
The worst letters of recommendation strategy for a DO student is the “I’ll just get whoever agrees to write one” approach. That is how you quietly sink an otherwise competitive application.
Let me break this down specifically. For DO applicants, balancing osteopathic and allopathic letter writers is not optional “fine-tuning.” It is core strategy. Programs absolutely make assumptions about you based on who is willing to put their name on the line for you—DO vs MD, specialty vs non-specialty, academic vs community.
You are being read through your letters.
1. What Program Directors Actually Care About (Not What Students Assume)
Most students obsess over the number of letters and miss the actual hierarchy of value.
Here’s the real pecking order for most residency programs when they look at DO applicants’ LORs:
- A strong specialty-specific letter from someone they know or trust (DO or MD).
- A strong specialty-specific letter from an academic faculty member in that specialty.
- A strong letter from a clinical supervisor (IM/Surge/EM/etc.) who clearly worked closely with you.
- A bland, generic letter from a big name.
- A non-clinical letter from research / volunteering / preclinical faculty.
- A character reference from someone outside medicine.
Notice what is not near the top: “Must be DO” or “Must be MD.” Those matter, but only in context.
Program directors are asking three main questions when they read your letters:
- Can this person do the job on Day 1 safely and reliably?
- Is this someone I want to work with at 3 a.m.?
- Does this letter writer actually know this student, or did they spend 2 days together?
Everything else—DO vs MD, name recognition, title—is interpreted through those questions.
Now, where DO vs MD matters is:
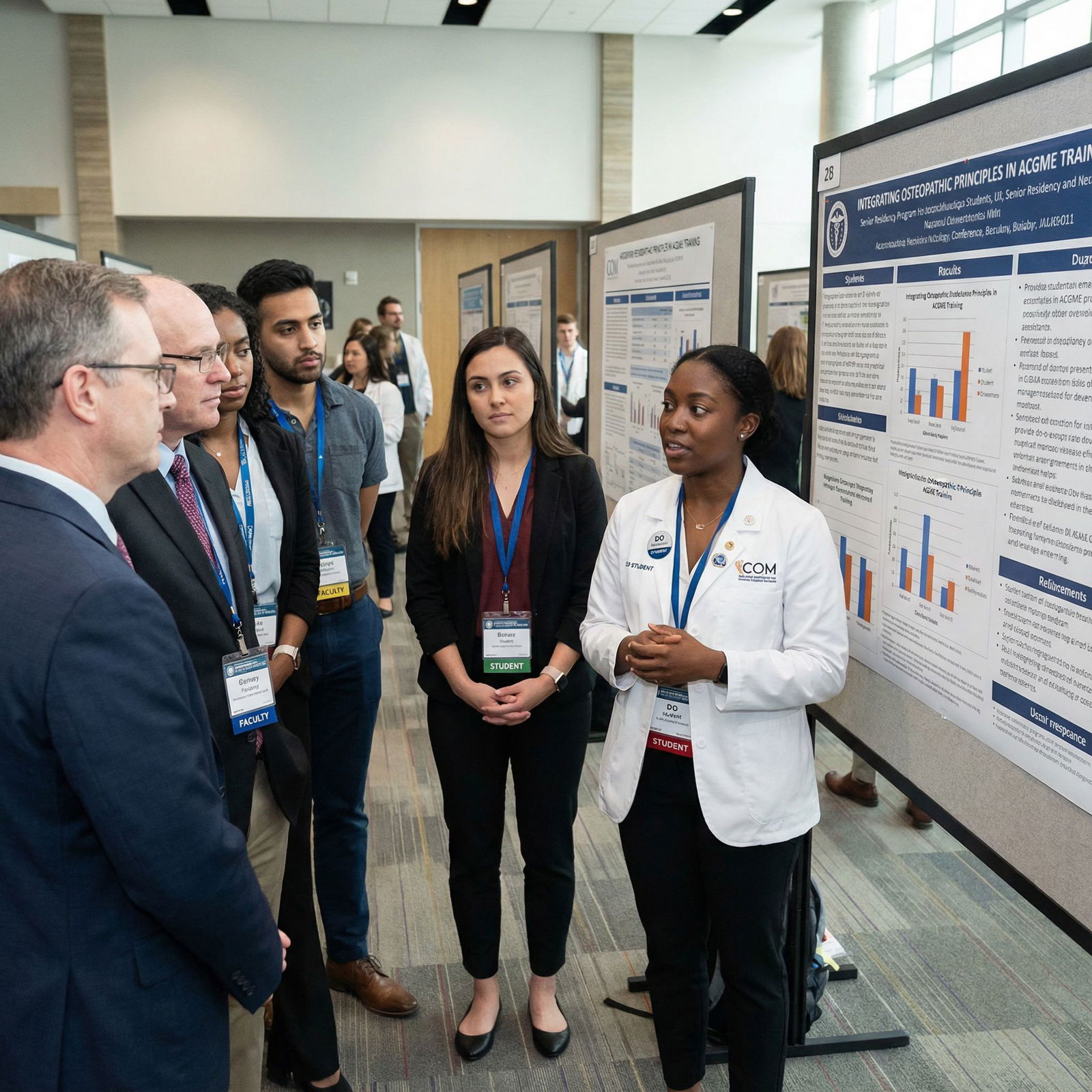
- For ACGME programs assessing whether you can integrate in an allopathic-heavy environment.
- For AOA-heritage / DO-heavy programs looking for evidence that you “get” osteopathic training and culture.
- For some competitive specialties where they want to see you have impressed their type of faculty.
So your strategy is not “how many DO letters” or “how many MD letters.” The strategy is: match the mix of letters to the kind of programs you are targeting, and make sure every letter proves you are a safe, hard-working, teachable resident.
2. How Many DO vs MD Letters: The Actual Ratios That Make Sense
Let me give you the blunt version: for most DO students applying broadly to ACGME programs, a balanced mix is ideal. Extreme all-DO or all-MD portfolios raise questions.
A typical requirement: 3 letters (sometimes 4) + MSPE + Dean’s letter. Many programs specify 1–2 “specialty letters” and leave the others flexible.
Here is a practical breakdown.
| Target Program Type | Specialty Letters (DO vs MD) | Total DO Letters Ideal | Notes |
|---|---|---|---|
| Mostly ACGME, MD-dominant | 1–2 in specialty (at least 1 MD preferred) | 1–2 | Show you function well with MD faculty |
| Mix of DO-heavy and MD programs | 1 in specialty (MD), 1 in specialty (DO) | 1–2 | Balanced portfolio |
| Primarily DO / AOA-heritage | 1–2 in specialty (at least 1 DO strongly fav) | 2–3 | Emphasize osteopathic identity |
| Very competitive specialties (MD) | 2 specialty letters (usually MD) | 0–1 | DO letter is fine as supplemental |
If you want a simple rule-of-thumb for a typical DO student applying to Internal Medicine, Family, Psych, Peds, EM, Anesthesia:
- 3 letters total:
- 1 specialty letter from an MD
- 1 specialty letter from a DO (if possible)
- 1 strong general medicine or sub-specialty letter (DO or MD, whoever knows you best)
What programs do not want to see: three tepid letters from random non-specialty DOs at community sites who barely supervised you. I have watched otherwise decent applications slide down rank lists because the narrative from letters was: “nice, quiet, unremarkable DO student, probably fine.”
The mix is half the story. The strength and specificity of the letters is the rest.
3. Specialty-Specific Nuances: Where DO vs MD Matters More
Not all specialties treat DO vs MD letters the same. Some care a lot about “specialty status,” others care far more that someone actually observed you on busy clinical services.
Let us go system by system.
Primary Care (FM, IM, Peds)
These are the most flexible and forgiving about DO vs MD mix, as long as your letters are clinically grounded and specific.
Ideal setup for Internal Medicine as a DO:
- 1 letter from an IM attending (MD or DO) at a core or sub-internship site, preferably academic.
- 1 letter from another IM or subspecialty (cards, pulm, GI) who saw you on inpatient consults or wards.
- 1 letter from any strong clinical rotation (FM, EM, Peds) who can speak to work ethic and reliability.
For Family Medicine and Peds, similar logic. Programs in community or DO-heavy settings are usually quite pleased to see DO faculty letters. Academic IM programs might slightly favor MD letters, but a strong DO letter from a well-known community preceptor can absolutely carry weight.
Emergency Medicine
EM is its own ecosystem and can be brutal if you ignore the unwritten rules.
- MD vs DO? Less important than SLOEs (Standardized Letters of Evaluation) from EM rotations.
- SLOEs > traditional LORs. If you have two strong SLOEs, you are in the game even as a DO.
Here the real hierarchy is:
- SLOE from an academic EM program where you did an audition rotation (MD or DO faculty).
- SLOE from a community EM site with residency or strong teaching structure.
- Traditional EM letter from an attending who knows you very well.
- Other specialty letters.
Do not waste energy chasing “MD vs DO” in EM if you do not first secure SLOEs.
Surgical Specialties (Gen Surg, Ortho, ENT, etc.)
Now the bias shows up.
- For competitive surgical subspecialties, MD academic letters tend to carry more weight.
- That does not mean DO letters are useless. A DO trauma surgeon or ortho attending who runs a high-volume service and is known locally can write a fantastic letter that helps you a lot.
For a DO student realistically targeting categorical General Surgery:
- 2 surgery letters (ideally MD, but one strong DO surgeon letter is completely acceptable).
- 1 additional letter (ICU, EM, IM) from someone who can talk about your performance on acute, high-responsibility rotations.
If you are reaching for Ortho/ENT/Neurosurg with a DO degree, you do not play the “balanced” game. You play the “who is most respected in this field” game. That often defaults to MD academic faculty. Your DO identity then gets reflected elsewhere (personal statement, CV, OMM involvement) rather than in letter composition.
Psych, Anesthesia, PM&R, Neurology
These are generally moderate in competitiveness and quite DO-friendly overall.
Solid structure for a DO applicant:
- 1–2 specialty letters (MD or DO; DO-heavy programs like at least one DO).
- 1 strong letter from IM/Neuro/EM/FM demonstrating teamwork and reliability.
For PM&R specifically, DO letters can be an asset because of the overlap with OMM, musculoskeletal medicine, and holistic functional focus. But again, strength > degree.
4. ACGME vs DO-Heritage Programs: Who Wants What
You cannot design a good LOR strategy without thinking about your target programs. “I’m applying everywhere” is not a strategy.
ACGME, Historically MD-Dominant Programs
These programs want proof that:
- You can hang in their environment, which has historically trained MD students.
- You have been vetted by MD faculty or academically oriented clinicians.
- Someone in their own training culture has seen you on busy services and still recommends you.
So for these:
- At least one letter from an MD in your chosen specialty is strongly preferred.
- Another letter from an MD in a core field (IM, Surgery, EM) helps.
- You can absolutely include 1 DO letter, especially if it highlights osteopathic aspects that translate well (bedside manner, manipulative skills where relevant, whole-person care).
AOA-Heritage / DO-Dominant Programs
These places know DO training. Many are explicitly proud of it. They often like to see:
- At least one letter from a DO in the specialty, showing you understand and value osteopathic mentorship.
- DO letters that explicitly reference osteopathic principles, if relevant. Not just boilerplate “X is a good student.”
If you send them three letters from MD faculty, it does not tank you, but it undercuts the narrative that you are seeking osteopathic mentorship and community.
Balanced Strategy If You Apply Widely
If you are realistic and applying to both MD-heavy and DO-heavy programs in, say, IM or FM, this is the cleanest approach:
- 1 MD specialty letter (academic if possible).
- 1 DO specialty or core letter.
- 1 strongest overall clinical letter (DO or MD, depending on who knows you best).
That gives programs flexibility: MD programs see that MD faculty trust you; DO programs see that DO mentors also invested in you.

| Category | Value |
|---|---|
| MD specialty letters | 40 |
| DO specialty letters | 30 |
| Other strong clinical letters | 30 |
5. The Real Priority: Who Actually Knows You (And How That Plays Out on Paper)
Here is where DO students mess this up. Many chase “big MD name” letters from attendings who barely know them. Those letters read like this:
“I met Student X for a two-week rotation. They were punctual and professional. Their medical knowledge was appropriate for their level. They will be an asset to any program.”
This is poison. Polite poison, but poison. It says: “I have nothing meaningful to say.”
A lesser-known DO preceptor who ran a busy inpatient service with you for 4 weeks can write:
“On our service at St. Mary’s, we admitted 10–14 patients daily. I directly observed Student X manage high-acuity patients, present succinctly on rounds, and independently follow through on care plans. I trusted them to call consults, discuss sensitive updates with families, and stay late when the department was short-staffed.”
That letter wins. Every single time.
So when you decide between a DO and an MD writer, ask these questions:
- Who supervised me the longest and in the most demanding context?
- Who has seen me handle call / cross-coverage / high volume?
- Who has directly watched my clinical reasoning and professionalism under pressure?
If that person is a DO at a community hospital, fantastic. If it is an MD at an academic site, also fantastic. You want your letters to sound like someone is testifying under oath about your day-to-day behavior.
6. Specific Scenarios: How I’d Advise You to Choose
Let me walk through a few real-world situations I see all the time.
Scenario 1: DO Student, Applying to IM, Rotations Mostly at Community Sites
- IM core with a DO hospitalist at a community site.
- Sub-I at an academic IM program with MD faculty but only 2 weeks.
- FM and EM rotations, both with DO attendings who liked you.
Strategy:
- Letter #1: DO hospitalist from IM core (saw you for 4 weeks, knows your work deeply).
- Letter #2: MD attending from IM sub-I (make sure they actually remember you; ask early, give them a detailed CV and bullet list).
- Letter #3: Strongest between FM and EM DO attendings—the one who can tell concrete stories about you taking ownership.
Result: 2 DO letters, 1 MD letter, but all three are specific, grounded, and trustworthy. That is a very solid IM application.
Scenario 2: DO Student, Applying to EM, One Academic EM Rotation, One Community EM
- 4-week academic EM rotation at a university hospital (MD faculty, SLOE).
- 4-week EM at a community site affiliated with a DO residency (DO faculty, SLOE).
- One IM rotation with a phenomenal DO letter writer.
Strategy:
- SLOE #1: Academic site (MD).
- SLOE #2: DO-affiliated community site (DO).
- Optional 3rd letter: IM DO letter if a program accepts an additional traditional LOR.
Here you are not playing “DO vs MD” games. You are maximizing SLOEs and then using your best non-EM letter as a supplement.
Scenario 3: DO Student, Gunning for General Surgery, Limited Academic Exposure
- 4-week general surgery at a community site (DO surgeon).
- 4-week trauma surgery at a different community site (MD surgeon).
- 4-week ICU with a Pulm/CC MD.
- No big-name academic rotation.
Strategy:
- Letter #1: DO general surgeon who ran your service and can speak to your operative prep, floor work, and work ethic.
- Letter #2: MD trauma surgeon, assuming they can write more than “did fine.”
- Letter #3: MD Pulm/CC from ICU—if they saw you functioning in a high-acuity environment.
Here you end up with 1 DO, 2 MD. But the real win is that all are in high-responsibility settings (OR, trauma, ICU). That matters far more to surgery PDs than which letters have “DO” on the signature line.
7. Timing and Logistics: When and How to Ask (So You Do Not Get Burned)
You can balance your DO/MD mix perfectly on paper and still get sunk by timing and execution.
When to Ask
The best time to request a letter is near the end of the rotation, when you have:
- Had at least 3–4 weeks with the attending.
- Gotten feedback that is clearly positive.
- Shown up consistently, taken ownership, and not faded into the background.
Ask in person if at all possible:
“Dr. Smith, I have really appreciated working with you this month. I am applying to Internal Medicine and I was hoping you might be willing to write me a strong letter of recommendation for residency.”
Watch their response. If there is any hesitation, that is your sign. You need enthusiastic, not reluctant.
Then follow up with:
- Your CV.
- Your personal statement draft (even if rough).
- A bullet list of patients, cases, and situations you were heavily involved in.
- ERAS letter request with clear instructions and deadlines.

| Period | Event |
|---|---|
| Third Year - Core rotations | Ask strong clinical attendings at end |
| Early Fourth Year - Sub-I / Auditions | Secure specialty-specific letters |
| Application Season - ERAS Opens | Ensure all letters uploaded before submission |
Do not wait until August or September to suddenly realize you “need an MD letter.” That is how you end up with a generic note from someone who barely remembers you.
How Many Letters Total vs How Many You Use
You can upload more letters to ERAS than you assign to each program. That is how you finesse the DO/MD balance for different target lists.
For example:
- Total letters uploaded:
- IM DO core letter
- IM MD sub-I letter
- FM DO letter
- EM MD letter (if they know you well)
Then:
- For DO-heavy community IM programs: assign IM DO, IM MD, and FM DO.
- For MD-heavy academic IM programs: assign IM MD, IM DO, and EM MD.
Same pool. Different combinations. Strategically tuned.

| Category | Value |
|---|---|
| Total Letters Collected | 5 |
| Letters Assigned per Program | 3 |
8. Subtle but Important: How Your Osteopathic Identity Shows Up in Letters
There is one more layer here that DO students often ignore. Your letters are one of the few places where your “osteopathic-ness” can show up in a credible way without sounding like brochure copy.
A DO letter writer who actually values osteopathic principles can highlight:
- Your use of structural exams or OMM in appropriate settings (PM&R, FM, sports, inpatient pain).
- Your tendency to see the psychosocial context of disease, not just the labs.
- Your ability to build rapport quickly and handle difficult conversations.
That is not fluff. For many fields—FM, Psych, Peds, PM&R—that is exactly the kind of narrative that distinguishes you positively as a DO applicant.
But it only works if:
- The attending has actually seen you practice this way.
- They can give specific examples, not “X practices holistic care.”
Meanwhile, MD letters often emphasize:
- How you stacked up against MD students.
- Your performance in a conventional, high-volume, guideline-driven environment.
- Your ability to learn and function in the same framework as their usual trainees.
You want both threads in your portfolio: the osteopathic flavor and the “I perform at the same level as MD peers” reassurance. That is the real value of a balanced DO/MD letter mix.
9. Common Mistakes DO Students Make With LOR Strategy
Let me be very direct about the patterns that sink DO letters portfolios every year.
All letters from DOs at small community sites, none from MD faculty.
Reads as: never really tested in MD-dominant or academic environments.All letters from MDs, zero DOs, when applying to DO-heavy programs.
Reads as: ambivalent about osteopathic training or never engaged with DO mentors.Non-specialty letters only for a competitive specialty.
Applying to surgery with zero surgery letters? I have literally seen it. Program directors barely read past that.Letters from preclinical professors instead of clinical supervisors (unless research-heavy field).
A glowing letter from your OMM lab instructor does not outweigh a so-so letter from your IM attending. Clinical > classroom.Generic letters from “famous” faculty instead of specific letters from mid-level attendings.
Name-dropping does not help when the content is bland. A detailed letter from a hospitalist beats a perfunctory letter from the chair.Waiting too long to ask, then scrambling, then accepting anyone who says yes.
That is how you assemble a pile of mediocrity instead of a curated set of advocates.

10. Building a Concrete Plan for Your LOR Mix
Let me force you to make this practical. Here is how I would have you structure your plan if we were sitting in a call and you were a rising M4 DO student.
Step 1: Define your primary specialty target and a realistic backup (if any).
Step 2: List all rotations where you had ≥3 weeks with a single attending and positive feedback.
Step 3: Mark each as DO or MD, and as specialty vs non-specialty.
Step 4: Prioritize:
- Specialty rotations first (regardless of DO/MD).
- Then high-acuity settings (ICU, wards, EM).
- Then others.
Step 5: Decide your target LOR pool:
- Aim for 4–5 total letters collected.
- At least 2 in your specialty.
- At least 1 DO and 1 MD if applying broadly to both MD and DO-heavy programs.
Step 6: Align with program types:
- If mostly ACGME MD programs: make sure at least one MD specialty letter, plus one more MD clinical letter.
- If many DO-heavy programs: make sure 1–2 DO letters, ideally including at least one specialty DO.
Step 7: Ask early, follow up politely, and track uploads. Do not assume “I’ll get to it” from faculty means anything without a timestamped upload in ERAS.

| Category | Value |
|---|---|
| Strong Specialty LORs | 90 |
| Generic Non-specialty LORs | 40 |
Key Takeaways
- The DO vs MD label on your letter writer matters, but only after strength, specificity, and specialty relevance. A detailed DO letter beats a generic MD letter every time.
- For most DO applicants, a mixed portfolio—at least one MD specialty letter and at least one DO clinical letter—signals you can thrive in both osteopathic and allopathic environments.
- Your letters are one of the few places that can show both your osteopathic identity and your ability to perform at the same level as MD peers. Choose writers who actually know you, ask early, and tailor which letters you assign to which programs.




















