
You’ve been lied to about residency: the idea that you must completely obliterate your personal life “for the good of your training” is outdated, lazy, and not supported by the data.
Do some residents get crushed? Yes. Do all have to? No. And pretending otherwise just excuses bad systems and bad habits.
Let’s separate three things people constantly mix up:
- Residency is hard.
- Residency can be exploitative.
- Residency requires you to have no personal life.
Only the first one is universally true.
The “No Life in Residency” Myth and Why It Persists
The myth sounds like this:
- “If you’re not miserable, you’re not working hard enough.”
- “You can have a life after training.”
- “Residency is supposed to break you down.”
I’ve heard those exact sentences in workrooms and call rooms. Usually from attendings who trained before duty hours, or from PGY-3s who’ve normalized dysfunction because “I survived it, so you should too.”
But look at what’s actually changed:

| Category | Value |
|---|---|
| Pre-2003 | 100 |
| 2003-2010 | 80 |
| 2011-2019 | 70 |
| 2020+ | 65 |
No, this chart does not mean residency is cushy now. It means the old-school 110–hour weeks are no longer the baseline. Yet the narrative about residency hasn’t updated. People are still talking like it’s 1995.
Why the myth survives:
- It flatters people who suffered (“we were tougher”).
- It absolves programs from fixing structural problems (“this is just how it is”).
- It gives residents a ready-made identity: the martyr doctor with no life.
The truth is more annoying because it demands responsibility from everyone: programs, attendings, and yes, you.
What the Data Actually Shows About Hours, Burnout, and “Having a Life”
Let’s start with what’s been measured instead of hallway folklore.
Work hours vs burnout: it’s not that simple
Residents are working fewer average hours now than two decades ago, yet burnout is still extremely common. Depending on specialty and study, burnout rates run around 40–70%.
If “amount of work” were the only factor, you’d expect burnout to track neatly with hours. But look at this:

| Category | Value |
|---|---|
| Low Control | 70 |
| Moderate Control | 50 |
| High Control | 30 |
That’s the pattern in multiple studies: feeling you have no control predicts burnout far more strongly than raw hours alone. Same with:
- Chaotic workflows
- Poor supervision
- Toxic culture
- Constant page/EMR ping interruptions
That means this: you can be working 60–70 hours and feel like you have zero life if your schedule is unpredictable, your days spill into nights, and every off day gets hijacked by “just one more thing.”
Flip side: I’ve seen residents on very busy services still protect:
- weekly dinners with a partner,
- a standing gym slot with a co-resident,
- or Sunday morning with their kid at the park.
Were they sleeping 10 hours a night? No. But they were not living the “no life until attendinghood” script.
The specialties people love to demonize
People love to say: “Sure, maybe peds has balance, but not surgery / EM / IM / OB.” Reality is more nuanced.
| Specialty | Average Hours/Week |
|---|---|
| General Surgery | 70–80 |
| Internal Med | 60–70 |
| OB/GYN | 65–75 |
| Pediatrics | 55–65 |
| EM | 45–55 |
These are ballpark ACGME-era approximations, but you get the idea.
Notice something: none of those numbers inherently prohibit a personal life. They restrict it. They strain it. But they don’t mathematically erase it.
So when someone says, “In surgery, you just accept you have no life,” what they actually mean is:
- The culture often punishes boundary-setting.
- The schedule is unpredictable.
- Seniors/attendings may model self-erasure as virtue.
That’s culture, not physics.
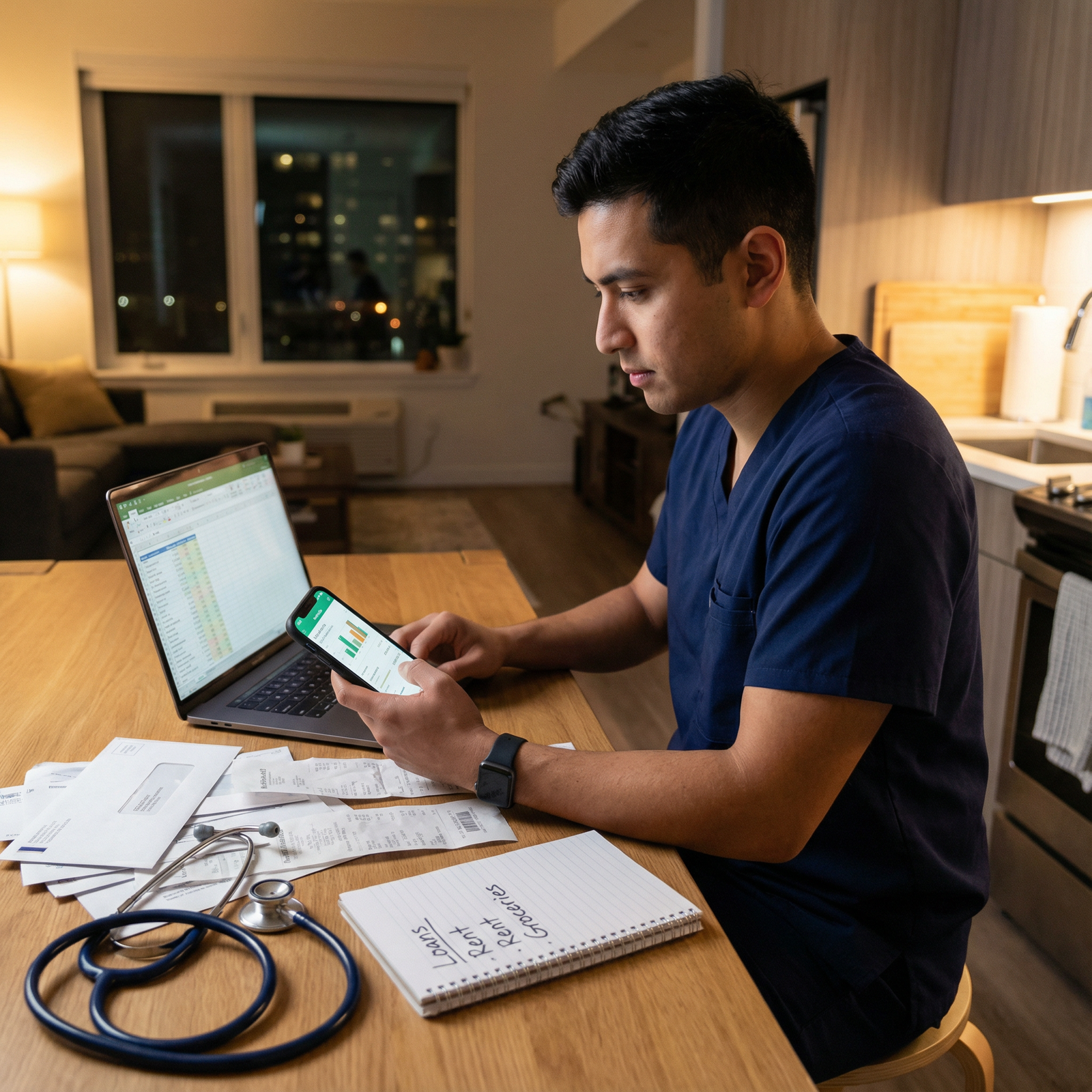
What Residents Actually Do With Their Non-Work Time
Let me be blunt: a lot of residents burn their limited free time on things that make them feel worse, then tell themselves they “have no life.”
Comparison:
- Resident A: post-call, goes home, doom-scrolls, answers non-urgent Epic messages, half-watches Netflix, passes out. Repeats. Feels like life is 100% hospital and couch.
- Resident B: post-call, sleeps 3–4 hours, then meets a friend for a walk and coffee, calls their mom for 10 minutes, preps lunch for tomorrow, reads 10 pages of a book. Still tired. But feels a little like a person.
Same hours worked. Very different sense of “having a life.”
This isn’t about being a productivity robot. It’s about being deliberate with the tiny slices of time the system does give you. Because you won’t get massive blocks. You’ll get scraps. If you passively let those scraps be eaten by charting and scrolling, of course it feels like you have no life.

| Step | Description |
|---|---|
| Step 1 | Scheduled Work |
| Step 2 | Sleep |
| Step 3 | Commute |
| Step 4 | Scrolling TV Random Tasks |
| Step 5 | Relationships Hobbies Exercise |
| Step 6 | Remaining Time |
The question is not “Do you have abundant time?” You don’t. The question is, “Do you use the bits you have intentionally enough to remember you’re more than your pager?”
Program Culture vs Individual Agency: What Actually Matters
Let’s separate two things again: what’s under your control, and what isn’t.
You cannot control:
- Call schedules
- Rotation assignments
- Staffing levels
- Hospital bureaucracy
- Your attending’s mood at 2 a.m.
If your program routinely violates duty hours, retaliates against residents who raise concerns, or runs on chronic understaffing, no amount of yoga will fix that. That’s a systemic problem, not a mindset issue.
But…
You actually do control more than residents think
Even inside a rigid schedule, high-functioning residents quietly do a few things differently. They:
Pre-decide their non-negotiables
One resident I know in IM had two rules:- Friday dinner with partner unless on call
- One gym session sometime between Fri–Sun Non-negotiable. Everything else was negotiable. Not perfect, but it gave shape to the week.
Batch and defend “life admin”
Instead of letting random pages/emails destroy every day off, they:- Picked a one-hour window to deal with bills, emails, scheduling.
- Used template responses.
- Pushed non-urgent work messages to that window unless it was genuinely urgent.
Stop glorifying martyrdom
They didn’t brag about staying two hours late “for the team” every single day while quietly seething. They worked hard, but they didn’t let guilt or image turn every shift into a 16-hour slog.Use co-residents strategically
In healthy programs, residents trade favors:- “Cover my clinic so I can go to my kid’s recital; I’ll cover your post-call on Friday.”
- “I’ll handle these discharges if you pre-round so we both get out near on time.” Broken programs discourage that. Good ones accept it as adult collaboration.
These are not magical solutions. They’re small, unsexy acts of resistance against the “you are only your productivity” lie.
Concrete Ways to Protect a Personal Life Without Tanking Your Training
I’m not going to tell you to “practice self-care” and then walk away. You already know sleep, food, and exercise matter. You’re a doctor. Let’s talk about what actually survives in real residency conditions.
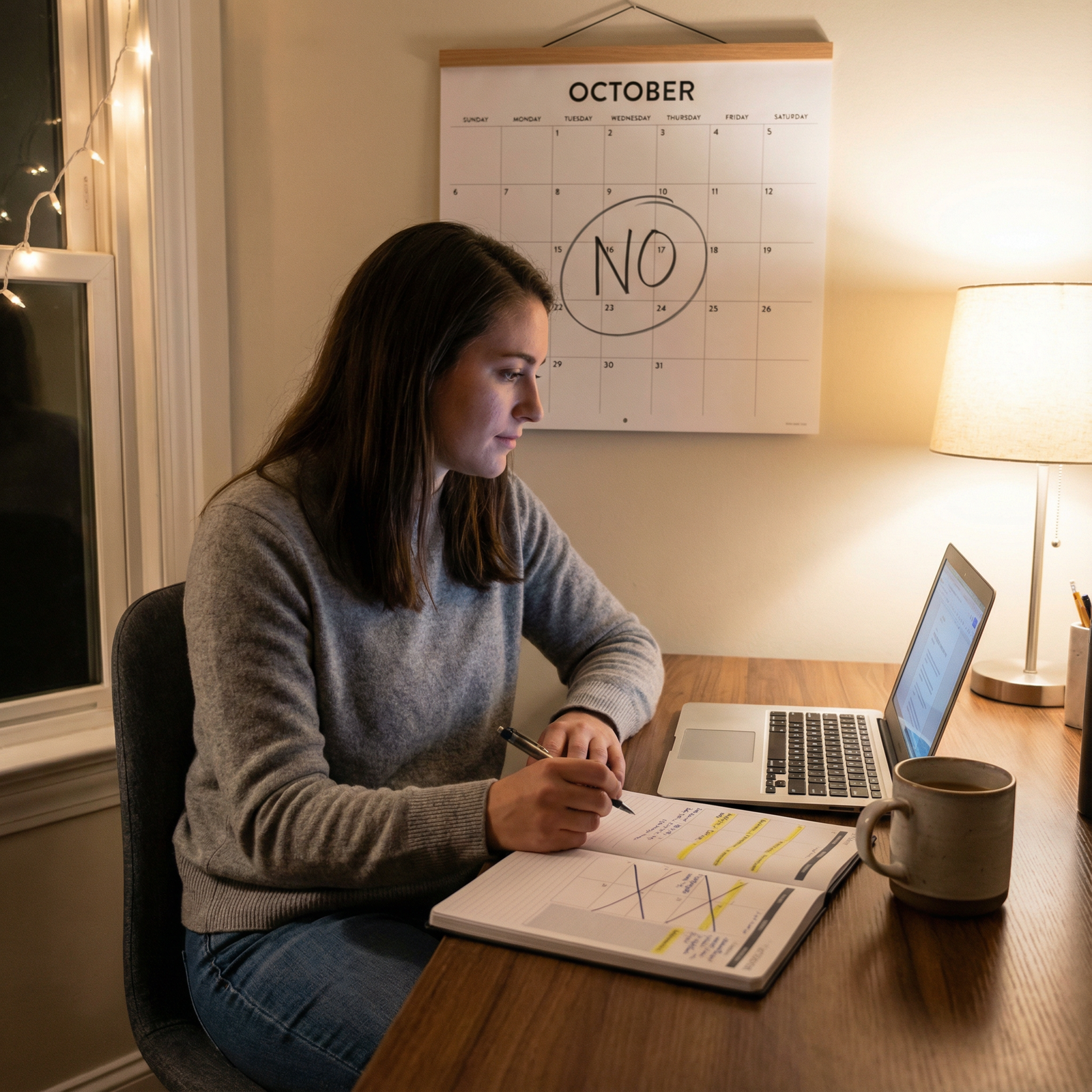
1. Define a “minimum viable life”
You will not have a rich, balanced existence during many stretches of residency. Stop chasing that fantasy. Instead, define your “minimum viable life”:
- 1–2 people you will actively maintain relationships with
- 1 physical habit (walk, gym, yoga, pushups at home)
- 1 non-medical interest that gets any attention (book, game, hobby, religious practice)
Write it down. When the month goes to hell, you’re not asking, “How do I have a life?” You’re asking, “How do I hit the minimum this week?” That shift matters.
2. Use micro-routines, not aspirational routines
People plan 90-minute morning rituals that die on day 2 of ICU.
Instead:
- 5–10 minute blocks tied to things that already happen.
- While coffee brews: text one friend or family member.
- After you park at home: 5-minute walk before going in.
- Before bed: 1 page of a book, not 30.
Not glamorous. But sustainable.
3. Don’t let charting eat your whole life
A gigantic, under-discussed reason residents “have no life” is poor EMR hygiene.
I’ve seen this over and over:
- Spending 45 minutes rewriting H&Ps that could be templated.
- Writing novels in assessments that no one reads.
- Answering non-urgent inbox messages at 10 p.m. from home.
Residents who claw back time:
- Build smart templates and dot phrases.
- Document efficiently during the day, not two hours after sign-out.
- Ask attendings what actually matters in notes and cut the rest.

| Category | Value |
|---|---|
| Inefficient Notes | 4 |
| Moderate Efficiency | 2 |
| High Efficiency | 1 |
That’s approximate average extra hours per week spent charting at home. It adds up.
4. Treat sleep like a clinical priority, not a luxury
You’re not special. You don’t thrive on 4 hours. You’re just accumulating cognitive debt and calling it “dedication.”
Realistically, you won’t hit 8 hours consistently. But you can:
- Protect sleep windows post-call instead of filling them with errands.
- Black out your room. Earplugs. Eye mask. Boring, but effective.
- Stop drinking caffeine after a reasonable hour, even on call.
You’ll enjoy what little “life” you have far more if you’re not half-delirious.
You’re Not Weak for Wanting a Life
There’s a toxic subtext in a lot of residency talk: if you care about your personal life, you’re less serious, less committed, not “hardcore.”
Here’s what the research says instead:
- Physicians with some work–life integration have lower burnout, lower medical error rates, and better patient satisfaction scores.
- Chronic burnout correlates with increased medical errors, worse communication, and higher turnover.
So when someone smugly tells you, “You can sleep or have hobbies once you’re an attending,” what they’re really endorsing is:
- Higher rates of depression
- Higher rates of substance misuse
- More errors and worse care
That is not professionalism. It is negligence dressed up as toughness.
The Big Variable No One Likes to Admit: Choice
Yes, even in residency, you have choices. They’re constrained. They’re ugly sometimes. But they’re there.
Choices like:
- Applying to programs with reputations for not destroying people.
- Prioritizing programs that actually follow duty hours and have real backup systems.
- Saying no to unnecessary “extras” when you’re underwater (the fifth QI project, the committee that meets at 7 p.m. monthly).
- Being honest with your co-residents when you’re at the edge instead of silently absorbing more.
Residents who protect a slice of personal life are not necessarily less busy. They’re more ruthless about where their limited hours go.
And programs that actively encourage this — that model attendings going home, that normalize using vacation, that take coverage seriously — produce better, safer physicians. This isn’t kindness. It’s quality control.
A More Honest Statement About Residency
So let’s rewrite the myth in a way that doesn’t insult your intelligence:
- You will sacrifice a lot in residency.
- You do not have to sacrifice everything.
- If you sacrifice everything, you do not become a better physician. You become a damaged one.
The system will happily take as much of you as you offer. It will not tell you to go home. It will not remind you to see your partner, your parents, your friends. You have to build those reminders yourself and, when possible, find programs that respect them.

Keep three things in your head:
- “No personal life” is not a requirement of residency; it’s a symptom of bad systems and unexamined habits.
- You can’t fix everything, but you can deliberately protect a minimum viable life — a few people, a small routine, one interest — even on brutal rotations.
- Wanting a life does not make you weak or less committed; it makes you more likely to still be standing — and practicing well — ten years from now.

















