
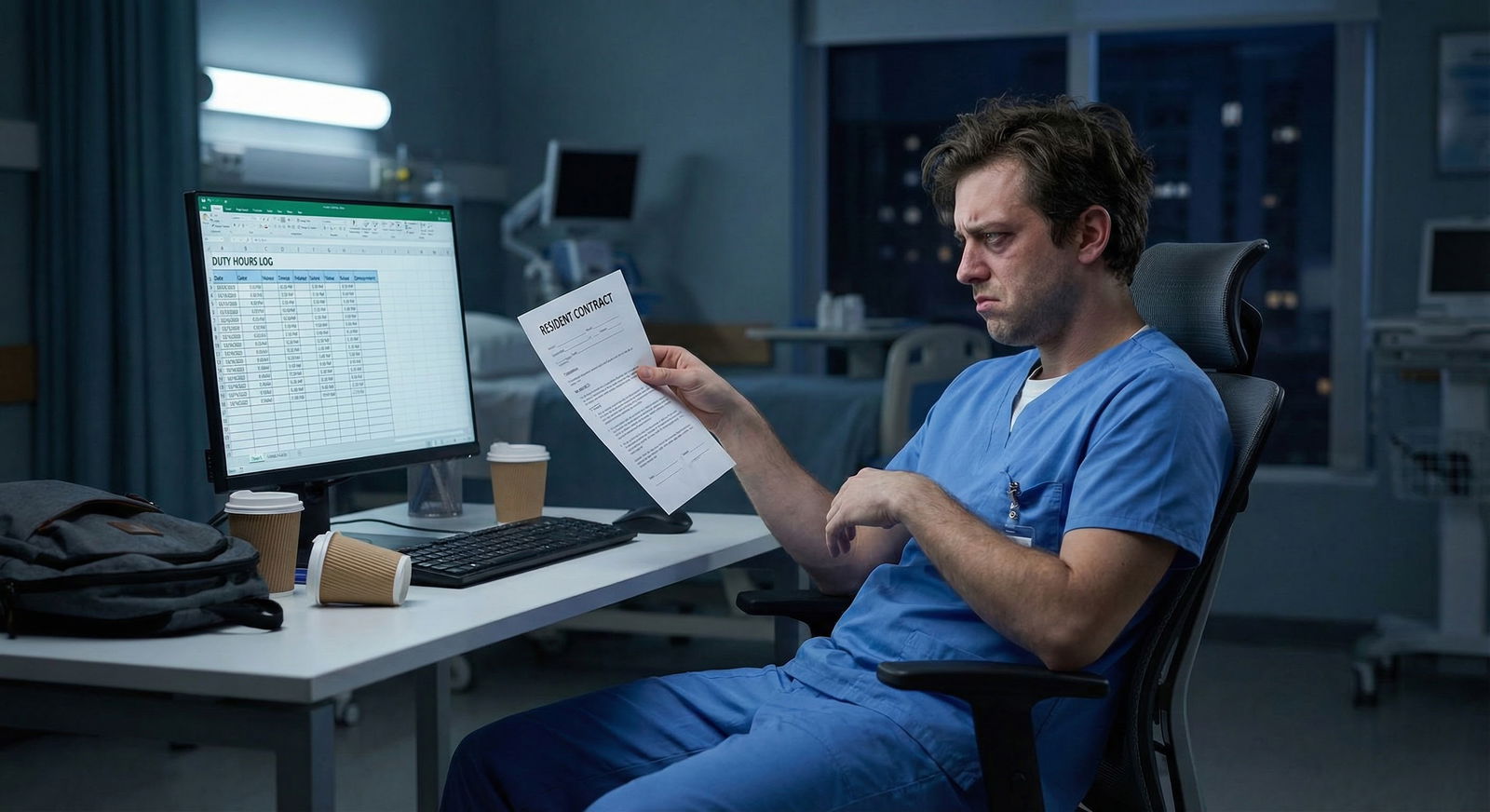
The dangerous myth is that your residency contract protects your moonlighting income. It doesn’t.
The Panic Scenario: Your Program Just Pulled the Plug
You’re mid‑PGY‑2. You’ve finally figured out how to survive 28‑hour calls, you’ve lined up a sweet moonlighting gig in the ED that pays $120/hour, and for the first time, your bank account doesn’t make you nauseous.
Then, out of nowhere, an email:
“Effective immediately, all moonlighting activities are suspended pending further review. This applies to internal and external moonlighting. Failure to comply may result in disciplinary action.”
Your stomach drops. You already counted that money. You need that money. Rent. Loans. Maybe daycare. Maybe supporting family. It’s not “extra” for fun; it’s how you were planning to not drown.
And now you’re doing the math in your head, at 2 a.m. between pages:
- How am I supposed to pay my loans next month?
- Can they even do this?
- What if I push back and they blacklist me for fellowship?
- Is this the thing that ruins my entire financial life?
Let’s walk straight into the ugly parts, because pretending “it’ll all work out” isn’t helping anyone.

| Category | Value |
|---|---|
| Rely heavily | 45 |
| Use as buffer | 35 |
| Mostly optional | 20 |
Can They Actually Ban Moonlighting Mid‑Training?
Short answer: yes, they usually can. And they do.
Most residency contracts and institutional policies are written to protect the program, not you. Buried in the fine print you were too exhausted to read on orientation day, there’s usually language like:
- “Outside employment must be approved by the Program Director or GME office.”
- “Approval may be modified or revoked at any time at the discretion of the program or institution.”
- “Duty hour, patient safety, or educational concerns may result in suspension of moonlighting.”
So what happens when they “suddenly” ban it?
Common triggers I’ve seen:
- ACGME site visit flagged duty hour issues
- Someone fell asleep on service after a long moonlighting shift
- New program director who hates moonlighting on principle
- Legal/insurance got nervous about malpractice coverage
- Hospital finances change and they don’t want residents competing for paid shifts
The worst part? They don’t have to care about your financial situation. Their argument is always the same:
- Patient safety
- Education first
- Duty hours compliance
- Liability
You can rage at the unfairness (and honestly, you’d be right). But from a power standpoint? They’re holding all the cards.
That doesn’t mean you’re helpless though. It means you have to be strategic instead of emotional.

| Step | Description |
|---|---|
| Step 1 | Moonlighting banned |
| Step 2 | Cut urgent expenses |
| Step 3 | Gather info |
| Step 4 | Talk to PD or GME |
| Step 5 | Short term patch plan |
| Step 6 | Long term financial reset |
| Step 7 | Side income options |
| Step 8 | Immediate crisis? |
| Step 9 | Permanent or temporary? |
Step 1: Don’t Get Yourself in Trouble
Your first panicked instinct might be: “I’ll just keep doing it quietly.” Don’t.
This is where worst‑case scenarios get real:
- You get caught → “unprofessional behavior,” probation, maybe a letter that haunts your fellowship apps.
- You go over 80 hours → ACGME violation, program freaks out, they use you as the example.
- You’re in an accident driving home from a moonlighting shift the program banned → liability nightmare.
I’m not saying any of this is fair. I’m saying this is exactly how programs think.
So you stop. Immediately. Even if the moonlighting place is begging you to come in. Even if they say “we’ve always done this under the radar.” They don’t answer when ACGME calls. You do.
You can tell the moonlighting site:
“My program just issued a blanket ban. I can’t risk my training. If this changes, I’ll reach out.”
Protecting your residency status is non‑negotiable. Losing your ability to graduate on time to hang onto a few shifts? That’s a financial catastrophe you don’t recover from.
Step 2: Figure Out if This Is a Temporary Fire or a Permanent Ice Age
Before you spiral into “my life is ruined,” you need data.
You schedule a calm, short meeting with:
- Program Director or
- Associate Program Director you trust or
- GME office if the email came from them
And you ask, very plainly:
- “Is this expected to be temporary or permanent?”
- “Is this tied to an ACGME issue, or is this a new philosophy of the program?”
- “Are there any exceptions at all, like senior residents, internal shifts, or specific settings?”
- “Is there a timeline for reevaluating this policy?”
You are not arguing. You are gathering information.
You can also ask, without sounding entitled:
“A number of residents, myself included, budgeted based on moonlighting income. If this is going to be ongoing, is the department or institution considering any stipends, bonuses, or other support?”
Most places will say no. Sometimes they’ll surprise you with:
- A small “educational stipend” increase
- Extra call pay
- An internal “coverage” pool that’s technically not called moonlighting
But they won’t offer it unless they feel some pressure and realize it’s a real burden. You don’t have to cry in their office (unless you do, that happens). Just be concrete:
“I’m concerned about affording [rent/childcare/loan payments] without the income I was getting from moonlighting. I want to keep my training my priority, but this does create a serious financial strain.”
Now you at least know if you’re planning for 3–6 months of pain, or a totally different residency reality.
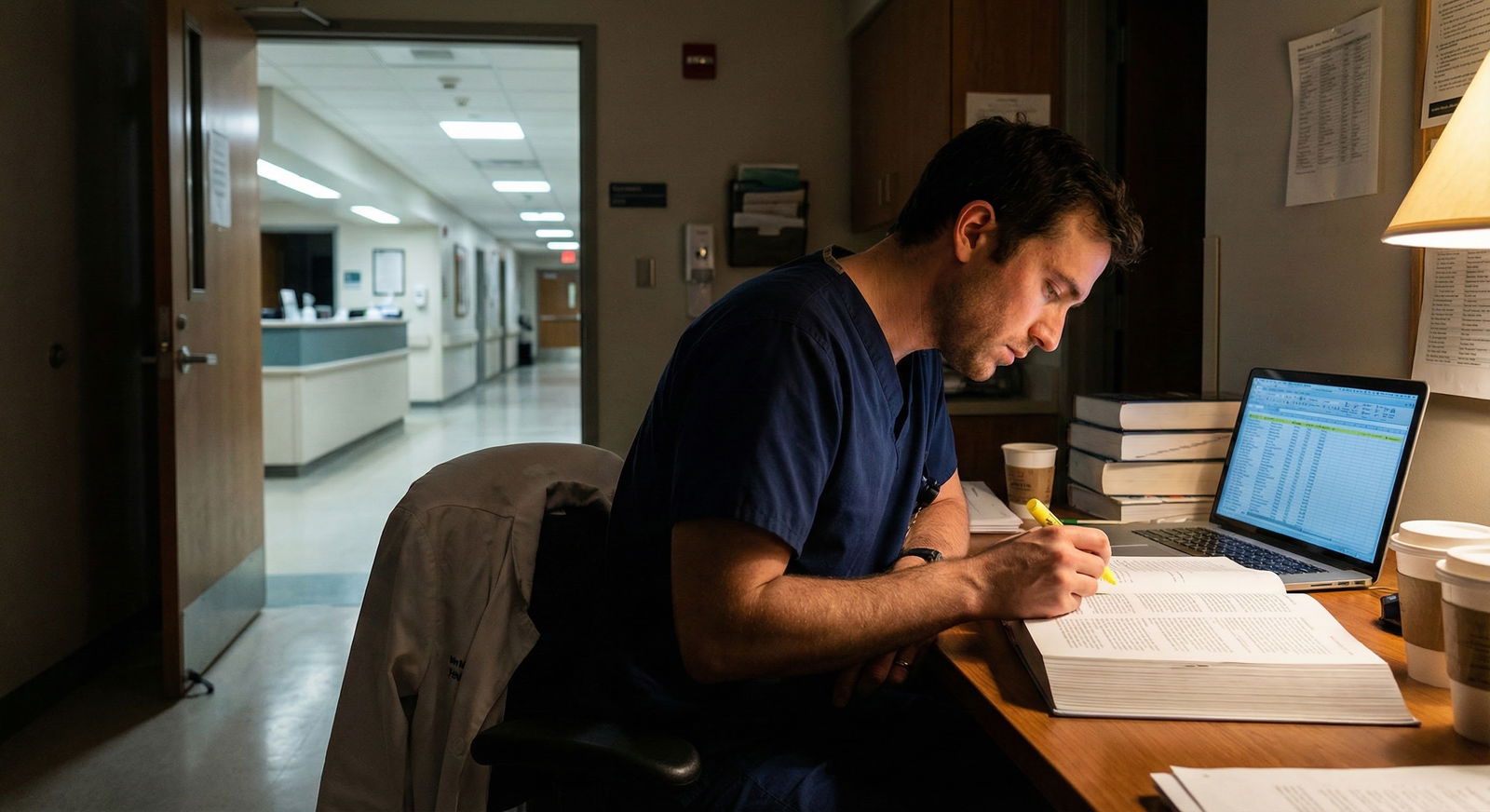
Step 3: Do the Financial Triage You’ve Been Avoiding
This is the part that feels awful, because you’re already working 70–80 hours and now you have to be your own financial planner on top of it.
But if moonlighting was paying, say, $2,000–$3,000/month, you cannot pretend that hole doesn’t exist.
You make a list. Not in your head. On paper or in a spreadsheet:
Fixed essentials
- Rent / mortgage
- Utilities
- Food (realistic, not DoorDash fantasy)
- Transportation / car / insurance
- Childcare
Debts
- Student loans
- Credit cards
- Personal loans
Non‑essentials / flex
- Subscriptions (gym, streaming, apps, cloud storage)
- Eating out
- Travel
- Random Amazon “I’m stressed” purchases
Then three uncomfortable moves:
Call your student loan servicer.
- Ask about income‑driven repayment, lower payments, or temporary reduction.
- If you’re on PAYE/REPAYE/SAVE, double‑check your income numbers are updated.
Call any high‑interest credit cards.
- Ask (yes, actually ask) for a lower APR, hardship plan, or temporary reduced payment.
- They won’t advertise these, but they exist.
Be ruthless with subscriptions and lifestyle creep.
- Nobody wants to hear “you might need roommates again” as a PGY‑3, but I’ve seen it happen and honestly, it’s better than drowning in 24.99 autopays and late fees.
You’re not cutting joy forever. You’re stabilizing the bleeding so one institutional email doesn’t wreck your credit score for the next 7 years.
| Category | With Moonlighting | Without Moonlighting |
|---|---|---|
| Take-home pay | $5,500 | $3,500 |
| Rent/Housing | $1,800 | $1,800 |
| Loans/Debt | $1,000 | $1,000 |
| Childcare | $800 | $800 |
| Leftover | $1,900 | -$100 |
This is why it feels like the world is ending. Because for some residents, that moonlighting money isn’t “extra.” It’s the only part of the budget that makes math even remotely work.
Step 4: Look for “Non‑Moonlighting” Income You Won’t Get Fired For
Is there any way to bring in money that doesn’t violate the ban? Sometimes, yes. But you have to thread the needle:
Key rule: anything clinical that looks, smells, or feels like “a shift as a doctor” is probably banned.
But some things are less clear:
Internal coverage that’s technically part of your residency.
Example: Extra jeopardy call that the program pays a small stipend for. It’s not “moonlighting,” it’s “additional call coverage.” Ask your chief residents if these exist.Paid teaching or tutoring.
- MCAT tutoring, USMLE tutoring, pre‑med coaching.
- Many residents do this on the side, online, away from the hospital.
- Your program might still require disclosure, but it usually doesn’t violate the clinical moonlighting ban.
Non‑medical side gigs.
- Editing personal statements.
- Tech/consulting if you had a pre‑med life.
- Simple remote jobs that don’t conflict with duty hours.
Stipended roles.
- Some hospitals pay small stipends for chief roles, QI leadership, or committee work. It won’t replace full moonlighting pay, but it’s something.
You must check your institutional policy, though. Some programs are control‑freak enough to require approval for any outside work, even non‑clinical. They hide this in the GME handbook.
Yes, that’s intrusive. Yes, they still do it.
But here’s the honest calculation: a little humiliation emailing GME to ask “Is USMLE tutoring okay?” is better than being summoned to the PD’s office with a printout of your side business LinkedIn.

| Category | Value |
|---|---|
| Clinical work | 55 |
| Admin/Charting | 10 |
| Sleep | 35 |
| Personal | 10 |
| Possible Side Gig | 5 |
Step 5: Prepare for This Before You Ever Start Moonlighting
This is the part nobody tells you as an MS4 or intern when you hear residents bragging:
“Yeah, I just paid off a whole credit card with moonlighting last month.”
Moonlighting feels permanent when you first taste it. It isn’t. It’s fragile. It depends on:
- Your program’s mood
- ACGME rules
- Malpractice coverage
- Some administrator not freaking out about duty hours
So if you’re reading this before your own disaster email:
Do not build fixed expenses on top of moonlighting.
- Don’t sign a 2‑year lease assuming those shifts will exist.
- Don’t buy the car “that only works if I do 4 shifts/month.”
Treat moonlighting as unstable bonus money.
- Use it for: emergency fund, high‑interest debt, short‑term goals.
- Not: long‑term monthly commitments that you can’t cover with base salary.
Keep a 1–2 month “if they cut me off” buffer.
I know, saving during residency sounds like a joke. But even a small cushion means the next “effective immediately” email is a crisis, not a catastrophe.
You’re not paranoid if you expect institutions to change rules mid‑game. You’re just paying attention.
Emotional Side: This Feels Like a Betrayal (Because It Kind of Is)
There’s the money panic, and then there’s the deeper anger: you planned like an adult, you found a way to not be completely broke, and someone who makes 3–4x your salary just took it away by email.
You’re allowed to be pissed.
Common mental spirals I’ve seen and lived:
- “If they cared about resident well‑being, they wouldn’t do this.”
- “I’m an adult physician, but they treat me like a child.”
- “I made promises to my family based on this income. Now I look irresponsible.”
You’re not imagining the power imbalance. They do control your graduation, your letters, your reputation. That’s what makes this all feel so trapped.
But here’s the part that actually helps: separate the institution’s behavior from your own worth or competence.
You didn’t screw up by planning to moonlight. You didn’t mess up because someone changed the rules. They can yank the policy; they don’t get to rewrite your narrative as “irresponsible” because you relied on what they allowed for years.
If this policy change makes you think, “I cannot work under people who treat residents like this,” that feeling is valid. You can use it:
- To shape what kind of fellowship or job you choose later
- To ask pointed questions as an attending interviewing somewhere: “What’s your moonlighting policy and how often have you changed it?”
You’re not powerless forever. Just not as powerful as you deserve right now.
When the Numbers Truly Don’t Work
Here’s the nightmare thought you probably haven’t said out loud:
“What if even after cutting and negotiating and side gigs… it still doesn’t add up? What then? Do I drop out?”
Usually, it doesn’t come to that. But sometimes, for residents with:
- heavy family responsibilities
- single incomes in expensive cities
- massive private loans
…it can feel impossible.
If you’re there, you don’t suffer in silence. You loop in:
- GME office, explicitly about financial hardship
- Social work / employee assistance programs
- Your union, if you’re in a unionized program (they can sometimes push back hard)
- A trusted attending/mentor who can quietly advocate
I’ve seen:
- Short‑term hardship grants
- Temporary housing support
- Creative solutions around call pay or stipends
- Rarely, relocation to a different program/hospital where your situation is more sustainable
It’s not guaranteed. It’s not fair. But you have more options when you name the problem early instead of quietly racking up 20k in credit card debt out of shame.

Quick Reality Check Before You Spiral
You’re not the first resident whose program killed moonlighting overnight. You’re not the last. Programs panic, policies swing, graduates move on, new residents arrive, and the wheel keeps turning.
That doesn’t pay your rent this month, but it does mean:
- This situation is survivable
- It doesn’t define your whole career
- You’ll probably be the attending later warning your residents: “Do not rely on moonlighting to pay core bills. I watched that get nuked mid‑year.”
In the meantime, your job is simple, not easy:
- Protect your training status
- Stabilize your finances enough to avoid long‑term damage
- Find small, policy‑compliant ways to bring in extra if you really need to
- Remember that this is a season, not a sentence
You’re allowed to hate it. You’re also capable of getting through it.
FAQ (Exactly 6 Questions)
1. Can I argue that my contract guaranteed moonlighting and they can’t change it?
Almost always, no. Most contracts or GME policies say moonlighting is “at the discretion of the program” or requires ongoing approval. Even if they mentioned moonlighting at recruitment, unless your contract says something like “you are guaranteed X hours of moonlighting at Y rate,” they can change or revoke approval whenever they want. You can ask for clarification, but a legal fight over this as a resident? Not worth the risk to your training.
2. What if I already signed a contract with an outside moonlighting site?
You read that contract carefully. Most have clauses that let either party terminate with notice. You reach out and say your program just changed policy and you’re no longer allowed to work there. Institutions that hire residents to moonlight are used to this; they won’t be shocked. Better a burned bridge with a moonlighting site than a scar on your residency record for violating program policy.
3. Are internal moonlighting shifts (within my own hospital) different?
Sometimes. Some programs ban external moonlighting but still allow internal paid shifts that they tightly control and monitor for duty hours. Other programs lump everything together and ban all extra paid clinical work. The only way to know is to ask specifically: “Does this ban apply to internal coverage/extra shifts too, or only external moonlighting?” Do not assume internal is safe unless they explicitly say so.
4. Will a moonlighting ban hurt my fellowship or job applications?
The ban itself? No. Programs know moonlighting rules change all the time. What hurts you is if you ignore the ban, get caught, and end up with a professionalism/probation note in your file. That’s the thing PDs talk about on the phone. If anything, being the resident who handled the change calmly, asked smart questions, and didn’t blow up might actually earn you quiet respect from faculty.
5. Is it worth switching programs over something like this?
Usually not in the middle of training, unless your entire situation is toxic beyond just moonlighting. Changing programs is messy: licensing, ACGME approval, possibly repeating a year, losing seniority. But if you were already miserable, financially drowning, and the moonlighting ban is just the last straw, it might be one of several factors pushing you to consider a move. Just be realistic about how hard it is to transfer and the risk it carries.
6. What if my co‑residents keep secretly moonlighting after the ban and tell me to do it too?
They don’t graduate for you. They don’t sit in your PD’s office when things go sideways. If the program made a clear policy, and you knowingly break it, you’re gambling your future on “they probably won’t find out.” And let’s be honest: they always find out eventually—through scheduling conflicts, billing, social media, or simple gossip. You can feel jealous, you can feel pressured, but you’re the one who lives with the consequences. If you’re already panicking reading this, that’s your gut saying: don’t risk it.
Key points:
- Programs absolutely can ban moonlighting mid‑training, and fighting the policy head‑on is usually a losing battle.
- Your first job is to protect your residency status, then stabilize your finances with ruthless budgeting, negotiation, and allowed side income.
- Never build your core life expenses on moonlighting—treat it as unstable bonus money, because institutions can pull it with one email.

















