want to use OMT weekly in practice?
- Is OMT part of your identity and long‑term plan (sports med, pain, rural primary care)?
- Or do you mainly want rock‑solid clinical training and a job?
Programs with Osteopathic Recognition can be very good. They can also be mediocre clinically but strong on OMT. I’ve seen both.
Good signs:
- Protected OMT clinic time
- Faculty who actually do OMT in real practice, not just as a checkbox
- Integration into hospital care (OMT consults for pregnancy, post-op ileus, headaches, etc.)
Bad signs:
- “We have an OMT afternoon once a month but we’re often pulled for floor coverage”
- One overworked DO faculty member trying to cover everything
- Residents quietly saying, “We basically do not do OMT”
If OMT is essential to you, then yes, Osteopathic Recognition with genuine integration matters a lot. If you just want to keep skills alive, a program with several DOs and at least one DO faculty may be plenty.
4. Clinical Volume, Autonomy, and Breadth
Now the meat of training quality. This applies to everyone, but DOs often end up over‑focusing on “friendliness” and under‑weighting actual case volume and autonomy. Bad trade.
You need:
- High patient volumes
- Progressively increasing responsibility
- Enough procedural exposure to be independently competent by graduation
Here’s what residents complain about after they graduate:
- “I never learned to run the ICU”
- “We barely saw bread‑and‑butter procedures”
- “Attendings micromanaged everything; I was not ready to be on my own”
Ask specific questions:
- “How many new patients do interns typically carry on a ward month?”
- “Who runs codes at night? Senior or attending?”
- “By graduation, how many central lines, intubations, LPs, etc. do residents usually have?”
- “Are there any procedures you feel underprepared for?”
If you hear:
- “Our attendings do most of the tough procedures” – that may sound nice; it is actually bad for your growth.
- “We’re very cushy” – translation: maybe low volume, maybe weak training.
You want busy, but not malignant. Tired, but not broken.
5. Faculty Quality and Teaching Culture (Especially for DOs)
Faculty can make or break your experience as a DO.
Look for:
- At least one DO in core leadership (PD, APD, site director, or major committee)
- Faculty who know your name and goals
- Real, structured feedback, not just “Good job”
Ask:
- “How often do you get formal feedback on rotations?”
- “Do attendings ever give you direct teaching at the bedside, or is it all ‘look it up’?”
- “Are there DO faculty here, and are they involved in resident mentorship?”
Red flags:
- All teaching is via PowerPoints, no bedside teaching
- Residents say they “learn the most” from other residents, not faculty
- DO residents quietly say: “The MD faculty are fine, they just do not really get the DO thing”
You are not looking for a spiritual DO temple. You’re looking for a place where osteopathic identity is respected and understood, and where faculty are actually good clinicians and teachers.
6. Board Pass Rates and Graduate Outcomes (Do They Help DOs Succeed?)
Yes, board pass rates matter. But not the way programs advertise them.
Everyone says “100% pass rate” for the last X years. Missing detail: they often filtered who was “allowed” to sit for boards.
What you should ask:
- “How many residents in the past 3 years did not pass boards on the first attempt?”
- “Do DOs and MDs get the same board prep support?”
- “Do you pay for board prep resources (e.g., UWorld, TrueLearn) and time off to study?”
What really matters:
- Structured board prep baked into the schedule
- Program-funded question banks and review courses
- Clear remediation process for struggling trainees
And then the big one: What do graduates actually do?
Ask:
- “Where did your last 3 DO graduates go after residency?”
- “Do DOs here match into competitive fellowships at similar rates to MDs?”
- “Can I see a list of fellowships and jobs for the last 5 years?”
If graduates (especially DOs) land where you want to land, that is the single strongest signal of training quality.
7. Fellowship and Career Support for DOs
If you are targeting fellowship—cards, GI, heme/onc, EM subspecialties—you must stop thinking “residency only” and start asking, “Who will pick up the phone for me?”
Key features:
- PD and faculty who are known and respected in your target field
- Prior DO residents who matched into solid fellowships
- Real mentorship, not vague encouragement
Ask pointedly:
- “Have any DOs from your program matched into [your field] in the last 5–7 years?”
- “Which fellowships regularly interview your residents?”
- “Who typically writes letters for fellowship applicants here?”
If they cannot name DOs who matched in your desired area, assume it will be harder for you. Not impossible, but harder.

| Step | Description |
|---|---|
| Step 1 | Identify Programs |
| Step 2 | Low Priority |
| Step 3 | Only if limited options |
| Step 4 | High Priority Rank |
| Step 5 | DO Presence >= 20%? |
| Step 6 | Good Volume & Autonomy? |
| Step 7 | Board & Fellowship Outcomes? |
8. Program Environment: Malignant vs. Supportive (Not the Same as “Nice”)
Everyone says their culture is “family-like.” That phrase is meaningless. You want to know:
- Are residents protected from abuse?
- Are DOs treated equally when things go wrong?
- Is the place survivable for three or more years?
Ask residents privately:
- “Have you ever seen anyone get yelled at or humiliated in front of others?”
- “Are there any attendings everyone dreads working with?”
- “When people struggle—DO or MD—how does the program respond?”
Listen for:
- “It is busy but fair” – usually okay
- “There are a couple of attendings who are rough, but leadership listens” – borderline but manageable
- “People cry on this service” – believe them
For DOs specifically, ask:
- “Have DOs ever felt singled out or treated differently?”
- “Any issues with rotations / procedures / fellowship letters for DOs vs MDs?”
The reactions you see on residents’ faces will tell you more than any official answer.
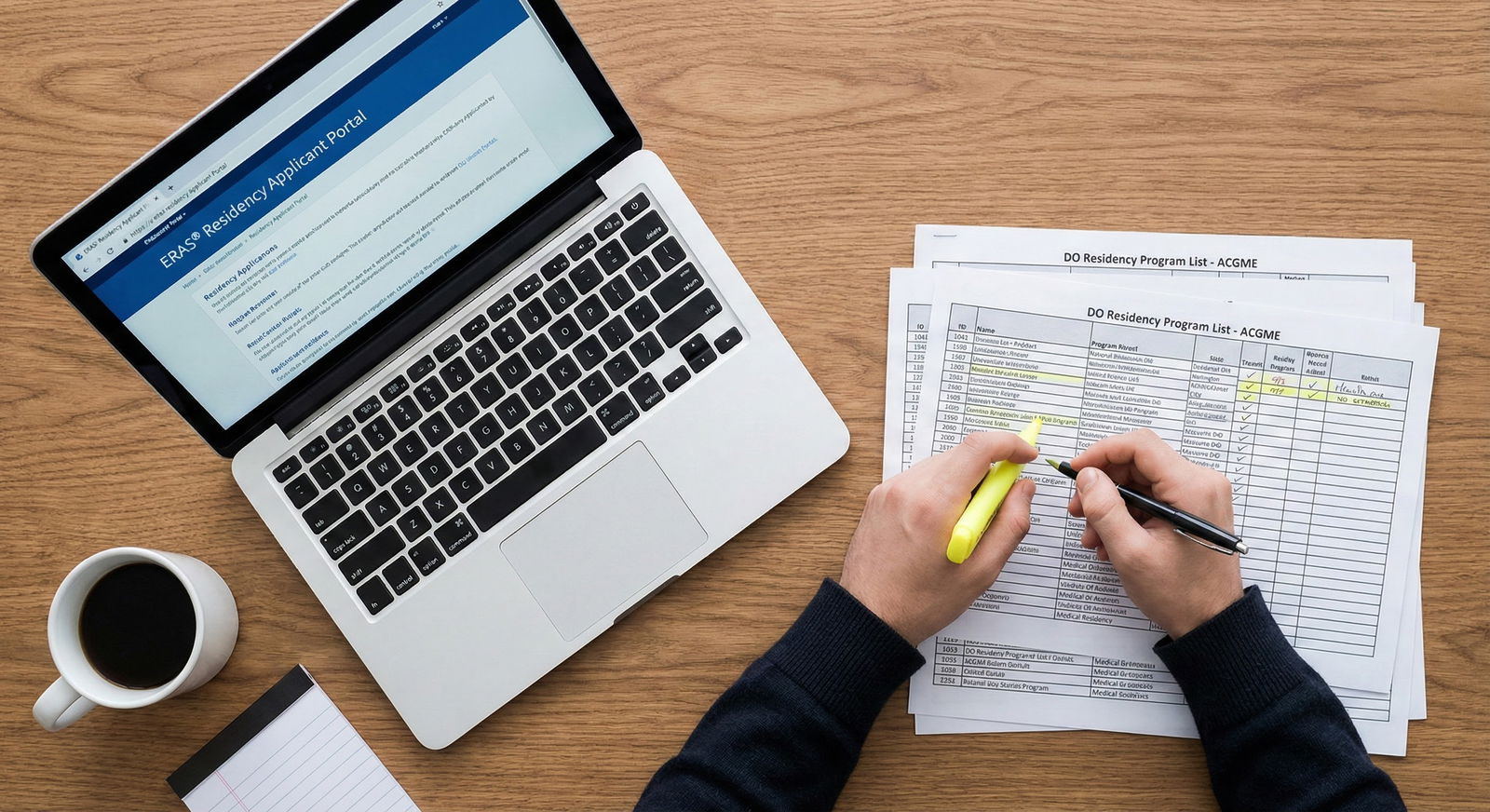
9. Practical Checklist: What To Actually Do
Stop relying on vibes. Use a structured approach.

| Category | Value |
|---|---|
| Clinical Volume & Autonomy | 30 |
| DO Culture & Representation | 25 |
| Board/Fellowship Outcomes | 20 |
| Faculty & Teaching | 15 |
| OMT/Osteopathic Features | 10 |
Rough weighting (my opinionated breakdown):
- 30% Clinical volume and autonomy
- 25% DO culture and representation
- 20% Board and fellowship outcomes
- 15% Faculty and teaching quality
- 10% OMT/osteopathic recognition (more if OMT is central to your goals)
On every interview:
- Count DOs in the room. Ask about DO chiefs and DO faculty.
- Drill into clinical exposure: numbers, responsibilities, procedures.
- Ask specific board and fellowship questions, broken down by DO vs MD when possible.
- Pull one DO resident aside and ask, “Would you choose this place again as a DO?”
After interviews, rank programs based on where you will become the strongest, most independent physician—who just happens to be a DO.
10. Common Traps DO Applicants Fall Into
I’ve watched DO students repeat the same mistakes every match cycle. Avoid these:
- Overvaluing “Osteopathic Recognition” while ignoring weak clinical volume.
- Prioritizing “cushy” lifestyle over real responsibility and independence.
- Assuming any “DO friendly” program will advocate for them in fellowship.
- Not researching where recent DO grads actually ended up.
- Ignoring subtle disrespect or confusion about osteopathic training because “the program is prestigious.”
Your job is not to win a name. Your job is to become good enough that 5 years later nobody cares whether your diploma says DO or MD—because your work speaks for itself.
FAQ: ACGME Program Features for DO Training Quality
1. Do I really need an ACGME program with Osteopathic Recognition as a DO?
No. It is nice if you want OMT as a core part of your practice, but it is not required for high‑quality training. Many excellent ACGME programs without Osteopathic Recognition train DOs extremely well, support COMLEX, and produce strong graduates. Focus first on clinical volume, autonomy, outcomes, and DO culture. Use Osteopathic Recognition as a tie‑breaker, not the starting point.
2. Is it a mistake to go to a program where I’d be the only DO?
Usually, yes—unless everything else is outstanding and you have a clear reason. Being the only DO often means more explaining, more skepticism, and less institutional memory of how to support DO residents. If you consider such a program, you must confirm: prior DO graduates succeeded there, leadership is explicitly supportive of DO training, and they understand COMLEX and osteopathic differences.
3. How much should I care about whether a PD is a DO vs an MD?
The PD’s attitude toward DOs matters more than their letters. A DO PD can be fantastic or terrible. Same with an MD PD. What counts: DO representation in leadership somewhere (PD, APD, chiefs, key faculty), equal treatment of DO residents, and a track record of DO graduates doing well. Do not worship titles—look at outcomes and culture.
4. If I want a competitive fellowship, should I avoid community programs as a DO?
Not automatically. A strong community program with high volume, excellent faculty who advocate for you, and a history of sending DOs to reputable fellowships can beat a big‑name academic program that barely knows what to do with DOs. But: for the very top competitive fellowships, brand and faculty connections matter. In that case, target mid‑to‑large academic programs that already have DOs successfully matching into your field.
5. What’s one question that quickly reveals if a program is good for DOs?
Ask: “Can you tell me about 2–3 recent DO graduates—where they started, how they were supported, and where they ended up?” A strong program will easily name names, describe real mentorship, and point to solid jobs or fellowships. A weak one will stumble, be vague, or generalize: “Our DOs do fine.” If they cannot tell you real stories, they probably are not truly investing in DO trainees.
Open your program list right now and circle the ones where you can clearly answer: “Yes, DOs here have thrived.” If you cannot say that confidently, move them down your rank list—no matter how shiny the name.




















