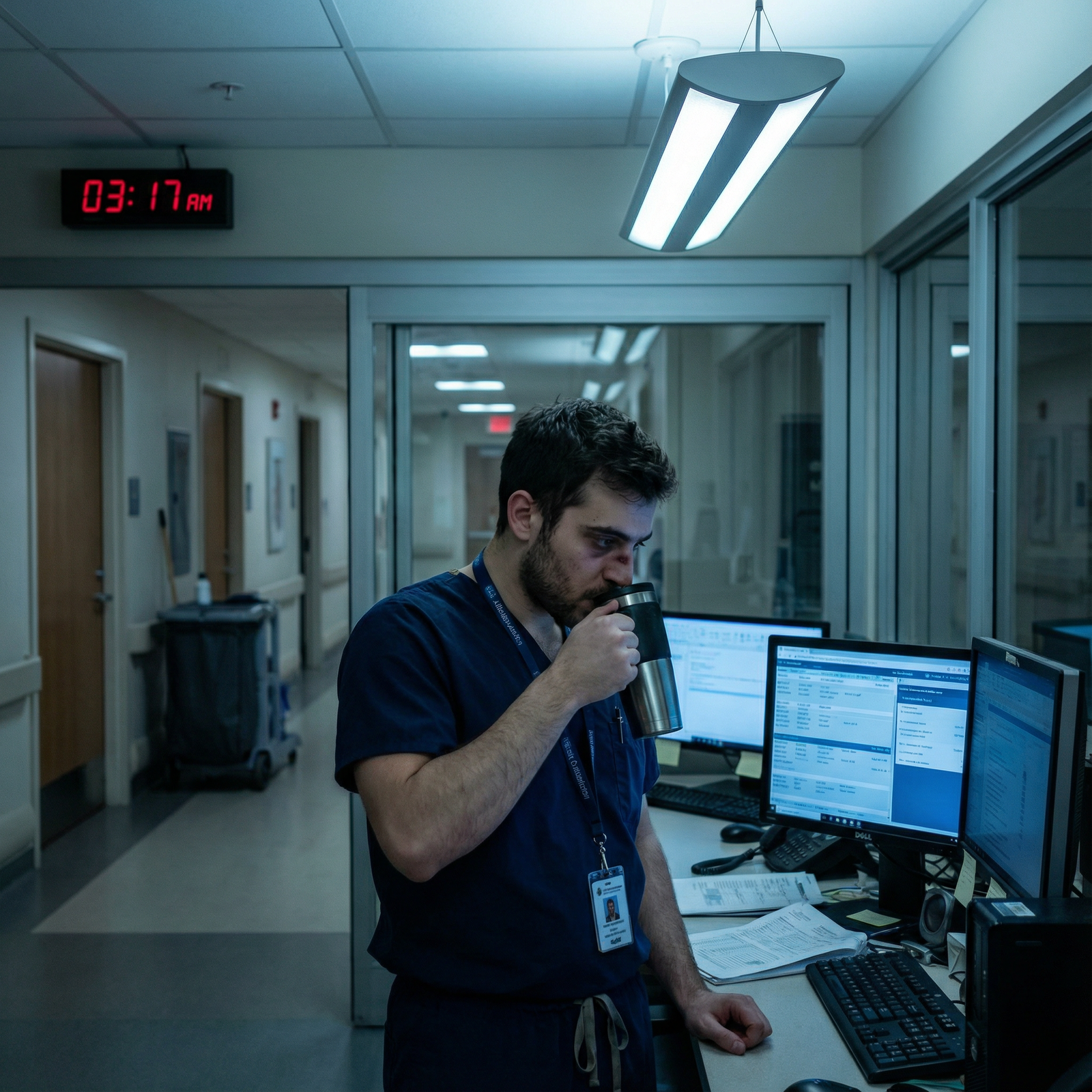
It’s 5:30 a.m. You haven’t even matched yet, but you’re wide awake because your brain is running the same loop:
“I’m going to be on night float. My partner works days. Daycare is 7–6. I’ll be post‑call, half‑dead. Who’s watching the kid? Am I just…not allowed to have children in residency?”
You picture yourself driving home after a 14‑hour night, eyes burning, then trying to “just nap a bit” while a toddler climbs the furniture. You imagine dropping your baby off at daycare in rumpled scrubs, then falling asleep in the parking lot because you’re too exhausted to drive home. And underneath all that: the absolute terror that if you ask about childcare at interviews, programs will judge you as “not committed.”
You’re not overreacting. This stuff breaks people.
Let me walk through what actually happens, how people with kids get through night float, and what the honest trade‑offs look like. Not the Instagram “resident mom boss” version. The real one.
First: You’re Not the Only One Losing Sleep Over This
Every cycle I hear the same quiet, almost-whispered lines from applicants:
- “We want to try for a baby during residency, but I have no idea how we’d survive nights.”
- “My spouse is also in training. Are we insane for even thinking about kids?”
- “Do people actually just leave their kids with…strangers? Overnight?”
You’re imagining being the only person at your program trying to coordinate daycare with a night schedule. That’s almost never true.
Programs almost always have at least a few residents with kids. They made it work in different, sometimes messy, ways:
- The married IM intern whose husband works 9–5 and they patch their lives around a grandmother and a part‑time sitter.
- The single mom OB resident who literally budgets for night nannies only for call months and lives lean the rest of the year.
- The peds resident couple who staggered their training years to avoid both being on nights at the same time as much as possible.
None of them found a perfect situation. But every one of them found a situation. Often at the last possible second, under pressure, with spreadsheets and panic and way too much caffeine.
You’re allowed to be scared. But you’re not facing an unsolved problem.
The Core Problem: Night Float Breaks Normal Childcare
Standard daycare assumes this: “You work roughly 8–5, Monday to Friday.”
Residency night float says: “Cool story. Now you work 7 p.m.–7 a.m., including weekends, and you need to be a semi‑functional human between shifts.”
Those two realities do not line up.
The specific fear most people have is this:
“How do I sleep enough to be safe, parent enough to not feel like a monster, and avoid spending more on childcare than I make as a resident?”
Here’s the uncomfortable truth: during night float with kids, you can’t protect everything at once. You’re going to sacrifice something:
- Money
- Sleep
- Time with your kid
- Time with your partner
- Social life (this one almost always dies first)
The goal isn’t “no sacrifice.” The goal is “no catastrophe.”
The Actual Childcare Solutions People Use (Not Theoretical)
Let’s go through what I’ve actually seen people do. Not fantasy land. Real residents, real programs, real chaos.
1. The Tag‑Team Partner Plan
This is the classic if you have a partner with more “normal” hours.
Rough structure on night float:
- You get home around 8–9 a.m.
- Partner leaves for work around that time.
- Kid is in daycare/school from ~8/9 a.m. to 4–6 p.m.
- You sleep while the kid is at daycare.
- Partner picks up kid, does afternoon/evening routine.
- You either wake around dinner for a bit of family time or sleep straight through until you need to leave again.
Where it breaks: weekends, sick days, school holidays, and the hours between partner leaving and daycare opening.
What people actually do to patch those holes:
- Pay a sitter 6–8 a.m. to cover the “partner gone, daycare not open, resident just got home” window.
- Use in‑laws or a grandparent for morning coverage during night block if they live close.
- Some residents bite the bullet and send the kid to daycare as soon as it opens and pick up as late as allowed, just to stretch sleep time.
Is it perfect? No. But it’s one of the less financially destructive options.
2. The Night Nanny / Overnight Sitter Route
This one scares people: “You expect me to leave my newborn with someone I barely know all night?”
But a lot of residents with infants, especially those doing q4 call or ICU nights, end up here.
How it usually looks:
- You work 7 p.m.–7 a.m.
- Partner either:
- Also works long hours, or
- Is home but cannot safely stay up all night with the baby and then function at work the next day.
- Night nanny or overnight sitter comes 9/10 p.m.–6/7 a.m., handles feeds/changes/soothing.
- You come home, quickly check in, then crash.
It’s insanely expensive. People budget like this:

| Category | Value |
|---|---|
| Daycare Only | 1200 |
| Daycare + Weekend Sitter | 1800 |
| Daycare + Night Nanny (2 weeks/month) | 2600 |
Yeah. That last bar hurts.
How people make it work anyway:
- Use night nanny only for the worst rotations (ICU, night float, q4).
- Live with roommates or family to cut housing costs.
- Take on more debt with the very conscious decision: “This is my survival tax. I’m paying it now so I don’t mentally or physically break.”
I’ve watched residents who refused any help at night end up so sleep‑deprived they were a danger to patients and themselves. White‑knuckling it is not a flex. It’s how you crash your car post‑call.
3. The Extended Family Village
Sometimes the saving grace is a grandmother who unapologetically moves in.
Patterns I’ve seen:
- Grandparent lives with the family for intern year or the first year with a newborn.
- They do the morning shift (5–9 a.m.) so the resident can sleep.
- They sometimes do weekend overnight stints during back‑to‑back calls.
It’s not always a fairytale. You trade money stress for family dynamics stress. Judgment about your hours. Comments like “In my day, doctors had better schedules” or “The baby doesn’t even recognize you.”
But when it works, it can be the difference between meltdown and “barely manageable.”
4. The “Shift Your Sleep” Strategy
This one is more common with older kids (school‑age) and slightly more humane schedules.
Rough version:
- You come home and stay awake for a bit of morning time with your kid.
- You sleep from late morning through the afternoon while they’re at school/daycare.
- You wake up around dinnertime, do bath/bedtime.
- Then you go to work.
So you’re splitting sleep into two chunks and giving your kid a parent both morning and evening.
Big problem: fragmented sleep. You are always tired. Always. I’ve seen people hold it together with this, but only with very stable partners and minimal extra responsibilities.
5. Fellow Residents / Co‑Parents / Group Hacks
Honestly underused but can be powerful:
- Co‑residents with kids occasionally trade coverage (e.g., one covers a weekend morning playdate while the other sleeps).
- In some programs, multiple residents hire the same sitter for overlapping morning shifts after nights to reduce cost.
- Childcare swaps within a trusted group: “You grab my kid Saturday morning so I can sleep after nights, I’ll take yours next month when you’re on nights.”
The catch is obvious: everyone is exhausted and overbooked, so this works best for small, very tight‑knit groups.
What Programs Actually Offer (And How Much It Helps)
You’ve probably seen vague lines on websites like “family-friendly culture” and “support for residents with children.” That could mean anything from “we say congrats when your baby is born” to “we literally have subsidized hospital daycare with flexible hours.”
Here’s the spread I’ve actually seen:
| Support Type | How Helpful It Really Is |
|---|---|
| On-site hospital daycare | Huge for day shifts, limited for nights |
| Backup/sick-day care | Saves you on crisis days |
| Stipend/discount | Helps, but doesn’t fix nights |
| Parenting/leave policies | Good for maternity/paternity, neutral on nights |
| Absolutely nothing | You’re fully on your own |
And here’s the annoying part: many programs do nothing specific for nights. Daycare hours are usually 6 a.m.–6 p.m. That’s great for day floats. Useless from 9 p.m.–3 a.m.
This is where your interview questions matter. You can ask about this without painting a target on your back.
Instead of:
“I plan to have kids. How flexible are you with childcare?”
Try:
“I’ve heard a lot of residents nationally struggle with overnight childcare during night float. How do residents with kids at your program usually handle that? Are there any institutional supports—daycare, backup care, or informal systems?”
You’re not saying “I’m pregnant.” You’re saying “I’m not oblivious to real life.” Good programs respect that.
How People Plan (And Still Feel Behind)
If you’re wired like me, you want a spreadsheet solution now, before you even match.
So here’s roughly how residents who stay mostly sane approach it.
1. They accept that night float is a season, not forever
Night blocks are brutal, but they are blocks. You’re not on nights every month of residency. Some specialties barely use them. Others (IM, EM, surgery) lean hard on them.
They plan like this:
- “For X months a year, our family system has to shift into ‘night mode.’ We will pay more, see each other less, and lower our standards for everything else.”
- “For the other months, we stabilize and recover.”
A lot of the dread you feel now comes from assuming your entire residency will feel like a worst‑case night float month. It won’t.
2. They budget assuming childcare will hurt more than they think
People consistently underestimate costs. Then panic.
The residents who seem calmer do the opposite. They over‑estimate.
They’ll literally write out a rough budget like:
- Base daycare: $X/month
- Extra sitter/night nanny for night float and ICU: another $Y/month averaged over the year
- Emergency padding: some buffer for sick days and gaps
And then they look at that number and decide what to cut elsewhere before they’re in crisis. Not fun. But better than discovering in October of intern year that your checking account is empty and you still have 2 weeks of nights left.
3. They pre‑collect names and backup options
The families who don’t completely implode during a kid fever + night float + partner stuck at work scenario are the ones who already had:
- At least one backup sitter who’d been to the house before.
- A sense of which urgent care clinics are open when.
- A co‑resident they could text to say, “I’m drowning, can you swap this one call?”
You can’t predict every scenario. But you can build a short list of humans and services before you need them. That’s the difference between “total meltdown” and “barely managed disaster” sometimes.
The Emotional Stuff No One Warns You About
This part is the hardest to talk about, because it hits right in the guilt center.
Things residents with kids on night float say to me all the time:
- “I feel like I’m choosing patients over my own child.”
- “My baby reached a milestone and I wasn’t there because I was admitting chest pains.”
- “My wife is basically a single parent when I’m on nights, and I feel useless.”
And from single parents:
- “If I get sick, there is no backup. It’s just me or no one.”
You might be worried that just wanting kids in residency makes you “less serious” about medicine. That’s nonsense. But the guilt is real.
Here’s what I’ve seen help:
- Brutal honesty with your partner about what night blocks will look like. No sugarcoating.
- Lowering the bar for yourself during those months. Messy house, takeout, screen time? Fine. Survival > aesthetics.
- Letting go of this fantasy that “good parents” are physically present for everything. Residents parent in snapshots and weekends and random Tuesdays post‑call. Kids don’t keep score the way your anxious brain does.
I’ve watched kids of residents grow up healthy, attached, clearly loved. Did they have night nannies and daycare and rotating caregivers? Yeah. Were they damaged? No.
You are not doomed to be a bad parent because you’re in training.
A Quick Reality Check on Worst‑Case Scenarios
You’re probably already thinking these, so let’s say them out loud:
“What if my childcare falls through and I’m signed out to 18 patients?”
“What if my kid gets sick the same week I’m on nights and my partner is out of town?”
“What if my program thinks I’m unreliable because I have childcare needs?”
Do disasters happen? Sometimes, yes.
But here’s what usually happens instead:
You scramble. You use sick days, co‑residents, extended family. You cry in stairwells. Your attending grumbles but then tells you about when their kid had RSV. People complain about “coverage,” sure, but they still help.
And over time, your system gets less fragile. You get better at seeing weak points before they explode.
The nightmare scenario where you get fired because your sitter canceled one morning? I haven’t seen that. Poor communication and chronic pattern of no‑shows? Sure. One childcare meltdown in three years? No.
What You Can Do Now (Pre‑Match) Without Losing Your Mind
Since you’re still in the application / pre‑residency phase, your job isn’t to lock in a specific nanny. It’s to stop this problem from feeling like an unknowable black hole.
Concrete stuff you can actually do now:
- During interviews, quietly pay attention to how many residents have kids and whether they seem like ghosts or actual humans.
- Ask residents off‑camera (on pre‑interview socials, second looks, etc.): “Are there people with young kids? How do they handle nights?” They’ll tell you the truth.
- When ranking, give extra weight to places that clearly have at least some institutional support for families. It matters way more than some shiny research line if you’re planning kids.
And privately with yourself and your partner, if you have one:
Talk seriously about timing, money, and what kinds of sacrifices you’re both willing to make. Not in a “maybe everything will magically work out” way. In a “yes, we’re signing up for something very hard, and here’s how we’ll protect ourselves from completely breaking” way.

| Step | Description |
|---|---|
| Step 1 | Leave for Night Shift 6 pm |
| Step 2 | Night Float 7 pm to 7 am |
| Step 3 | Drive Home 7 to 8 am |
| Step 4 | Quick Handoff and Kid to Daycare |
| Step 5 | Sitter or Family Covers Morning |
| Step 6 | Resident Sleeps 9 am to 3 pm |
| Step 7 | Wake Up, Dinner or Brief Family Time |
| Step 8 | Partner Home? |

FAQs
1. Is it completely insane to have a baby during residency if I know I’ll have night float?
Not insane. Hard, yes. The people who do it without totally imploding either have: a reasonably supportive partner or family, a willingness to pay for extra help during the worst months, and a realistic idea that those night blocks will be ugly but temporary. If you expect it to feel balanced or “normal,” you’ll be miserable. If you treat night float with a baby as a short, intense season you plan around—financially and emotionally—it can be survivable.
2. Will programs judge me if I ask about childcare or mention I want kids?
If you phrase it as “I’m curious how residents with families are supported,” most decent programs will not penalize you. They know residents are adults with lives. If a place visibly bristles at that question or clearly has zero support and no residents with kids, that’s useful data for you. You don’t want to spend three to seven years in a place that thinks your family makes you a liability.
3. What if I can’t afford a night nanny or extra sitters on a resident salary?
Then you lean harder on lower‑cost options: tag‑teaming with a partner, using extended family if that’s an option, maximizing standard daycare hours, sharing sitters with other residents to cut costs, and reserving any paid overnight help for truly dangerous moments (like when you’re in the ICU and have back‑to‑back nights). A lot of residents live very bare‑bones during those years to make childcare work. It’s not glamorous, but it’s temporary.
4. How much sleep do resident parents on night float actually get?
Honestly? Often less than ideal, but usually enough to function—barely—if the system is set up decently. A fairly “good” setup might give you 6–7 hours during the day while the kid is in daycare and someone else handles mornings and evenings. A bad setup (no help, toddler at home, partner also gone) can drop you to 3–4 hours, which is unsafe. The whole point of planning is to avoid living in that unsafe range for weeks at a time.
If you remember anything, let it be this:
You’re not weird for panicking about childcare and night float. People with kids get through it with imperfect, patchwork systems—some expensive, some exhausting, all a little messy. Your job isn’t to create a perfect plan now. It’s to choose a program that won’t make this harder than it has to be, accept that certain months will be survival mode, and line up just enough support that you’re tired, not broken.



















