
The blunt truth: training in a rural region does not automatically limit your urban job prospects — but training in a weak program absolutely will. Location is secondary. Program quality, reputation, and your own choices are what actually move the needle.
Let’s untangle this properly, because a lot of people get this wrong.
The Real Question You Should Be Asking
You’re not actually asking, “Is rural bad and urban good?”
You’re asking:
- Will employers in big cities take me seriously if I train in a smaller, rural program?
- Will I be locked into “rural-only” jobs?
- Will I miss out on fellowships, networking, or high-acuity exposure?
Here’s my position up front:
- A strong rural program beats a mediocre urban program for your career.
- Urban employers care more about:
- How good your training is
- Your clinical competence and references
- Whether you’ve shown interest/experience in urban-style practice
- You can absolutely match into urban jobs and fellowships from rural training — but you need to be intentional.
The doctors I’ve seen “stuck” after rural training weren’t stuck because of geography. They were stuck because they coasted, didn’t network, and didn’t build a clear story for what they wanted next.
How Employers in Urban Areas Actually Think
Urban hospital administrators and group leads are not sitting there with a map saying, “We only hire people who trained in cities.”
They’re asking three questions:
- Can this person handle our patient population and volume?
- Can I trust them to be safe, efficient, and not a nightmare to work with?
- Do they have experience or clear interest in our kind of practice?
Where “rural vs urban” does sneak in is as a proxy. They worry (fairly or unfairly) about:
- Volume: Did you see enough patients and pathology?
- Acuity: Did you manage sick enough patients, or will you be overwhelmed in our ED/ICU/trauma center?
- Systems: Have you worked with larger teams, consult-heavy workflows, and complex health systems?
A solid rural or regional program can absolutely answer “yes” to all of those. A tiny, under-resourced, under-accredited program may not.
Rural Training: Real Advantages and Real Risks
Forget the romantic brochure shot of a resident holding a baby in a barn. Here’s what rural or regional programs typically actually give you.
Real Advantages
Broader hands-on responsibility.
You’re not one of 50 residents fighting over procedures. You intubate. You reduce joints. You run codes. You make decisions.Earlier autonomy.
Urban academic centers can be very layered and hierarchical. In many rural setups, you’re “the doc” much earlier (with backup, yes, but still).Strong continuity with attendings.
Smaller faculty → they really know you. That means stronger letters and more willingness to pick up the phone for you when you apply to urban jobs or fellowships.Generalist skillset.
Urban employers, especially in community hospitals, love a well-rounded physician who can handle a bit of everything and isn’t helpless without a 10-subspecialty backup.
Real Risks
Limited subspecialty exposure.
Less tertiary/quaternary care. Fewer zebras. Less “cutting-edge” imaging/procedures. This matters a lot if you’re chasing high-end specialties.Weaker name recognition.
If your program is “Regional Medical Center of Somewhere” and you’re applying to a big private group in a top-10 city, they might not instantly know your program. You’ll have to show your quality through CV, letters, and interviews.Fewer onsite fellowships.
In many rural regions, pipeline fellowships (cards, GI, heme/onc, etc.) just aren’t there. That means more hustle to get exposure and letters from tertiary centers.
So the tradeoff isn’t “rural vs urban.” It’s “autonomy, broad practice, and strong faculty relationships” versus “brand name, subspecialty proximity, and volume of exotic pathology.”
When Rural Training Is Totally Fine for Urban Jobs
Let’s talk concrete scenarios.
You’re usually in good shape if:
You’re going into primary care (FM, IM, peds) and want to work in:
- Large urban outpatient clinics
- Hospitalist roles in city hospitals
- Urgent care or large health system employment
You’re in EM, anesthesia, psych, or OB/Gyn at a regional hub that has:
- Decent trauma exposure or a partnership with a regional trauma center
- ICU exposure and critical care management
- Enough volume and diversity of pathology
You train at a well-regarded regional academic or hybrid program with:
- Solid board pass rates
- Ok to strong fellowship matches
- Known faculty who regularly interact with bigger centers (referrals, conferences, multi-center trials)
In these cases, urban jobs are absolutely in play. I’ve seen IM residents from places like “Regional Health X” land:
- Urban hospitalist roles in major cities
- Outpatient IM jobs with big multispecialty groups
- Even fellowships at larger academic centers, though that requires more intentional planning.
When Rural Training Can Make Urban Roles Harder
There are times where your training environment will genuinely limit your options — and those limits would exist whether that place is rural or urban.
Red flags:
Minimal volume and limited acuity.
If your ED sees very low daily volume, or your ICU is tiny and ships out almost everything, you’re going to have a harder time convincing a high-volume urban center you’re ready to hit the ground running.Poor program reputation or instability.
Chronic ACGME citations, constantly changing leadership, high resident attrition. Urban employers may not say it out loud, but they notice.No track record of graduates going to cities or fellowships.
If literally everyone stays in the town or nearby and nobody’s made the jump to big-city jobs, understand that you’ll be the one blazing that trail. It’s doable, but not automatic.
This is where people quietly get burned. They don’t look at the outcomes of prior grads, sign onto a weaker program (because “any residency is fine, right?”) and then discover a ceiling.
What Urban Employers Look At (Beyond Your ZIP Code)
Let’s be specific. For urban jobs, the usual filters are:
| Factor | How Much It Matters |
|---|---|
| Program reputation | High |
| Letters of recommendation | High |
| Interview performance | High |
| Geographic training site | Low–Medium |
| Fellowship or extra training | Medium–High |
A few patterns I’ve actually seen:
- IM resident from a small Midwest regional program → lands hospitalist job in a major coastal city because: excellent letters, strong chief year, did an away elective at a big urban hospital.
- FM resident at a rural-focused program → gets turned down from several boutique “concierge-style” city clinics because their program had low name recognition and they did zero urban outpatient electives. Fixed it by doing a 1-year fellowship in sports med at a city program, then reapplied.
- EM resident from a rural-heavy program → easily hired by a large multi-hospital urban system because they ran tons of codes, did procedures, and had stellar references from a regional trauma rotation.
Notice the pattern: the program’s reputation and your track record matter more than GPS coordinates.
Specific Strategies if You Train Rural and Want Urban
If you’re already in (or likely headed toward) a rural or regional program but want the option of an urban career later, here’s how you stack the deck.
1. Choose the Right Kind of Rural Program
Not all “rural” is equal. You want:
- Affiliation with a larger academic center or health system
- Strong board pass rates
- Documented graduates going to urban jobs or solid fellowships
- Clear volume in your core areas (clinic visits, admissions, ED visits, deliveries, OR cases)
If the program director dodges questions like “Where have your recent graduates gone?” — that’s a problem.
2. Get Urban or Tertiary Exposure During Training
Don’t just live inside one hospital forever.
Do away rotations or electives at:
- A large urban academic center
- A high-volume specialty service (e.g., cards, ICU, trauma, subspecialty clinic)
Go where your target jobs or fellowships are.
Want to work in Chicago, Seattle, or NYC later? Try to get 1–2 rotations there. Let people see you work.
This gives future employers something relatable: “Oh, you rotated here and Dr. X remembers you? Great.”
3. Build Relationships That Cross Regions
Your letters don’t all have to be from your home program.
- Get one or two letters from faculty at larger or urban centers where you’ve rotated.
- Go to regional/national conferences. Present a poster. Shake hands. Have someone say, “Yeah, I know her; she was sharp.”
Networking is not just a buzzword. It’s how people from unknown programs get taken seriously by hiring committees who live inside big-city bubbles.
4. Shape Your CV Toward Urban Practice
You can’t change where your hospital is, but you can change how relevant you look.
Examples:
Want an urban hospitalist job?
- Do extra inpatient months
- Moonlight in busier community hospitals (if allowed)
- Get strong ICU and procedures exposure
Want urban outpatient primary care?
- Beef up your chronic disease management, behavioral health, and complex multi-morbidity experience
- Do electives in urban FQHCs or high-volume clinics
Want a subspecialty in the city?
- Research, subspecialty electives, and strong letters from academic physicians become non-negotiable.
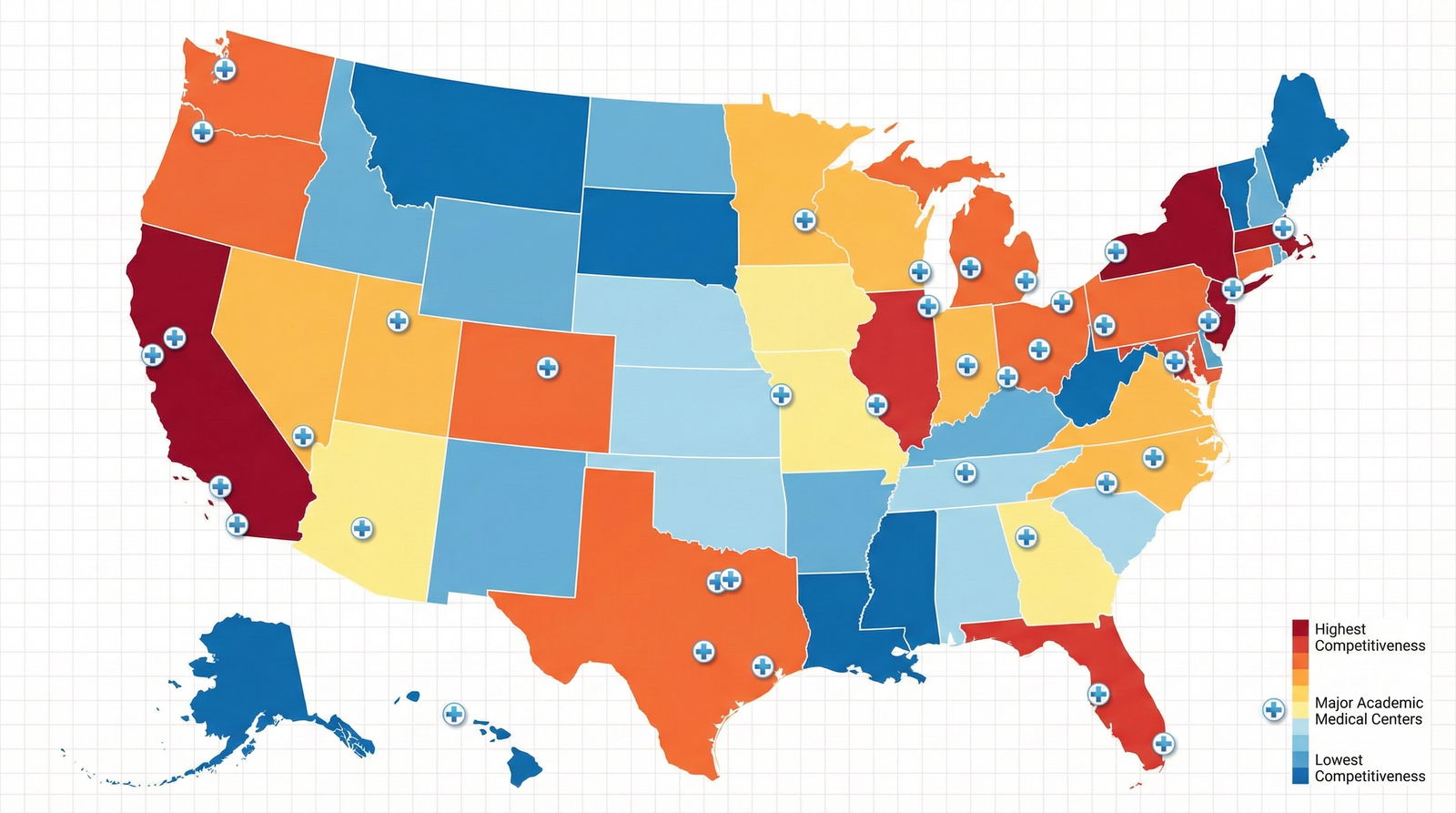
How This Plays Out by Specialty
Different specialties care differently about rural vs urban training.

| Category | Value |
|---|---|
| Family Medicine | 9 |
| Internal Medicine | 8 |
| Emergency Medicine | 7 |
| Psychiatry | 8 |
| Surgical Specialties | 5 |
Scale: 1 = very restrictive, 10 = flexible for urban jobs.
- Family Medicine – Very flexible. Rural FM can make you extremely attractive to urban underserved clinics, FQHCs, and big systems.
- Internal Medicine – Also flexible, especially for hospitalist and general outpatient roles. Fellowship-heavy paths (cards, GI) may require more strategy.
- Emergency Medicine – Rural/regional EM can be excellent, especially if trauma/ICU exposure is good. Urban academic tertiary EM may be trickier but not impossible.
- Psychiatry – Very flexible. Urban psych demand is huge. Exposure to severe mental illness is key; many rural programs still provide this.
- Surgical Specialties – This is where program volume and case mix matter a lot. A truly rural, low-volume surgery program can absolutely constrain you for competitive urban jobs and fellowships.
The One Thing That Will Limit You
Let me be crystal clear: a low-quality residency program — rural or urban — will absolutely limit your job prospects.
Signs you’re dealing with that:
- Weak supervision or inconsistent attendings
- Poor exam pass rates
- No clear educational structure
- Graduates struggling to find jobs or fellowships they actually want
- Constant negative gossip about the program from nearby hospitals
If that place happens to be rural, don’t blame “rural” for closing doors later. Blame the program.
Same if it’s an urban program with a big name hospital system but terrible teaching and chaos. That also hurts you.
Simple Decision Framework: Will This Hurt My Urban Options?
Run your current or prospective program through this quick filter:

| Step | Description |
|---|---|
| Step 1 | Considering rural program |
| Step 2 | High risk for any job, avoid |
| Step 3 | Urban high acuity jobs harder |
| Step 4 | You can be first but need hustle |
| Step 5 | Urban jobs very feasible |
| Step 6 | ACGME accredited and stable? |
| Step 7 | Good board pass rates? |
| Step 8 | Solid volume and acuity? |
| Step 9 | Grads getting urban jobs or fellowships? |
If you land on E or G, that doesn’t mean “don’t go.” It means “go in with eyes open and plan earlier.”
Regional vs Urban Training Outcomes Snapshot
| Factor | Strong Rural/Regional Program | Mid-Tier Urban Program |
|---|---|---|
| Hands-on procedures | Often higher | Variable |
| Name recognition | Lower–medium | Medium–higher |
| Path to urban community job | Very feasible | Very feasible |
| Path to top academic role | Possible but harder | Easier, if you hustle |
| Faculty knowing you well | Typically stronger | Depends on program size |
What You Should Do Today
Open a new document and write three things:
- Where you’d ideally like to work after training (rough city and setting).
- The kind of medicine you want to practice (hospitalist vs outpatient vs procedural vs subspecialty).
- Your current or target residency programs — and where they stand on:
- Volume and acuity
- Board pass rates
- Graduate job/fellowship outcomes, especially in urban areas
Then email or meet with one person at your program (or a mentor) and ask them one specific question:
“Can you show me recent graduates from this program who are now working in big-city jobs or fellowships like the ones I’m interested in?”
Their answer — and how easily they can back it up — will tell you more about your urban prospects than the population size of the town around your hospital ever will.
FAQ: Rural Training and Urban Jobs
1. Will a rural residency hurt my chances of getting a competitive urban fellowship?
It can, but not automatically. What matters more is program quality, research output, and letters from recognizable faculty. If you’re at a rural or regional program and aiming for something like cards, GI, or heme/onc in a major city, you’ll probably need:
- Strong board scores
- Subspecialty electives at larger centers
- Some research or scholarly work
- At least one letter from a well-known academic attending
I’ve seen people go from strong regional IM programs to urban fellowships. It’s just rarely an “I did nothing and fell into it” situation.
2. Do recruiters actually care if I trained rural versus urban?
Most recruiters care about: board certification/eligibility, visa status (if relevant), malpractice history, and whether your story fits the job. Hiring physicians will look harder at your training, but geography is a minor factor. What does sometimes happen: if your program is very rural and low-volume, they’ll ask more questions about whether you’re comfortable with high-volume, complex urban care.
3. If I do rural training, should I plan on a fellowship to get back to a city?
Not necessarily. For many specialties (FM, IM, EM, psych), you can go straight from residency into urban jobs without a fellowship. A fellowship can help if:
- Your residency is weaker and you want to “upgrade” your pedigree
- You’re changing your focus (e.g., FM → sports med in a city)
- You want a very competitive urban niche (e.g., ICU-focused academic job)
It’s a tool, not a requirement.
4. How can I tell if a rural program has enough volume and acuity?
Don’t trust the brochure. Ask specific questions:
- How many admissions per resident per call night on average?
- How many deliveries/surgeries/trauma activations/ICU beds?
- How often are patients transferred out, and for what?
- Can I see anonymized case logs of recent grads?
If they can’t or won’t answer those with real numbers, be cautious.
5. I’m already in a very rural, low-name program. Is it too late to aim for an urban job?
No, but you’ve got to be proactive:
- Maximize every high-acuity rotation you have
- Seek external electives or visiting rotations in city hospitals
- Go to conferences, present something, and meet people
- Get the strongest possible letters from the best-known faculty you can access
- Be ready to explain clearly in interviews how your training prepared you for an urban environment
Your next step today: email your PD and ask about possibilities for external electives at larger centers — especially in cities where you might want to work.
















