
The biggest lie about residency nights is that it “gets easier.”
It doesn’t. It just gets different. Your responsibility, risk, and mental load scale up every year.
I’m going to walk you through it like it actually plays out: PGY-1, PGY-2, PGY-3. Month by month, then zooming into what a single night looks like at each level. So you know what’s coming and what you should be able to handle at each step.
Big Picture: How Night Responsibilities Shift From PGY-1 to PGY-3
At this point, you need a birds-eye view before we drill into the timeline.

| Category | Value |
|---|---|
| PGY-1 | 30 |
| PGY-2 | 65 |
| PGY-3 | 90 |
PGY-1 nights:
- Task-heavy, protocol-driven, low autonomy
- You’re the orders, the cross-cover, the “can you write for Tylenol?” person
- You call seniors for anything that feels even slightly off
PGY-2 nights:
- You’re the stabilizer and triage lead on many services
- You field calls from PGY-1s, handle sicker patients, run more codes
- You start to feel the weight of “if I miss this, bad things happen”
PGY-3 nights:
- You are the overnight adult in the room
- You supervise, make disposition calls, run resus, negotiate with consultants
- You shape the night for everyone else
Now let’s break it down chronologically.
PGY-1: Survival Mode and Learning the Floor (Months 1–12)
Months 1–3: Orientation Nights and Controlled Chaos
At this point, your job is simple: do what you’re told, and don’t miss the obvious.
Typical responsibilities:
- Cross-cover 20–60 patients on a general medicine or surgery service
- Put in orders for:
- PRNs, fluids, electrolyte repletion
- Pain, nausea, sleep meds
- See new issues:
- Chest pain, shortness of breath, fevers, confusion, falls, low urine output
- Call your senior for:
- Any potential transfer to ICU
- New oxygen requirement or change in mental status
- Anything that “feels bad” even if you cannot say why
Night flow in this phase usually looks like:
Sign-out (6–7 pm)
- Someone rapid-fires at you: “Room 612 is DNR/I, very fragile; 718 has soft pressures but stable; 730 is agitated; here are four to-do’s.”
- At this point you should:
- Write everything down, obsessively
- Clarify code status on every sick patient
- Ask: “Who are you actually worried about tonight?”
7 pm–11 pm: Pager Hell
- You’re getting:
- “Pt c/o 10/10 pain, can we get more?”
- “Temp 38.6, do you want Tylenol or workup?”
- “This patient’s BP is 88/54, HR 120, on 4L NC now.”
- At this point you should:
- See hypotension, hypoxia, or acute mental status changes in person
- Start learning which vitals you can watch vs which require immediate action
- Call your senior early. They’d rather hear a false alarm than code blue
- You’re getting:
11 pm–3 am: Admission + Cross-cover Balance
- You might have 1–3 admissions depending on the service.
- Your job: histories, focused exams, initial orders.
- Your senior might see the patient after you, or just staff over the phone.
- At this point you should:
- Use admission templates/checklists so you don’t forget DVT ppx, code status, home meds
- Call your senior with:
- A one-liner
- A differential with at least 2–3 real possibilities
- A proposed plan (even if it’s bad, it shows you’re thinking)
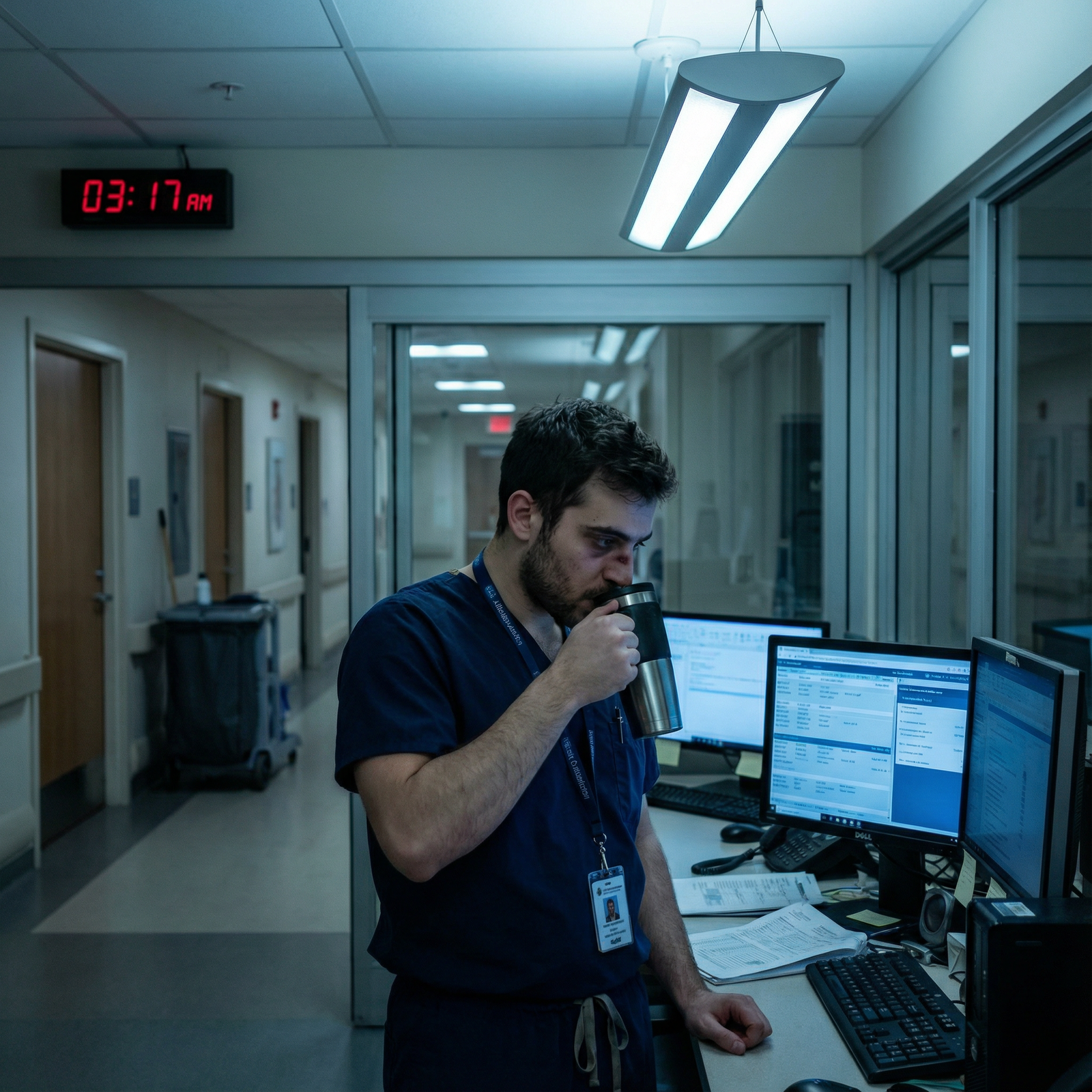
3 am–7 am: The “watch them not die” window
- This is when things either stay stable or unravel.
- You’re exhausted, which is exactly when weird arrhythmias and septic shock show up.
- At this point you should:
- Re-check anyone who was borderline earlier in the night
- Pre-round lightly on the sickest ones; know their overnight story cold for the day team
- Start simple sign-out notes for each patient seen overnight
Months 4–6: Competent Cross-cover, Early Pattern Recognition
By now, you shouldn’t be calling your senior for simple stuff:
- Potassium 3.2? You know the replacement protocol.
- Afebrile for 24 hours with stable vitals? You’re not repeating blood cultures just because.
- Mild agitation in known dementia? You can manage non-pharm first, then low-dose meds if needed.
At this point you should:
- Handle:
- Routine fevers with a clear source
- Mild hypotension that responds to fluids
- Basic arrhythmias like AF with RVR in a stable patient (with guidance at first, then solo)
- Escalate:
- Any unclear deterioration (“I have a bad feeling”)
- Anyone needing pressors, non-rebreather, or BiPAP for the first time
- New focal neuro deficits, possible strokes
This is where you start learning the hidden curriculum:
- Which nurses will call you early vs late
- Which attendings will grill you on 7 am sign-out if you did not document properly
- How to chart just enough at night without drowning
Months 7–12: You Know the System, Still Not in Charge
By late PGY-1:
- You’re faster at admissions
- You can sense septic vs not-septic from the doorway
- You know which consults you can push back on and which you should call immediately
At this point you should:
- Be independently:
- Writing full admission orders without needing your senior to adjust everything
- Starting antibiotics appropriately for common problems (PNA, UTI, cellulitis)
- Running the first few minutes of a code (compressions, airway, first meds) until backup arrives
- Still be:
- Calling for major decisions—ICU transfers, code status changes, complex end-of-life issues
Key PGY-1 night survival moves by this stage:
- Pre-charting: glancing at all cross-cover patients at the start of your shift
- Grouping tasks by floor so you are not walking the length of the hospital 40 times
- Knowing your personal “danger signs”: when you’re too tired to think straight and need to pause before ordering something risky
PGY-2: From Task-Doer to Night Stabilizer (Months 13–24)
Year 2 is where the real pressure shows up. Same building. Completely different mental game.
Months 13–18: First Months Being the “Senior on Nights”
At this point you might:
- Be the primary night senior for:
- A medicine service
- A surgery team
- An ICU or step-down unit (depending on program structure)
- Field calls from:
- PGY-1s on cross-cover
- Nurses on step-down units
- ED about admissions and potential ICU needs
Your responsibilities now:
- Supervise:
- Every new admission (at least by chart review and phone, often in person for sick patients)
- PGY-1 decisions about hemodynamics, oxygen changes, and transfers
- Triage:
- Who needs you right now vs who can safely wait
- Which ED patient gets the last floor bed vs ICU consult
- Run:
- Rapid responses
- Many of the codes in your building until an attending appears
Night flow for a PGY-2 senior:
Sign-out (6–7 pm)
- You’re now listening for global risk:
- “These three might decompensate. Watch them.”
- At this point you should:
- Ask: “If something goes wrong with this patient, what would you do?”
- Mentally pre-rank which patients you’ll personally eyeball before midnight
- You’re now listening for global risk:
Early Shift (7–11 pm): Teaching + Oversight
- PGY-1 calls: “I got paged for a BP 88/52, HR 110.”
- At this point you should:
- Ask for a structured presentation: one-liner, vitals, exam, labs
- Decide: phone guidance vs “I’ll come see with you”
- Teach 1–2 points each time: “Next time, always check lactate early in someone like this.”
Midnight Zone (11 pm–3 am): The Bottleneck
- Multiple things hit at once:
- Two admissions from the ED
- A rapid response on 7 East
- A cross-cover hypotension on 5 West
- This is your real test.
- At this point you should:
- Use very explicit triage:
- Sickest airway/breathing/circulation issues first
- Send PGY-1 to “simple but time-sensitive” stuff (pain, nausea, basic workups)
- Communicate:
- “You go see 7 East rapid, I’ll handle ED admit that looks like sepsis. Call me from bedside.”
- Use very explicit triage:
- Multiple things hit at once:
Late Shift (3–7 am): Anticipation + Cleanup
- You’re making sure no one is circling the drain at 6:45 am when day teams show up.
- At this point you should:
- Reassess anyone:
- Started on pressors
- On new BiPAP
- Whose vitals were borderline earlier
- Confirm that all critical events are documented and sign-out is coherent
- Reassess anyone:

| Period | Event |
|---|---|
| PGY-1 - Month 1-3 | Learn basics, constant supervision |
| PGY-1 - Month 4-6 | Manage routine issues, call for sick patients |
| PGY-1 - Month 7-12 | Faster cross-cover, early autonomy |
| PGY-2 - Month 13-18 | First senior nights, triage, supervise interns |
| PGY-2 - Month 19-24 | Run rapid responses, lead codes, disposition decisions |
| PGY-3 - Month 25-30 | Full senior role, oversee multiple teams |
| PGY-3 - Month 31-36 | Act as attending-lite, system-level thinking |
Months 19–24: Comfortable Senior, Real Accountability
By late PGY-2, you should:
- Be comfortable:
- Running ACLS without freezing
- Calling for ICU transfer without needing someone to hold your hand
- Saying “No, this patient can go to the floor” and backing it up with facts
- Be increasingly good at:
- Knowing when not to over-test at 3 am
- Giving PGY-1s appropriate autonomy while keeping them safe
At this point you should:
- Transition from “I’ll see everything” to:
- “You see the stable chest pain; I’ll see the hypotensive GI bleeder.”
- Start acting like a shield:
- You absorb the stress, not your intern
- When things get ugly, the buck stops with you first, not them
You also start dealing more with:
- Angry families at 2 am asking “Why hasn’t anything been done?”
- Surgeons or consultants who say “Call back in the morning” for something you know is urgent
- Hospital politics: bed control, ICU capacity, ED congestion
PGY-3: Night Shift Field General (Months 25–36)
Senior year nights are where you stop thinking like “my patient list” and start thinking “the whole hospital ecosystem.”
Months 25–30: Full Senior, Limited Supervision
At this point, attendings are often at home, available by phone. You are the in-house decision-maker.
Your responsibilities now:
- Oversee:
- Multiple interns and possibly PGY-2s across one or more services
- All new admissions to your department overnight
- Lead:
- Every code on your floors until attending arrives
- Difficult end-of-life and goals-of-care conversations that cannot wait
- Coordinate:
- ICU vs floor placement
- Step-down upgrades
- Transfers from outside hospitals arriving at 2 am
Night flow as a PGY-3:
Pre-Shift (5:30–7 pm): Strategic Setup
- At this point you should:
- Review sickest patients yourself during or right after sign-out
- Ask the day senior: “Who is likely to blow up tonight?”
- Meet interns:
- Set expectations: “Call me for X, Y, Z. I don’t care what time.”
- At this point you should:
7 pm–11 pm: Proactive Senioring
- You’re:
- Filtering consultant recommendations for interns
- Adjusting plans that are clearly not going to work overnight (e.g., complex procedures scheduled at 2 am for no reason)
- At this point you should:
- Push teaching on the fly:
- “Walk me through your plan before you call GI.”
- “Tell me why you chose this antibiotic.”
- Protect sleep:
- For yourself a little
- But especially for your more junior residents by heading off some nonsense pages
- Push teaching on the fly:
- You’re:
11 pm–3 am: High-Stakes Decision Window
This is when the true PGY-3 role crystallizes:
- ICU attending asks: “Do you really think this patient needs us?”
- ED: “We’ve got three for you, one might be septic, one is chest pain, one is social admit.”
- Intern: “I’m with a crashing patient already, but I’m getting paged about another hypotension.”
At this point you should:
- Make fast, defensible decisions:
- Who needs ICU
- Who can wait in ED
- Who can safely stay on the floor with clear parameters
- Deploy your team:
- “You stay with the crashing patient; I’ll evaluate the new hypotension and call you if I need you.”
- Communicate clearly:
- With nurses: “If MAP stays under 60 after this bolus, call me immediately.”
- With ED: “This patient is floor-appropriate with tele, I’ve reviewed the chart and labs.”

Months 31–36: Attending-Lite, System-Level Thinking
Final year nights, you’re not just taking care of patients. You’re shaping how the night runs.
By now you should:
- Anticipate system failures:
- Know which services are chronically understaffed at night
- Pre-plan: “ICU is full; we need a contingency plan for decompensating floors patients.”
- Mentor intentionally:
- Let PGY-1s make low-risk mistakes (ordering the wrong fluid rate, then you correct it and explain why)
- Debrief tough cases: “Let’s talk about that code. What would you do differently next time?”
- Model calm:
- Even when everything is on fire, you sound steady on the phone
- You never transmit panic to the team
At this point you should:
- Be the one saying:
- “This patient is not safe for the floor; I will call the attending and advocate for ICU.”
- “We need to talk to this family tonight, not in the morning. Things are changing quickly.”
- Own the big calls:
- Stopping resuscitation efforts
- Overriding a consultant who’s clearly under-calling the severity of illness
- Balancing risk vs benefit of middle-of-the-night imaging and procedures
How the Night Shift Skillset Evolves Year by Year
Here’s the progression in a more structured way.
| Domain | PGY-1 | PGY-2 | PGY-3 |
|---|---|---|---|
| Primary Role | Task-doer, cross-cover | Stabilizer, triage lead | Field general, de facto in-house leader |
| Autonomy Level | Low–moderate | Moderate–high | High (with attending backup) |
| Codes/RRTs | Participates, basic ACLS | Runs many, calls for help | Leads, teaches, makes stop/go decisions |
| Admissions | Data gathering, initial orders | Co-manages, refines plans | Final call on level of care and disposition |
| Teaching | Learner | Teaches interns 1:1 | Teaches team, shapes culture |
| Systems Decisions | None/minimal | Bed flow within service | Cross-service and hospital-wide thinking |
What You Should Be Able To Do At Each Stage (Checklist Style)
By End of PGY-1 Nights, You Should:
- Recognize:
- Sepsis vs “infected but stable”
- Real chest pain vs clearly non-cardiac
- Delirium vs baseline dementia
- Manage independently:
- Uncomplicated fevers, mild hypotension, basic electrolyte issues
- Simple pain and nausea regimens without over-sedating patients
- Know when to escalate:
- Any second dose of fluid for hypotension
- New oxygen requirement above nasal cannula
- Any patient who just “looks wrong”
By End of PGY-2 Nights, You Should:
- Run:
- Most rapid responses smoothly
- ACLS algorithms without needing a cheat sheet
- Triage:
- Multiple simultaneous issues without freezing
- Which pages your intern handles vs you handle
- Decide:
- Floor vs step-down vs ICU and defend it
- Which issues absolutely must be fixed overnight vs can wait for day team
By End of PGY-3 Nights, You Should:
- Lead:
- The entire night operation for your service
- Codes, complex family discussions, consultant conflicts
- Think:
- One step ahead for the whole hospital, not just your list
- About downstream consequences of your choices (ICU capacity, bed flow, imaging backlog)
- Leave:
- Clear, concise sign-outs that set the day team up to succeed
- A culture where juniors felt supported, not abandoned
Final Takeaways
- Responsibility doesn’t just “increase” from PGY-1 to PGY-3; it changes shape—from tasks to triage to true leadership.
- At each stage, your goal isn’t to act like the level above you; it’s to fully own the level you’re at and be ready for the next one.
- The residents who thrive on nights are the ones who call early as PGY-1s, triage ruthlessly as PGY-2s, and protect their teams while making hard calls as PGY-3s.



















