The physiology of test anxiety is not “in your head.” It is in your heart rate, your vasculature, your adrenal glands, and your prefrontal cortex getting temporarily hijacked at exactly the wrong time.
Let me break this down specifically: on exam day you are running a carefully choreographed autonomic experiment on yourself. Most students have no idea what pattern their body falls into, and as a result, they try random “relaxation tips” that fight their physiology instead of working with it.
We are going to map what actually happens: the sympathetic and parasympathetic shifts, HPA axis timing, respiratory changes, cerebral perfusion patterns, and how all of this shows up as “blanking out,” overthinking, or panicking halfway through a block.
1. The Autonomic System Is Running Your Exam Before You Do
You are not a rational brain floating in space. You are a brainstem, hypothalamus, and adrenal medulla deciding how much blood and glucose you get to use for that question on nephron transport.
The autonomic nervous system (ANS) has two major arms you need to think about:
- Sympathetic nervous system (SNS): “fight, flight, or freeze”
- Parasympathetic nervous system (PNS): “rest, digest, and consolidate”
On exam day, the game is not “shut off sympathetic and be calm.” That is naïve. The real game is: achieve a high-performance state with:
- Enough sympathetic activation to be alert, fast, focused
- Enough parasympathetic tone to keep fine motor control, working memory, and GI comfort stable
I have watched hundreds of students tank Step/Level exams because they chased total calm. That is wrong. You want controlled arousal, not sedation.

| Category | Value |
|---|---|
| Very Low | 30 |
| Low | 65 |
| Moderate | 100 |
| High | 70 |
| Very High | 25 |
This curve (Yerkes-Dodson) is what your physiology is trying to ride. Too little arousal: you are sleepy, slow, missing simple details. Too much: you are flooded, impulsive, and your cortex goes offline.
2. Exam-Day Timeline: What Your Body Actually Does
You do not have “test anxiety” as a single thing. You have a series of physiological states across the morning. Let’s walk through them like a call schedule.

| Period | Event |
|---|---|
| Pre-arrival - 05 | 30-06 |
| Pre-arrival - 06 | 00-07 |
| Check-in - 07 | 30-08 |
| First Block - 08 | 00-09 |
| Mid-Exam - 10 | 00-12 |
| Late Exam - 13 | 00-15 |
2.1 Early Morning: Cortisol and the “Waking Surge”
Around 5–7 AM, cortisol naturally peaks (the cortisol awakening response). On exam day, this is exaggerated.
Physiology:
- Hypothalamus → CRH
- Pituitary → ACTH
- Adrenal cortex → cortisol surge
Effects:
- Increased gluconeogenesis and mild hyperglycemia
- Increased blood pressure and cardiac output
- Heightened alertness and vigilance
Subjective:
- “I woke up before my alarm with my heart already racing.”
- “I feel wired but not fully awake.”
This is not pathology. This is your system gearing up for “threat + performance.”
If you add:
- Extra caffeine
- No breakfast
- Poor sleep
You convert a useful cortisol peak into jittery tachycardia and GI distress before you even sit.
2.2 Check-in and Sitting Down: Acute Sympathetic Spike
The moment you badge into the testing center, a classic sympathetic pattern hits:
- Locus coeruleus firing → increased norepinephrine in CNS
- Sympathetic preganglionic neurons (T1–L2) → adrenal medulla (ACh → NE/Epi release)
- Increased HR, contractility (β1)
- Peripheral vasoconstriction in skin, splanchnic circulation (α1)
- Bronchodilation (β2)
Subjective symptoms:
- Palpitations, chest tightness
- Cold hands/feet, maybe sweating
- Dry mouth (salivary glands inhibited)
- Urge to pee “one more time”
And cognitively:
- Narrowed spotlight of attention
- Hypervigilance to noises, small changes, proctor movements
This phase is short. Most people settle into a slightly toned-down level 10–20 minutes into the first block. The mistake is interpreting this spike as “I am losing it” instead of “this is the normal SNS ramp-up.”

3. Sympathetic Physiology: The Patterns You Feel as “Anxiety”
Let us get very concrete. Test anxiety is not vague. It is specific receptor-level physiology.
3.1 Cardiovascular Pattern
Sympathetic activation via NE and Epi hitting:
- β1 receptors in the heart → ↑ HR, ↑ contractility
- β2 in skeletal muscle vasculature → vasodilation (direct Epi effect)
- α1 in skin, GI → vasoconstriction
Net effect:
- Higher cardiac output
- Redirected blood flow to skeletal muscle, away from gut and sometimes from prefrontal cortex if systemic vasoconstriction and hypocapnia kick in
If you are prone to high sympathetic responses, exam-day findings:
- Tachycardia 100–120 just sitting
- “Thumping” heartbeat that distracts you
- Lightheadedness if you hyperventilate
And then the cognitive disaster: mild reduction in PFC perfusion + catecholamine flood = impaired working memory and impulse control. Translation: you misread the question, change correct answers to wrong ones, or freeze on questions you normally crush.
3.2 Respiratory Pattern: Overbreathing and CO₂ Drop
Most anxious test-takers subtly overbreathe.
Mechanism:
- Increased respiratory drive from brainstem and cortical influence
- Slight hyperventilation → ↓ PaCO₂ → cerebral vasoconstriction
Result:
- Reduced cerebral blood flow
- Dizziness, tingling fingers, feeling “detached”
- Subjective “my brain is not working, everything is foggy”
This is one of the fastest physiologic ways you sabotage high-level reasoning on an exam. It is not psychological. It is gas exchange.
3.3 GI and Bladder: The Inconvenient Autonomics
Sympathetic outflow + reduced PNS tone:
- Reduced GI motility
- Reduced salivation
- Altered sphincter tone, plus local ENS responses
Phenotypes I keep seeing:
- The diarrhea-and-cramp crowd: often from mixed sympathetic surge + pre-existing IBS + rapid coffee + high-fructose “energy” drinks → frequent urgent bathroom runs.
- The nausea-no-appetite group: stomach feels like a tight knot, cannot tolerate breakfast, then crashes in block 3.
- The pee-every-20-minutes pattern: partly real sympathetic-driven urgency, partly perception/misinterpretation.
None of this is “weakness.” It is predictable autonomic wiring that you can plan around.
4. Brain Circuits: Why You “Blank Out” Under Pressure
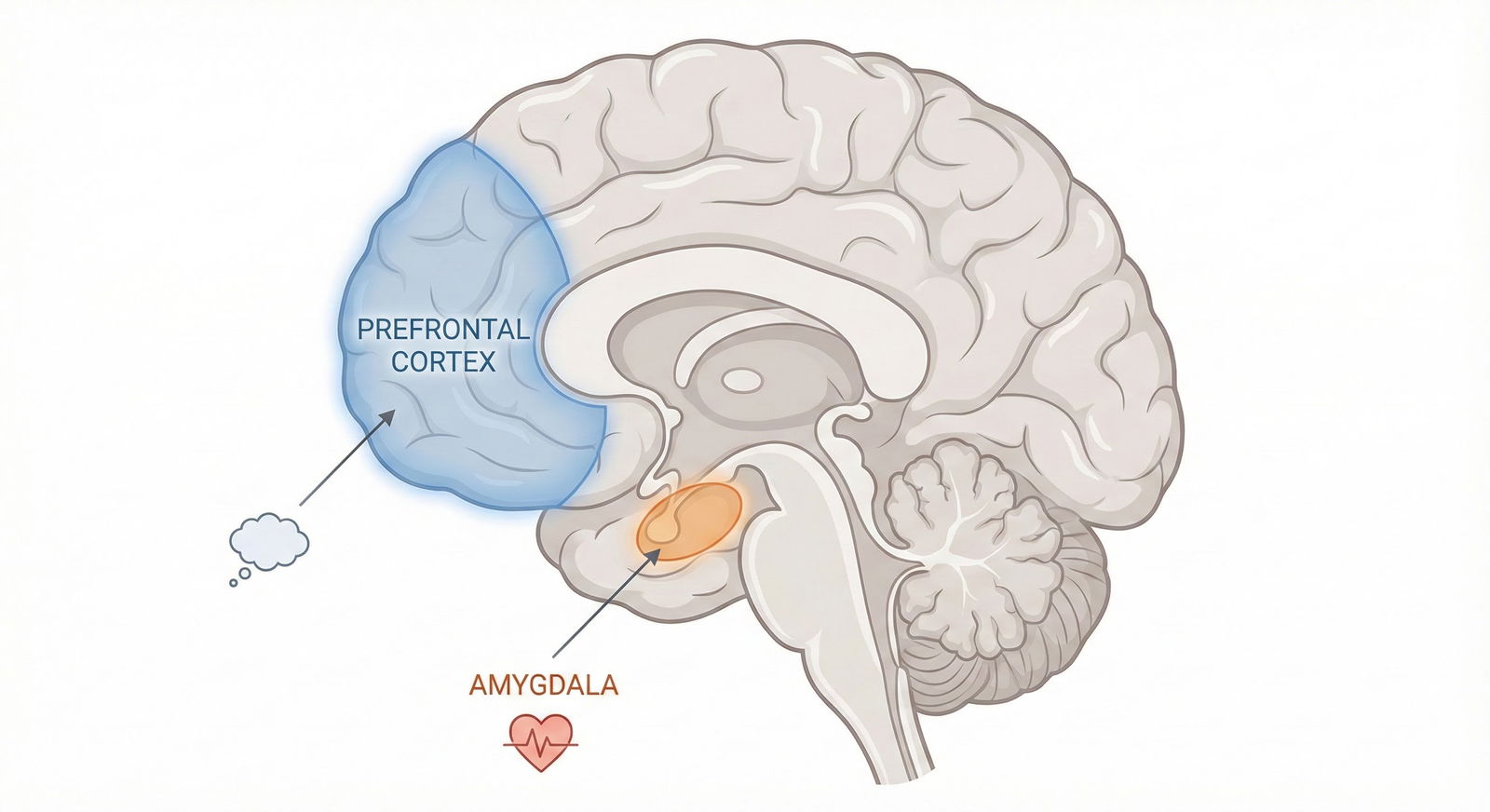
If you want one mental model, use this: exam anxiety is a tug-of-war between prefrontal cortex (PFC) and limbic system under catecholamine and cortisol modulation.
4.1 PFC vs Amygdala
- PFC (especially dorsolateral) → working memory, planning, error monitoring, cognitive flexibility
- Amygdala → threat detection, fear conditioning, emotional salience
In an ideal exam state:
- Moderate catecholamine levels enhance PFC signal-to-noise.
- Amygdala is activated enough to keep you alert, but not dominating.
In test anxiety state:
- Amygdala hyperactivates to “threat of failure, humiliation, residency dreams dying.”
- Stress hormones (NE, Epi, later cortisol) bias processing toward rapid, heuristic decisions and away from slow, analytical reasoning.
Subjective:
- “I know I have seen this, but I literally cannot recall it right now.”
- “My mind went completely blank when I saw that cardiac pharmacology question.”
Objectively, what is happening:
- Acute stress impairs retrieval from declarative memory
- Working memory buffer (holding the question stem, the lab values, the answer options) compresses, then fragments
4.2 Yerkes-Dodson in the Cortex
At low arousal:
- PFC underactivated → boredom, mind-wandering, slower reaction times
At optimal moderate arousal:
- PFC firing patterns sharpen
- Dopamine and NE levels sit in the “goldilocks” zone, enhancing signal transmission
At high arousal:
- Excess NE and DA noise in cortical circuits
- Shift to more limbic-driven, habitual responses
- Decreased top-down control: you know the test strategy but cannot execute it
5. Individual Autonomic “Phenotypes” on Exam Day
Not all test anxiety looks the same. I see three dominant patterns in medical students.
| Pattern | Dominant System | Typical Symptoms | Exam Risk |
|---|---|---|---|
| Hyperadrenergic | Sympathetic | Tachycardia, sweating | Rushing, misreading, impulsivity |
| Vagal/Shutdown | Parasympathetic rebound | Sleepiness, heaviness | Slowness, zoning out, time pressure |
| Mixed/Unstable | Alternating | Waves of panic and fatigue | Inconsistent performance, swings |
5.1 Hyperadrenergic Pattern
Physiology:
- High SNS tone, high circulating catecholamines
- Often paired with low baseline HRV (heart rate variability)
Subjective:
- Restless, cannot sit still
- Racing thoughts, jumping between answer choices
- “I finished with 20 minutes left but my accuracy tanked.”
On vitals (if you could measure mid-exam):
- HR 95–120
- BP mildly elevated
- Resp rate subtly increased
This group overperforms on easy questions (because of speed) and underperforms on difficult integrative questions (because of impulsivity and poor working memory under high arousal).
5.2 Vagal / Shutdown Pattern
This one is less talked about but very real.
Physiology:
- After initial sympathetic spike, strong parasympathetic (vagal) counter-response
- Relative drop in HR and blood pressure
- Often compounded by poor sleep and low glucose
Subjective:
- Brain fog, heavy eyelids, “tired but wired”
- Feeling detached, almost dissociated while reading stems
- Needing to re-read questions 3–4 times
This is the student who says, “I was not panicking. I just could not get my brain to turn on.”
The autonomic picture is more like dorsal-vagal shutdown than classic panic. The system chooses “conserve and freeze” instead of “fight or flee.”
5.3 Mixed / Unstable Pattern
Oscillation between the two:
- Early blocks: hyperadrenergic, overthinking, sweating
- Mid exam: crash, headache, GI upset, brain fog
- Late exam: random second wind or complete cognitive wipeout
This often aligns with erratic sleep, caffeine, sugar use, and high trait anxiety without any structured regulation practice.
6. HPA Axis and Timing: Why You Tank in Block 3 or 4
You know that feeling: blocks 1–2 go fine, then suddenly by block 3:
- You miss straightforward questions
- You feel emotionally raw or nihilistic (“I am failing, so why bother”)
- Your body feels heavy, but your heart still jumps on hard questions
HPA axis physiology explains a lot of this.
6.1 Acute vs Chronic Stress Hormones
- Immediate: NE/Epi from sympathetic nerves and adrenal medulla (seconds to minutes)
- Delayed: Cortisol from adrenal cortex (peaks around 20–40 minutes after stress onset, but in chronic anticipatory stress like exam day, you are already elevated)
Cortisol effects over hours:
- Mobilizes energy (glucose, fatty acids)
- Modulates immune function
- Critically, affects hippocampal and PFC function: at high levels, impairs memory encoding and retrieval
By mid-exam:
- You have had hours of sustained arousal
- Cortisol has been elevated for a prolonged period
- Glucose fluctuations are more pronounced if you did not eat strategically
Subjective mid-exam:
- Reduced cognitive flexibility
- Increased negativity bias (“I am blowing this,” “I always fail at this part”)
- Emotional reactivity to small setbacks
This is not you “losing mental toughness.” This is predictable neuroendocrine fatigue.

| Category | Catecholamines | Cortisol |
|---|---|---|
| Pre-wake | 10 | 20 |
| Wake | 30 | 60 |
| Check-in | 70 | 65 |
| Block 1 | 60 | 70 |
| Block 2 | 55 | 75 |
| Block 3 | 50 | 80 |
| Block 4 | 45 | 78 |
7. Respiratory and Cerebral Blood Flow: The Silent Performance Killer
If you remember nothing else from this article, remember this: your CO₂ level is directly tied to your cerebral blood flow. You overbreathe, you starve your brain.
Mechanism:
- Hyperventilation → ↓ PaCO₂ → respiratory alkalosis
- Cerebral vessels constrict in response to low CO₂
- Result: ↓ cerebral perfusion, especially problematic for areas already under stress (PFC, hippocampus)
Symptoms during an exam:
- Tingling fingers or lips
- Lightheadedness, “floating” sensation
- Tightness in chest even though oxygen saturation is fine
This is why shallow, rapid breathing at the computer terminal is so toxic. You do not feel “out of breath,” so you ignore it. But your brain is running on reduced perfusion right when you need complex pattern recognition.
8. Practical Application: Matching Regulation Strategies to Your Physiology
Now the part most guides skip: applying the physiology. Generic “relax” advice is useless. You need targeted interventions that push you toward the optimal arousal zone for your pattern.
8.1 If You Run Hyperadrenergic
Your problems:
- Excess sympathetic tone
- Hyperventilation
- Cognitive impulsivity
Physiology-based strategies:
Respiratory downshift, not sedation
Use slow, slightly extended exhalation to raise CO₂ back toward normal and stimulate vagal tone, without putting you to sleep.- 4–5 second inhale through nose
- 6–8 second exhale through pursed lips
- 4–6 breaths like this between questions or at flag points (e.g., every 10 questions)
You are not doing a long meditation session. You are making micro-corrections to your blood gases and vagal tone.
Tonic muscle release
Sympathetic hyperactivity shows up as co-contracted muscles: jaw, shoulders, hip flexors.
Brief pattern: on a break or even seated, do:- Clench fists and shoulders for 5 seconds, then release deliberately
- Roll shoulders slowly, exhale as you drop them
This uses reciprocal inhibition to reduce global muscle tone and, through afferent feedback, calms central arousal slightly.
Caffeine and sugar discipline
With an already high catecholamine baseline, front-loading caffeine plus energy drinks is basically malpractice on yourself.- Keep caffeine to your usual or slightly less amount
- Avoid large sugar loads; use slow-release carbs and protein
8.2 If You Run Vagal / Shutdown
Your problems:
- Excess PNS rebound during prolonged stress
- Sleep debt
- Relative hypoglycemia risk
You do not need more “calming” tools. You need controlled sympathetic activation.
Pre-exam activation
Light physical warm-up to raise HR slightly:- 5–10 minutes brisk walk before entering center
- Few rounds of dynamic stretches (leg swings, arm circles)
This primes catecholamine release in a controlled way.
Strategic stimulation during breaks
- Small dose caffeine (if you tolerate it): e.g., half your usual coffee, not a triple espresso
- Light snack combining complex carbs + some protein + small amount of fat (e.g., half a peanut butter sandwich, nuts + fruit)
You are aiming for steady glucose and mild arousal, not jittery spikes.
Posture and breathing
These students often slump, compressing diaphragm, reducing tidal volume.- Sit tall with feet planted, slight anterior pelvic tilt
- Use slightly deeper, but not overly slow, nasal breathing to maintain adequate ventilation and awareness
8.3 If You Are Mixed / Unstable
You need structure more than anything.
Pre-planned micro-breaks in each block
Every 10–12 questions:- Take one deliberate slow breath cycle
- Briefly relax jaw and shoulders
- Gently refocus eyes away from the screen for 2–3 seconds
This prevents both runaway hyperarousal and deep crash.
Tight nutrition and fluid schedule
No surprises. You already know how your body responds because you practiced the exact exam-day routine during full-length practice tests. (If you did not, then that is your assignment.)Cognitive scripting that matches physiology
This is not “positive thinking.” It is giving your amygdala clear, specific expectations.Example internal script:
- “First 10–15 minutes my heart race will be high. That is normal. It settles.”
- “Block 3 I will feel more tired; that is HPA fatigue, not failure. Stick to process.”
This reduces secondary anxiety about the sensations themselves, which otherwise amplifies the physiological cascade.

9. Training the System: Why You Must Rehearse Physiology, Not Just Content
Most medical students only “train” their cortex: UWorld questions, Anki, reading. They show up to the real exam with an untested ANS protocol and then act surprised when physiology runs the show.
You need to train your autonomic response during practice tests:
- Same wake time
- Same caffeine timing and dose
- Same breakfast
- Same scheduled breaks
- Same micro-regulation (breathing, posture, cognitive scripts)
You are conditioning:
- Your baroreflex and HRV patterns to expect this demand
- Your HPA axis to handle sustained arousal without crashing as hard
- Your respiratory control to avoid chronic subtle hyperventilation under stress
Repeated exposure with controlled regulation builds an internal model: “This level of stress is safe and manageable.” That reduces amygdala overactivation on the real day. It is literally fear extinction training.

| Step | Description |
|---|---|
| Step 1 | Full-length practice test |
| Step 2 | Sympathetic activation |
| Step 3 | Apply breathing and posture tools |
| Step 4 | Improved performance state |
| Step 5 | Positive outcome memory |
| Step 6 | Reduced amygdala threat response |
Over 3–5 high-fidelity practice exams, you will notice the physiological spikes get less dramatic and your recovery faster. That is your autonomic system learning.
10. The Clinical Framing: Test Anxiety as a Legitimate Physiological State
You are in medicine. So let us call things by their real names.
Test anxiety is a specific instance of an acute stress response characterized by:
- Sympathetic activation (tachycardia, sweating, GI changes)
- HPA axis activation (cortisol elevation across hours)
- Altered respiratory patterns (often subtle hyperventilation)
- Dynamic shifts in PFC-amygdala balance that impair high-level cognition under high arousal
It is not a character flaw. It is not simply “nerves.” And it is not purely cognitive. This matters because:
- You would never tell a patient with orthostatic hypotension to “just relax and think positive.” You would manage fluids, salt, meds, physical maneuvers.
- Similarly, you should not treat your own exam-day physiology as something to mentally override. You work with it, using the levers you actually have: breathing, posture, muscle tone, nutrition, sleep, stimulant use, exposure practice.

Key Takeaways
Test anxiety is a concrete autonomic pattern, not a vague feeling. Sympathetic tone, HPA axis activation, and respiratory changes directly alter your cognition on exam day.
Different students show different physiologic phenotypes (hyperadrenergic, vagal/shutdown, mixed). Generic “relaxation” advice is useless unless it matches your pattern.
You must rehearse your physiology, not just content. Full-length practice with structured breathing, posture, nutrition, and timing trains your autonomic system to support—not sabotage—your performance when it actually counts.




















