Last month, a second-year resident stumbled into sign-out at 7:15 a.m., hair a mess, eyes red, mumbling, “Crazy night.” The attending nodded, said nothing, then caught my eye and quietly opened the chart. Ten minutes later he turned to me and said, “That was not a crazy night. That was a disorganized one.”
That’s the part no one tells you: attendings judge your night float performance very differently than your day-team heroics. And a lot of it never gets said to your face.
You want the unfiltered version, so let’s get into it.
What Night Float Really Is (From the Attending Side)
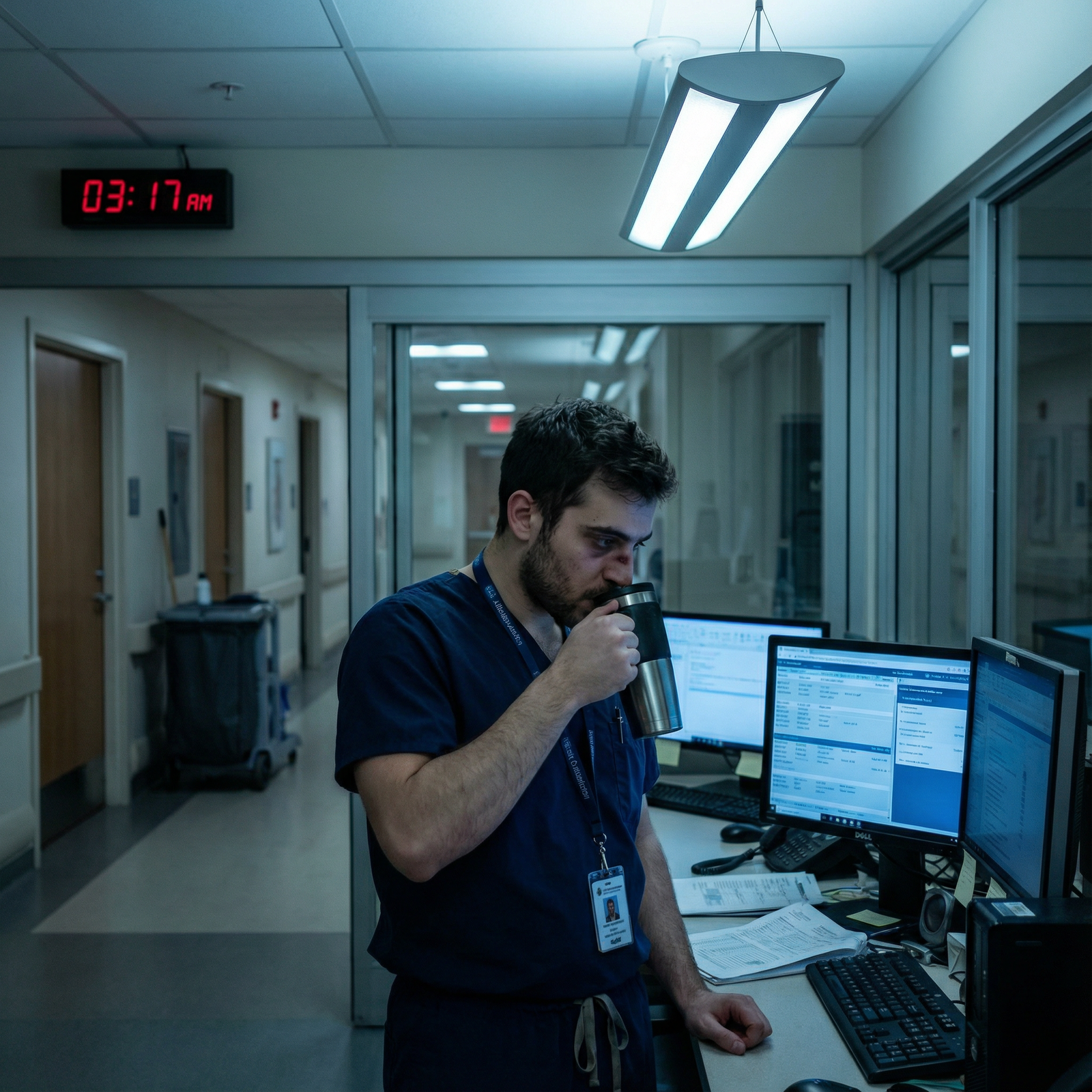
On paper, night float is “cross-coverage and admissions.” On the attending’s side, it’s something else: it’s a stress test of whether you can practice safely when no one is watching.
During the day, attendings see you. They watch you present, examine patients, talk to families. At night, they see footprints: orders, notes, pages answered (or not), the timing of decisions, how the list looks at 6:30 a.m.
When we log in at 5 or 6 a.m., we’re not just “catching up.” We’re silently grading you.
We’re looking at:
- What changed overnight and how you responded
- Which problems you ignored because they were “annoying” rather than critical
- Whether the unit felt calmer or more chaotic after you came on
Nobody says this outright because night float is “just a rotation.” But I’ve watched more than one resident’s reputation get made—or quietly destroyed—based almost entirely on how they handled nights.
The First Thing Attendings Check in the Morning
Let me tell you what really happens between 5 and 6:30 a.m. while you’re frantically pre-rounding or finishing that last cross-cover admission.
Most attendings log in from home or the office and do the exact same sequence, even if they don’t admit it.

| Step | Description |
|---|---|
| Step 1 | Log into EMR |
| Step 2 | Check overnight event log |
| Step 3 | Scan vitals and rapid response calls |
| Step 4 | Review admissions list |
| Step 5 | Open orders and notes |
| Step 6 | Form opinion of night coverage |
First: event log. Any RRTs, codes, transfers to ICU. We look at the timestamp, who was on, and what actually happened—was there early recognition or a delayed scramble.
Then: vitals trending. Did someone sit hypotensive for 3 hours at 80/50 with no fluids, no med changes, no note? That tells us everything we need to know about how closely you’re really paying attention.
Then we look at admissions. Not the notes first—the orders.
Did you:
- Start the right antibiotics before the CT came back?
- Put in fluids for the sepsis admission or just order “NS 100 mL/hr” and walk away?
- Get troponins and EKGs on the chest pain?
- Actually reorder home meds before the 6 a.m. nursing call storm?
If the orders make sense, we relax. If we’re seeing Swiss cheese, we start hunting for patterns.
No one will say, “I spent 30 minutes this morning figuring out whether you know what the hell you’re doing.” But that’s exactly what’s happening.
What They Really Notice About Your Clinical Judgment
On nights, your clinical judgment is distilled. No attending at the bedside, no team huddle, no consultant holding your hand. Just your brain, the nurse, and a blinking pager.
Here’s what we silently scrutinize.
1. Who You Overcall vs Undercall
Attendings won’t fault you for calling too much during your first few nights. They might grumble, but they won’t kill you for it.
What they actually pay attention to is pattern:
- You call for every stable fever of 38.1 but do not call for a BP of 78/40 that’s new.
- You call for a sodium of 129 at 2 a.m. but not for a new oxygen requirement from 2 to 6 L.
We see that and think: this person doesn’t understand what’s actually dangerous.
If you consistently escalate on real issues—hypotension, respiratory distress, altered mental status, GI bleeds, chest pain with concerning features—and handle low-level noise yourself, you build trust fast.
If you escalate nonsense and sit on danger, we stop trusting you. Even if no one says those exact words.
2. Time to Action, Not Just Action
Everyone focuses on “I ordered the CT,” “I started the antibiotic,” “I called the ICU.” Fine. But we look at time stamps.
You got paged at 1:20 a.m. about a patient “a little more short of breath.”
You saw them at 3:05 a.m.
You called us at 3:20 a.m.
They transferred to ICU at 4:00 a.m.
By morning, the nurse note shows they were tachypneic and hypoxic at 1:20 with clear vitals recorded. We will never say it in those words—but that delay gets stored in our heads.
We remember who moves when the pager goes off and who just keeps “finishing this one note.”
3. Your Threshold for Diagnostics
Another thing we notice: who uses tests to cover fear and who uses them to clarify risk.
Night float residents who spray CTAs, CT abdomens, and troponins on everyone send a message: I do not know how to think through probabilities, so I’m ordering the menu.
The ones who write, “Low suspicion for PE given Wells 0, no tachycardia, no hypoxia; will not pursue imaging tonight, strict return precautions, re-eval in a.m.”—those stand out. That tells us you are thinking, not just clicking.
Same with labs: adding a lactate when you increase oxygen, checking LFTs when the patient on high dose Tylenol looks off, ordering a BMP before giving multiple doses of IV Lasix. That’s the judgment we notice.
What We Notice About How You Handle Nursing Pages
Here’s the part you don’t see: after a rough night, charge nurses debrief. They talk about you. And then they talk to us.
You think the attending just “happens” to know you were slow, or dismissive, or impossible to reach? No. Night nurses absolutely report residents—informally and formally.
We watch how the floor behaves when we walk in at 7 a.m. Are nurses calm, updated, relatively satisfied? Or are there three of them waiting to ambush us at the door with, “We paged multiple times about…”

Here’s what attendings really notice from the nursing side:
- Do you answer pages reasonably fast, or do pages cluster with “second attempt,” “third attempt” comments?
- Do you actually go see the patient, or do you order Tylenol, Zofran, melatonin from your chair for every complaint?
- Do you document even a one-liner when things get dicey, so we can see your thought process?
Nurses absolutely know which residents are safe at night. The ones they’re nervous about? That gets back to us one way or another.
And once a nurse says, “I don’t feel safe when X is covering nights,” it’s very hard to un-hear that.
The Hidden Metrics Attendings Use to Judge You
Everyone thinks night float is about “surviving” and “staying awake.” Attendings are watching an entirely different scoreboard.
Here’s what we actually track in our heads:
| Metric | What It Really Tells Us |
|---|---|
| Timestamps on key orders | Urgency and situational awareness |
| Call vs no-call patterns | Risk recognition and humility |
| Note timing and content | Ownership and reasoning |
| Nursing feedback/tone | Reliability and safety culture |
| Morning sign-out quality | Organization and priorities |
Ownership, Not Heroics
One of the biggest things we notice is ownership. Not how smart you are. Whether you treat the patients like they’re your patients for that night.
That looks like:
- Leaving a short, focused event note at 3 a.m. summarizing an RRT or deterioration, even if it’s not required
- Letting the day team know in your sign-out, “I was actually worried about X; I think they could crash later today”
- Fixing obvious problems (pain control, bowel regimens, DVT prophylaxis) instead of saying, “Day team can handle it”
Residents who act like “I’m just covering, it’s not my problem” get labeled quickly. We don’t say it out loud, but we know you’re the type who disappears when things get hard.
Your Ability to Triage Competing Fires
On a bad night, you will have more problems than minutes.
We see if you can:
- Drop low-yield tasks when real emergencies arise
- Chain tasks logically (see the crashing patient, then while you’re up there, check in on nearby borderline ones)
- Communicate with nurses: “I’m in a code, I’ll be up in 20; in the meantime, please do X, Y”
The resident who spends 20 minutes rewriting a useless med rec while a hypotensive patient waits is never going to be trusted with a sick unit. Whether we ever explicitly tell them or not.
Documentation: What We Read Between the Lines
Attendings don’t read every one of your notes. We do skim patterns.
What stands out on nights:
A 4-line event note at 2:45 a.m. after a near-RRT: “Paged for rising O2 needs, patient now 6L from 2L, RR 28. Exam: diffuse crackles, tachycardic. Gave 40 IV Lasix, ordered stat CXR, ABG, discussed with ICU fellow, will follow closely.”
That tells us: you recognized it, you had a plan, you closed the loop.A zero documentation night where three patients got significant new interventions, but the chart is quiet. That tells us: you’re not thinking like the responsible physician, you’re acting like a firefighter with amnesia.
Also, the tone of your notes matters. We all catch the passive-aggressive resident who writes, “Multiple pages overnight from nursing about patient’s complaint of pain” with an eye roll embedded in the EMR. That sort of thing travels fast in the wrong way.
Sign-Out: Where Attendings Quietly Judge Your Mind
Morning sign-out is a gold mine. Attendings sit there, mostly silent, and listen to how you summarize.

We’re listening for:
- Can you distinguish signal from noise? Or do you report every blood pressure fluctuation like it was a crisis?
- Do you know which patients scared you overnight—and can you explain why in two sentences?
- Do you admit when you were uncertain and what you did about it?
If you sound scattered, disorganized, or surprised by information in your own sign-out (“Oh, I guess they did get another fever at 4 a.m.”), we know your overnight mental model is weak.
The residents who say, “There were a lot of pages, but only two patients I’m truly worried about now, let me start with those,” and then give tight, focused updates? Those are the ones we trust later with sicker teams.
The Stuff You Think Matters (But We Don’t Care That Much About)
Let me burst a few illusions.
Attendings are not deeply impressed by:
- How late you stay charting after your shift. Staying till 10 a.m. finishing notes after a night float does not read as “hardworking.” It reads as “inefficient and at risk for mistakes because you’re exhausted.”
- How many “interesting” zebras you diagnosed at 3 a.m. Most of the time, your job at night is not to diagnose rare diseases; it’s to keep people alive and stable.
- Your heroic stories about “not sleeping at all.” That’s not a flex. That tells us you have no idea how to manage your own bandwidth, which is dangerous.
Stop trying to impress by suffering. No one healthy is grading you on misery.
The Things Attendings Actually Respect on Night Float
You want to know what really builds your reputation on nights? Here it is, bluntly.

| Category | Value |
|---|---|
| Clinical judgment | 30 |
| Responsiveness | 25 |
| Organization | 20 |
| Humility | 15 |
| Raw knowledge | 10 |
Residents who earn quiet respect tend to show the same traits:
They call early for truly sick patients—but not for everything. “I might be overcalling, but this feels like the beginning of something bad, not the end” is a sentence that makes attendings listen.
They’re transparent about uncertainty. They don’t bluff. They say, “This is what I saw, this is what I was thinking, here’s what I did, here’s what I’m still worried about.”
They protect morning rounds. This one is subtle: they anticipate what will blow up rounds and handle what they can. Things like getting urgently needed labs drawn, making sure someone with rising O2 needs is evaluated before 7 a.m., not at 8:30 when half the team is in a conference.
They don’t throw people under the bus. Blaming nurses, blaming the ED, blaming the previous team—if that’s your reflex every time something goes wrong at night, we notice. And we assume you will do the same to us when we’re not in the room.
And maybe the biggest one: they learn visibly during the block. The first few nights, calls are messy and anxious. By the second week, their pattern sharpens. They’re calling less but smarter. Their documentation is clearer. Their anticipatory planning improves. That growth curve gets remembered.
How to Actually Survive Night Float Without Damaging Your Reputation
No, this isn’t going to be the usual “drink water, bring snacks” nonsense. You already know that.
Here’s how the residents who come out of night float stronger actually run their nights.
Build a Mental “Red List”
Before your shift really starts, make your own list of patients you do not trust. The borderline ones. The “something feels off” ones. Then proactively check on them early, not when the nurse finally snaps and pages you at 3 a.m.
Even a 2-minute bedside check at 11 p.m. buys you information and credibility. And it prevents 4 a.m. disasters.
Treat Every RRT as a Personal Teaching Case
After the dust settles, spend 5–10 minutes reading: what happened earlier in the day, what subtle warning signs were there, what would you do differently next time. Then write a tight note.
By the end of one night float block, you can get a mini-fellowship in early decompensation recognition—if you actually do this. Attendings notice which residents get sharper with each scare and which ones never learn.
Script Your “Call the Attending” Conversations
The worst calls are wandering and vague: “So uh… they don’t look great.”
Before you dial, get your script straight in your head:
- Who is this? (Name, age, why they’re admitted.)
- What changed? (Objective vital/lab change, not just “they look bad.”)
- What did you see? (Key exam points.)
- What did you already do?
- What are you worried about? (Two or three concrete possibilities.)
- What do you want? (Transfer, orders, just a sanity check?)
Residents who can present like that at 3 a.m. earn an enormous amount of trust very fast.
Have the “Lines in the Sand” Clear
Know before night one on each service: which things your attendings absolutely want to be called about. Many will state it once—“Call me for chest pain, new pressor, unplanned ICU transfer, or anything that makes you personally nervous”—and then assume you’ll remember.
If they don’t say it, ask them directly. “What do you definitely want to be called for overnight?” That one question makes you look more mature than half your class.
The Underground Truth: Night Float Follows You
Here’s the part no one tells you during orientation.
Attendings talk about night float performance when promotions, fellowship letters, and chief resident discussions come up. I’ve sat in those rooms. I’ve heard:
- “She’s fine during the day, but nights… I wouldn’t leave her alone with a sick floor.”
- “He grew a lot on nights; his judgment really tightened up.”
- “The nurses love her overnight. They feel very safe.”
No one says, “We’re ranking you based on your night float month,” but it weights the impression of your reliability. A surprisingly large amount.
So if you’re going into nights thinking, “This is just a miserable month to get through,” you’re missing the truth: this is one of the few rotations where attendings see what kind of doctor you are when the structure falls away.
They are watching. Silently, through the EMR and through the morning chaos and the nursing grapevine.
Use that to your advantage.

Quick Recap: What Actually Matters on Night Float
Keep these in your head on the way in:
- Attendings judge your nights by patterns: time to action, what you call for, how your orders and notes line up with the story.
- Nursing feedback and morning sign-out say more about your safety and reliability than any individual “cool save” you pull off.
- The residents who own their patients, communicate cleanly, and learn visibly during nights are the ones attendings remember—in a good way—long after the block ends.
FAQ
1. How often should I call the attending overnight without looking incompetent?
Call more in your first few nights and tighten over time. If it’s an unplanned ICU transfer, new chest pain, hypotension that does not respond to simple measures, respiratory status change requiring more than a small bump in O2, or anything that makes you uneasy—call. You look far more incompetent missing a crash than “bothering” someone at 2 a.m. with a focused concern.
2. What’s the biggest red flag attendings see on night float?
Delayed response to real instability. When the chart shows hours between concerning vitals and meaningful action, that’s the fastest way to be labeled unsafe. Sloppy documentation and blaming others run a close second.
3. How do I handle being overwhelmed by multiple sick patients at once?
Triage: identify the truly crashing patient and get there physically first. As you move, give clear instructions to nurses on the others (“Draw a lactate, increase O2 to 4 L, I’ll be there in 15 minutes, page me if X happens first”). If you have more than one person you’re afraid will die in the next hour, call for help—attending, ICU, rapid response—early.
4. Can a bad night float month really hurt my fellowship chances?
One rough night will not. A pattern of poor judgment, bad feedback from nurses, and attendings saying “I don’t trust them alone on nights” absolutely can. Fellowship directors listen to those off-the-record impressions. The good news: a strong night float where you clearly grow and show solid judgment can help you just as much.



















