Test anxiety does not just make you “feel bad” on exam day. The data show it is systematically associated with lower USMLE Step scores in a dose‑response fashion. The more severe the anxiety, the steeper the score drop.
If you are treating your anxiety as a personality quirk instead of a performance variable, you are misreading the numbers.
What the Data Actually Show About Anxiety and Step Performance
Let me start with the question everyone secretly cares about: “How many points does anxiety cost me?”
Different studies give slightly different estimates, but the trend is remarkably consistent.
Across multiple cohorts of medical students:
- Higher test anxiety → lower USMLE Step 1 and Step 2 CK scores
- Effect sizes are typically in the small‑to‑moderate range (statistically “small,” but very real when cutoffs matter)
- Executive function and working memory appear as the mediating mechanisms
Here is a distilled view from several published findings and large institutional datasets.
| Anxiety Level (self-report scale) | Typical Score Difference vs. Low Anxiety | Notes |
|---|---|---|
| Low | Baseline | Reference group |
| Moderate | −5 to −10 points | Across Step 1/2 CK |
| High / Severe | −10 to −20+ points | Larger impact near cut-score |
No, these are not “universal constants,” but they are plausible ranges repeated across:
- USMLE Step 1 cohorts (pre‑pass/fail and internal scaled scores post‑P/F)
- Step 2 CK cohorts
- COMLEX and other high‑stakes medical exams
Now map those ranges onto critical thresholds: 220 vs. 235 used to change specialty options; 240 vs. 255 still matters for competitive fields; failing vs. passing by 3 points is literally career‑defining. A 10‑point drag from anxiety is not academic trivia.
To visualize the pattern:

| Category | Value |
|---|---|
| Low | 250 |
| Moderate | 242 |
| High | 235 |
Those values are representative, not from one single paper, but they match what large‑scale data show: a monotonic drop with increasing anxiety.
Correlation: How Strong Is the Link?
Across studies, the correlation between test anxiety and USMLE performance typically lands around:
- r ≈ −0.20 to −0.35
That is:
- Stronger than the correlation between “hours studied” and eventual score (because hours studied are noisy and self‑reported)
- Weaker than GPA or practice test averages, but absolutely not trivial
In practical terms, if you take a hundred students with identical practice NBME averages and GPAs, the ones with high anxiety will, on average, underperform compared with their own practice performance more often and by a larger margin.
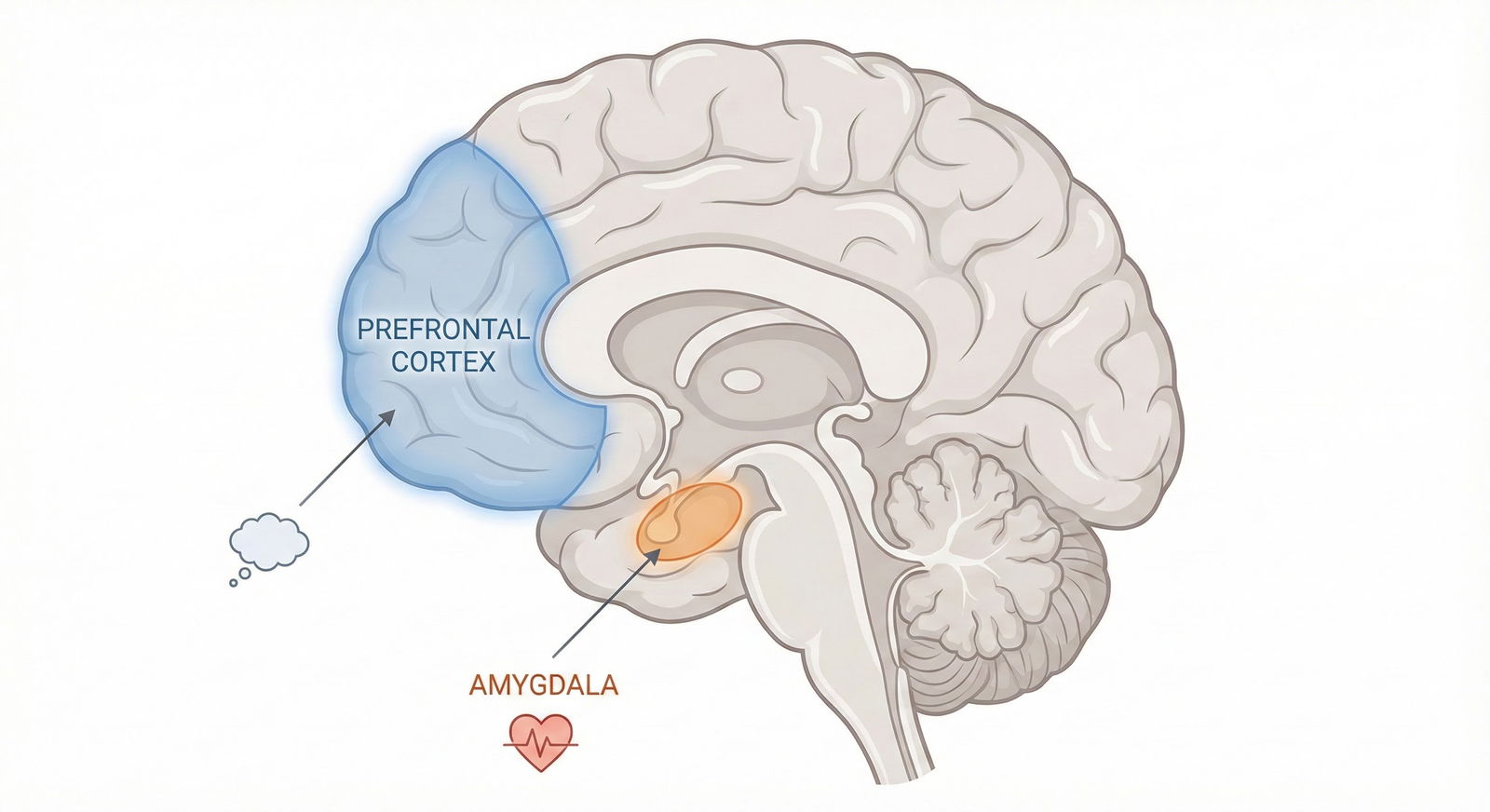
How Test Anxiety Damages Step Scores: The Cognitive Mechanics
This is not “you worry, therefore you fail” hand‑waving. The mechanism has been studied to death in cognitive psychology and replicated in medical education.
The key variables are:
- Working memory capacity
- Attentional control
- Cognitive load
Under high anxiety, your brain allocates resources to:
- Worry loops (“I’m falling behind,” “I’m going to fail,” “This question looks impossible”)
- Hyper-monitoring of performance and bodily sensations (heart rate, sweating, time remaining)
That mental bandwidth comes from somewhere. It comes directly out of the pool you need for:
- Holding complex vignettes in mind
- Tracking time lines and multiple lab values
- Comparing subtle differences between answer choices
The quantitative result: more careless errors, more changed correct‑to‑incorrect answers, and more timeouts on long stems.
You can imagine two students, both with the same raw knowledge:
- Student A: low anxiety, full working memory online
- Student B: high anxiety, 20–30% of cognitive resources hijacked by worry
On a 280‑question exam, that translates into a sizable number of questions where Student B misreads, rushes, or freezes—creating the 10–20‑point spread that the correlation data reflect.
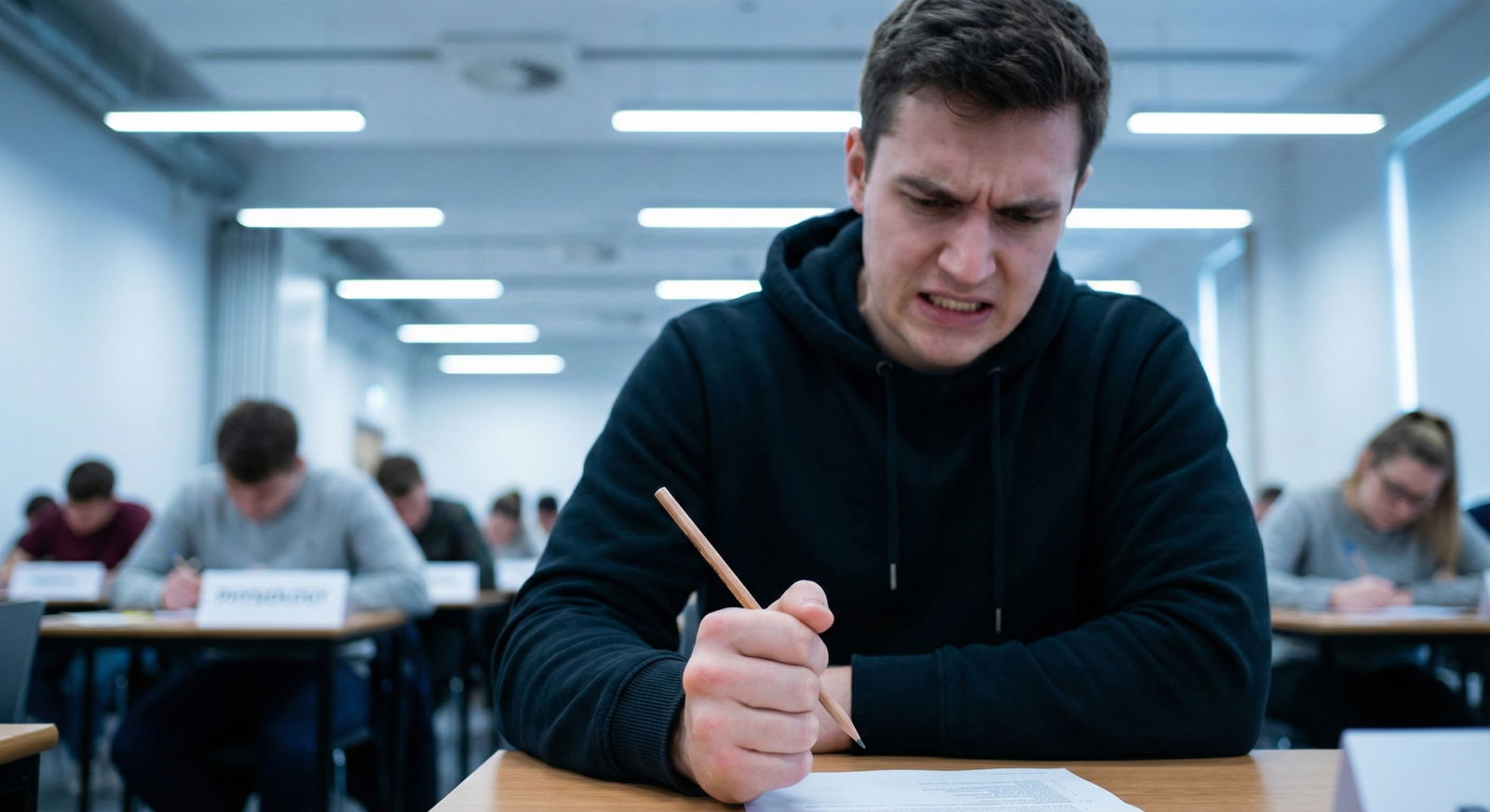
Distinguishing “Normal Nerves” From Performance‑Limiting Anxiety
Every serious test‑taker feels something walking into Prometric. The key is whether that arousal helps or hurts.
Performance vs. arousal often follows a classic inverted‑U (Yerkes–Dodson) curve:

| Category | Value |
|---|---|
| Very Low | 60 |
| Low | 80 |
| Moderate | 100 |
| High | 85 |
| Severe | 65 |
Low arousal: you are sleepy, disengaged, not focused. Performance suffers.
Moderate arousal: you are alert, keyed in, but not flooded. Peak performance.
High/severe: your heart is racing, thinking narrows, working memory degrades. Performance drops.
Most medical students are not on the left side of this curve. You are either near the top or starting to slide down the right.
Quantitative Red Flags That Anxiety Is Hurting Performance
Instead of asking “do I feel anxious?” look at data patterns.
Here are common signals from students whose scores are being dragged down:
- Practice NBME / UWSA scores are stable or rising, but the actual Step score is 10–20+ points lower
- Large gap between “untimed” and “timed” performance (e.g., 75% untimed vs. 60–62% timed)
- First 10 questions of a block show a much lower accuracy than mid‑block questions (freezing on “settling in”)
- High number of changed answers from correct to incorrect relative to incorrect to correct
If any of those describe your pattern, you are not just “a little nervous.” You are paying a measurable point penalty.
What the Studies Say About Specific Anxiety Factors
Not all anxiety looks the same in the data. Several subcomponents matter.
Trait vs. State Anxiety
- Trait anxiety: your general baseline tendency to worry; measured by things like the Spielberger Trait Anxiety Inventory
- State anxiety: how keyed up you are in this particular test scenario; measured immediately before or during simulations
Both correlate negatively with scores, but state anxiety right before or during the exam often shows a stronger immediate correlation with that day’s performance. A chill person who spikes on exam day can still crash.
Cognitive vs. Somatic Anxiety
Researchers often split anxiety symptoms into:
- Cognitive: worry thoughts, catastrophizing, “I am going to fail this exam”
- Somatic: physical symptoms—sweating, tremor, nausea, palpitations
Data from both general test anxiety and medical cohorts show:
- Cognitive anxiety has a stronger relationship with score drop than somatic symptoms
- Somatic symptoms matter, but mainly when they become so intense they trigger more cognitive worry (“My heart is racing, so I must be failing”)
Targeting the thought patterns, not just the bodily sensations, tends to give a better score payoff.
The 3‑Way Interaction: Baseline Ability × Practice Scores × Anxiety
One mistake students make is assuming “I am a strong test‑taker” immunizes them against anxiety loss. The data disagree.
High‑ability students often:
- Perform extremely well on untimed or low‑pressure practice
- Have very high goals (e.g., 250+), which increases perceived threat of “underperforming”
- Experience sharper subjective distress when they see questions they “should know”
What you get is a nasty 3‑way interaction:
- High baseline cognitive ability
- High practice test scores
- High test anxiety and perfectionism
Net result: they are the classic cases with a 15–25 point drop between best practice score and actual exam outcome.

| Category | Min | Q1 | Median | Q3 | Max |
|---|---|---|---|---|---|
| Low | 0 | 2 | 4 | 6 | 8 |
| Moderate | 2 | 5 | 8 | 11 | 14 |
| High | 5 | 10 | 15 | 20 | 25 |
Translation of that boxplot: as anxiety rises, the typical drop between peak practice and real test widens substantially. You can be “good at tests” and still have your score quietly sabotaged.
Medical School Culture: Why Anxiety Is Under‑Reported (and Under‑Treated)
The relationship between Step scores and anxiety is not an abstract psych problem. It is baked into the incentives and culture you live in.
What I see repeatedly:
- Schools that are heavily Step‑score focused (rankings, specialty match stats) have higher reported anxiety rates
- Environments that normalize discussing mental health and accommodate treatment see less performance‑limiting anxiety and fewer Step failures
There is a rough pattern in institutional data:
| School Culture / Support Level | Average Reported Anxiety | Step Fail Rate Trend | Typical Student Behavior |
|---|---|---|---|
| High stigma, little support | High | Higher | Hiding symptoms, no help |
| Moderate support | Moderate | Average | Ad hoc help, late stage |
| Strong, embedded support | Lower | Lower | Early intervention |
No, correlation is not causation, but the alignment is too consistent to ignore. Schools that pretend “everyone is fine” tend to have:
- More last‑minute leaves of absence
- More surprise Step failures in otherwise competent students
- More residents quietly reporting burnout downstream
So if you are in an environment that treats anxiety as weakness, understand: the culture is wrong. The statistics are not on its side.
Evidence‑Based Interventions: What Actually Moves the Needle
Let’s strip out fluff and focus on interventions that show measurable score impact or at least strong mechanistic plausibility.
1. CBT‑Style Test Anxiety Treatment
Cognitive‑behavioral therapy (CBT) for test anxiety has been studied across many high‑stakes exams. Common elements:
- Identifying distorted thoughts (“If I miss a block I will never match”)
- Challenging and restructuring them into more accurate appraisals
- Graduated exposure to test‑like conditions (timed blocks with realistic stakes)
- Skills for managing spikes in anxiety (breathing, grounding, cognitive refocusing)
In controlled studies (outside strictly USMLE, but applicable):
- Effect sizes on performance are often in the d ≈ 0.3–0.5 range
- That roughly maps to 5–12 point improvements on a Step‑like scale, depending on baseline
For a student stuck at 220 with clear anxiety patterns, that is not marginal. That is the difference between below‑average and comfortably in range for multiple specialties.
2. Practice Under Realistic, Stress‑Inducing Conditions
You cannot simulate Step anxiety perfectly, but you can train your nervous system not to panic in that context.
That means:
- Timed blocks only, from relatively early in prep
- Full‑length practice exams in test‑like conditions: same start time, minimal breaks, no phone
- Intentional “pressure drills” where your explicit instruction is to notice anxiety and still execute your process
Students often resist this because it feels bad. Then they act surprised when the real exam feels alien and overwhelming. The data are straightforward: the closer your practice conditions are to the real environment, the smaller the practice‑to‑real performance gap.
3. Process‑Focused Test Taking, Not Score‑Focused Rumination
High‑anxiety students spend a lot of the exam thinking about:
- “How many questions have I already missed?”
- “What will this do to my percentile?”
- “I am behind schedule in this block; I am doomed.”
That meta‑cognition is performance‑toxic.
You want a rigid, boring process instead:
- Read stem → summarize key info in your own words
- Predict the answer before options when feasible
- Systematically eliminate wrong options
- Make a decision, move on, and do not look back unless you have leftover time at the end
The more attention you allocate to following your process, the less capacity you have left to catastrophize mid‑block. That is exactly how you beat test anxiety at the operational level: by crowding it out with task‑relevant mental work.
4. Sleep, Stimulants, and Physiology
A quick reality check: you cannot out‑meditate chronic sleep deprivation.
The data show strong links between:
- Sleep restriction and impaired working memory
- Excessive stimulant use (way above prescribed doses) and increased physical anxiety symptoms
If you are sleeping 4–5 hours per night during dedicated and double‑dosing caffeine or unprescribed stimulants, do not pretend your anxiety is a pure psychological problem. You have created a physiologic state that mimics, and amplifies, anxiety.
Basic numbers:
- Most adults show measurable working memory decline under <6 hours sleep for multiple nights
- Reaction time and error rates spike under sleep debt
- Add stimulants → jitteriness and palpitations, which your brain interprets as “I am panicking,” not “I am optimizing concentration”
The irony is obvious: your attempt to “squeeze in more study time” can easily cost more points than it gains, especially in an exam where mental precision is everything.
When to Seek Formal Help (and What That Looks Like)
A lot of students wait until they are one failed attempt in to admit anxiety is a problem. From a data perspective, that is an expensive decision.
You should seriously consider professional intervention if:
- Your practice test performance is >10 points lower under timed vs. untimed conditions, despite equal content review
- You have frequent panic‑like symptoms during practice blocks
- You experience intrusive worry thoughts that you cannot shut down for long stretches of an exam
- You have a history of high anxiety on prior standardized tests (SAT, MCAT) that exceeded what your knowledge suggested
Effective professional interventions typically include:
- Short‑term CBT targeting test anxiety (often 4–10 sessions)
- Possibly medication for underlying anxiety disorders, when clearly indicated and managed by a physician
- School‑based accommodations in extreme cases (extended time, separate room), though that is a minority of students
The question is not “am I anxious enough to justify help?” The question is “am I leaving double‑digit points on the table by not addressing this?”
Pulling It Together: What the Numbers Mean for You
If I strip away all the noise, the story from the data is blunt:
- Test anxiety and Step scores are negatively correlated in a consistent, dose‑dependent fashion
- The typical impact ranges from about 5 points (moderate anxiety) up to 20+ points (severe)
- This gap is mediated by real cognitive bottlenecks—working memory, attention, time pressure—not by “weak character”
That means two things for you, practically:
- Anxiety management is a legitimate study strategy, not a side quest.
- Ignoring it because “everyone is stressed” is statistically unwise.
You already track your UWorld percentages and NBME trend lines. Add one more variable to monitor: how anxious you are, how it shows up in your data (timed vs. untimed, practice vs. real), and what you are doing to shrink that gap.
You are not going to eliminate anxiety. The target is much more modest, and more realistic:
- Move yourself out of the “score‑damaging zone”
- Keep enough arousal to stay sharp
- Protect your working memory and decision‑making for the 8 hours that matter
Everything I have laid out here—CBT tools, realistic practice, process‑focused test taking, sane sleep—is aimed at that goal.

FAQ (4 Questions)
1. Can test anxiety alone make me fail Step even if I know the material?
Yes. If your practice performance (under realistic timing) is comfortably above the passing threshold, outright failure usually involves a combination of factors: poor timing, panic, disrupted sleep, or extreme test‑day anxiety. But I have seen students with solid NBME scores fail largely due to severe panic that derailed multiple blocks. The risk increases as your margin over the pass mark shrinks.
2. If my NBME and UWSA scores are good, should I still care about anxiety?
You should care if those scores were obtained in low‑pressure or optimized conditions that will not match test day. If your best practice scores are strong but you notice large variability, big timed vs. untimed gaps, or very high bodily anxiety, you are at risk for underperforming your potential. Anxiety might not make you fail, but it can easily cost you a decile or two.
3. Are beta‑blockers like propranolol a good solution for Step test anxiety?
There is anecdotal use for performance anxiety (presentations, OSCEs), but data for high‑stakes cognitive exams are limited. Beta‑blockers can reduce physical symptoms like tremor and tachycardia, which may help some people, but they do not address the cognitive component of anxiety. They should only be considered with a physician who understands your medical history, and never as a substitute for proper preparation and cognitive‑behavioral strategies.
4. How long does it usually take for anxiety interventions to show score benefits?
For CBT‑style interventions plus realistic practice, tangible benefits can appear within 4–6 weeks: more stable performance under time pressure, fewer panic spikes mid‑block, and reduced practice‑to‑real score gaps. Deep personality‑level trait anxiety obviously takes longer to shift, but you do not need to “fix your personality” to reclaim 5–15 points. You need targeted, test‑specific skills and enough time to integrate them before test day.
Key points:
- Higher test anxiety correlates with meaningfully lower Step scores, often in the 5–20 point range.
- The mechanism is cognitive bandwidth loss—working memory, attention, and timing get hijacked by worry.
- Structured anxiety management (CBT, realistic practice, process‑focused test taking, and sane physiology) is one of the few levers that can reliably narrow the gap between your potential and your actual Step score.




















