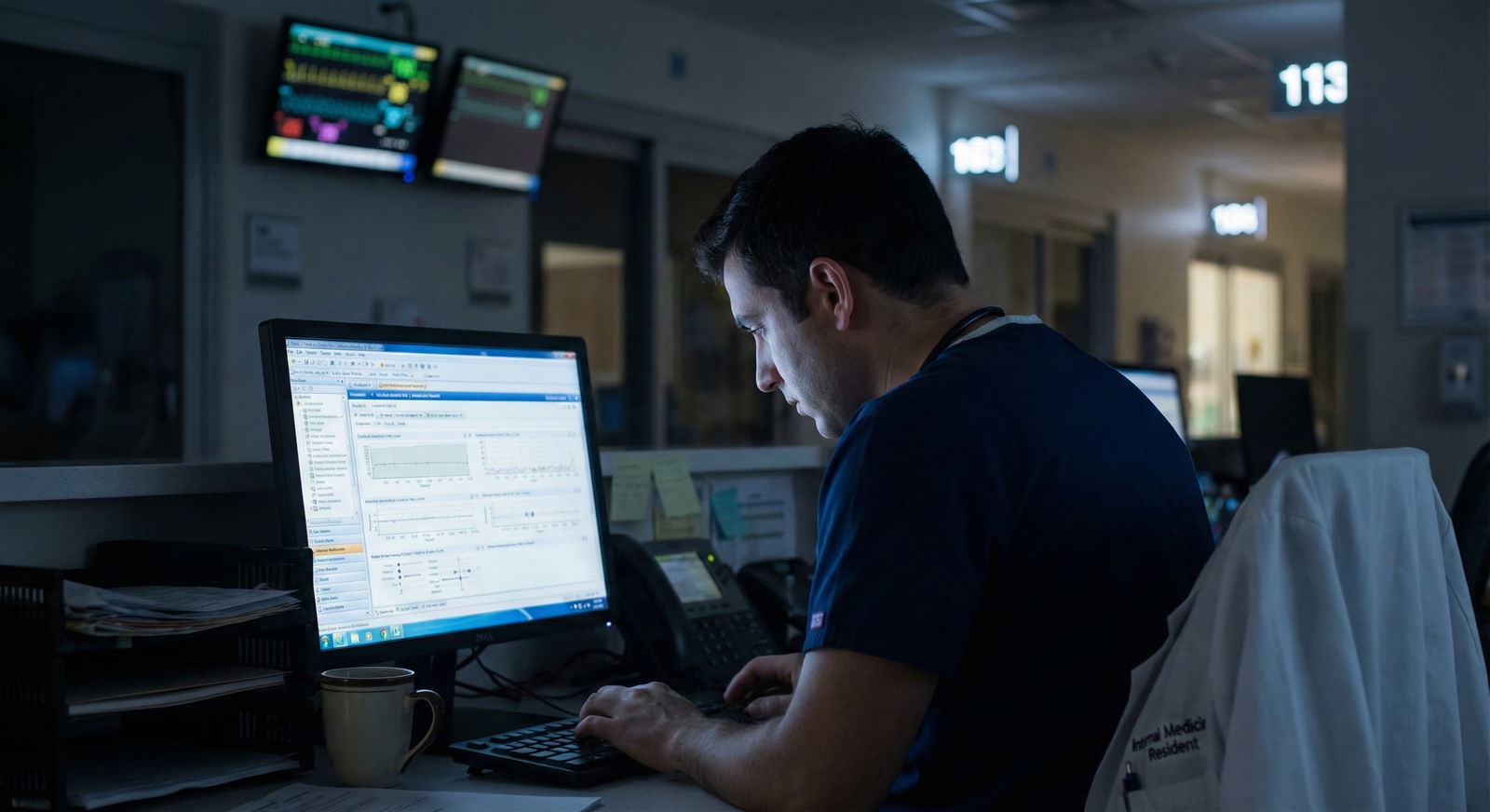
It’s 10:45 p.m. You just signed out, you’re finally home, and someone in your class texts: “Hey, I just scheduled Step 3 for December, when are you taking it?”
You freeze. Because you haven’t even decided when to take Step 3, let alone started studying.
Here’s the answer you’re looking for: the best time to take Step 3 is usually between 6–18 months into residency, during a lighter rotation, after you’ve taken Step 2 CK and before fellowship applications or licensing deadlines hit.
That’s the simple version. Let’s break it down with real-world nuance so you can pick your best timing, not some generic “end of intern year” line people repeat without thinking.
The Core Rule: Align Step 3 With Three Things
Ignore the noise and focus on this: your ideal Step 3 timing is when three conditions line up:
- Your knowledge is adequate
- Your schedule is sane
- Your program and career timelines demand it
If any of those three is off, your timing’s bad.

| Category | Value |
|---|---|
| Knowledge Readiness | 40 |
| Schedule Flexibility | 35 |
| Career/Program Requirements | 25 |
Let me walk through how this actually plays out by year of residency and specialty.
Year-by-Year: Pros and Cons of Step 3 Timing
Taking Step 3 Before Residency (Rare, but possible)
This applies to a small group: prelim/TY folks who have a gap, or people with visa issues needing early completion.
Pros:
- Step 1 + Step 2 + Step 3 all done before residency. No exam hanging over you.
- You can focus fully on clinical training once you start.
Cons (and they’re big):
- You haven’t practiced real inpatient medicine, discharges, follow-up, or continuity care yet. A lot of Step 3 case management will feel abstract.
- You’re burned out from Step 1/2 and want to be done with exams, but this often leads to a mediocre performance.
- Many states don’t even let you register for Step 3 until you’ve got an MD/DO and/or some GME underway.
My opinion:
Unless your situation is unusual (immigration/licensing/visa), don’t take Step 3 before residency. It’s timing that looks efficient on paper and usually backfires in practice.
Taking Step 3 Early in Intern Year (First 3–6 Months)
You start residency in July, you’re on steep learning curve mode, adjusting to EMR, notes, call, sign-out, everything. Some people still try to cram Step 3 here.
Pros:
- Your Step 2 CK knowledge is relatively fresh.
- You get it out of the way before you’re responsible for a team, notes, supervising juniors, etc.
- If you’re on a cush outpatient or elective block early, you may have study time.
Cons:
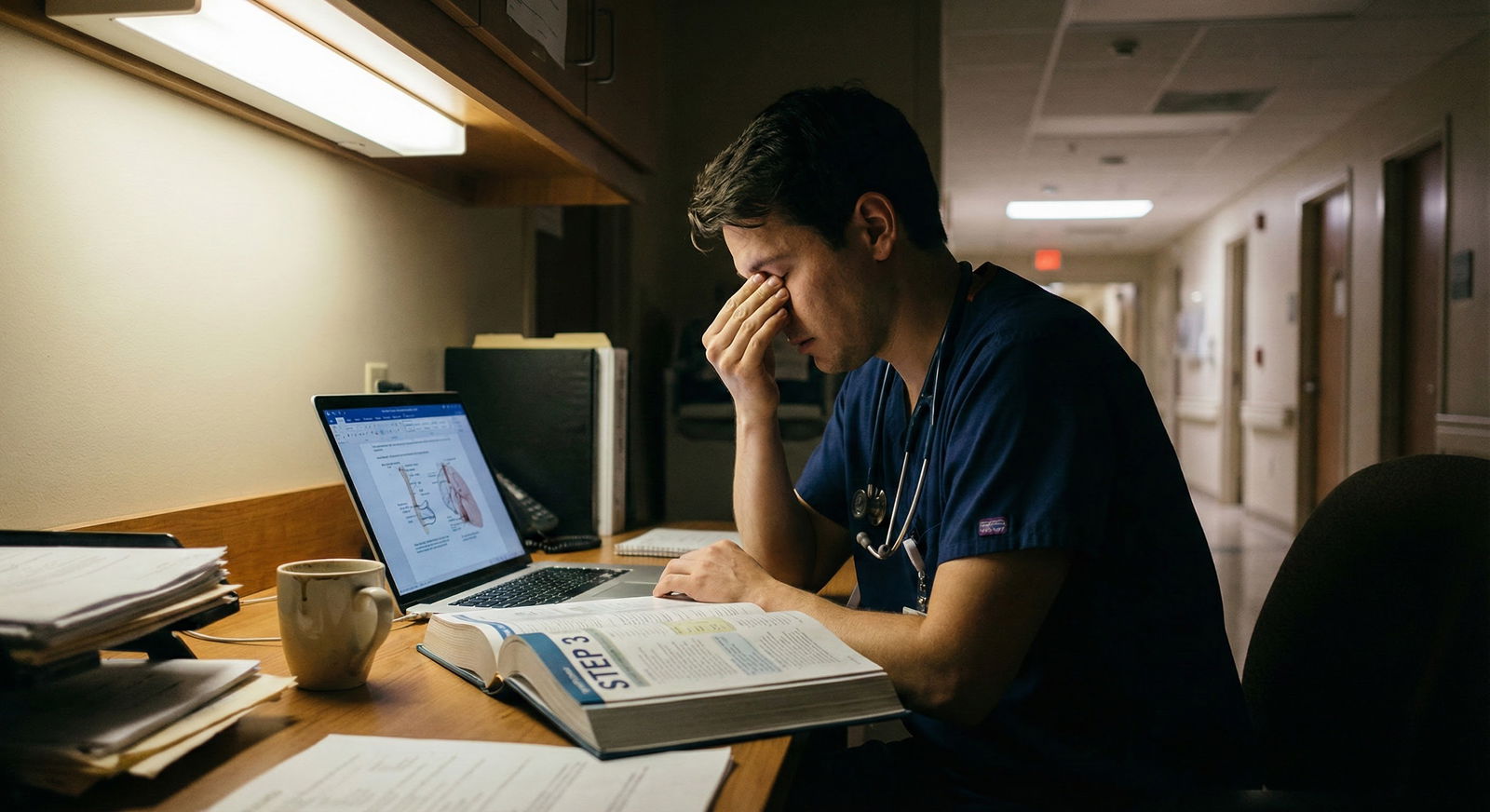
- You’re still figuring out how to be a doctor, and that’s already a cognitive overload.
- You often don’t have a good feel yet for systems of care, ambulatory management, long-term chronic disease follow-up — big themes on Step 3.
- Higher risk of burnout, because you’re layering exam prep on top of one of the steepest transitions in your career.
Who this works for:
- IM/FM/peds interns with:
- A legitimately light early outpatient or elective rotation
- Recently took Step 2 CK and scored solidly (think ≥ 240 equivalent)
- Limited need for visas, fellowships soon, etc.
Verdict:
Reasonable but not ideal for most. Only do this if you clearly have both a light block and strong Step 2 foundation.
Taking Step 3 Late Intern Year / Early PGY-2 (Most common sweet spot)
This is where most residents should land, if they plan it correctly.
Timeline: Somewhere between January of PGY-1 and December of PGY-2.
Why this window works best:
Knowledge maturity
You’ve seen:- Bread-and-butter inpatient medicine
- Common ED presentations
- Transitions of care
- Ambulatory follow-ups (at least some)
That alone makes the CCS cases and management questions feel far more intuitive.
You understand your schedule
By mid-PGY-1, you know:- Which rotations are brutal
- Which ones are “study-capable” (clinic-heavy, elective, research, consult service)
- How you personally tolerate nights and call
You’re ahead of career deadlines
For competitive fellowships (cards, GI, heme/onc, etc.), programs like having Step 3 done by the time you’re applying (mid-PGY-2). Some states and programs also want Step 3 completed by the end of PGY-2 for full licensure or moonlighting.
Ideal combo:
Light rotation + 6–18 months of clinical experience + at least 6 weeks of semi-consistent study time.
| Specialty | Typical Timing | Main Reason |
|---|---|---|
| Internal Medicine | Late PGY-1 to early PGY-2 | Prep for fellowship, solid clinical base |
| Family Medicine | Mid PGY-1 to mid PGY-2 | Early outpatient continuity experience |
| Pediatrics | Late PGY-1 to PGY-2 | Mix of inpatient/outpatient exposure |
| Surgery | PGY-1 light rotations or research year | Schedule intensity later |
| Psychiatry | PGY-2 | Ambulatory + chronic care perspective |
My opinion:
For most residents, this is the best time window. The exact month will depend on when you have a not-insane block.
Taking Step 3 Late (Late PGY-2 or PGY-3+)
Sometimes you blink and it’s PGY-3 and Step 3 still isn’t done. I’ve seen this happen a lot.
Reasons people delay:
- Busy or malignant schedule early on
- Severe Step test anxiety and avoidance
- International grads dealing with visas, paperwork, multiple moves
- Underestimating how annoying this exam will feel once you’re tired and jaded
Risks of delaying too long:
- Some programs mandate Step 3 by:
- End of PGY-2 (common)
- Before promotion to senior resident
- Some states require Step 3 within a certain number of years from Step 1/starting residency.
- Exam knowledge does degrade over time — especially biostatistics, ethics, ambulatory medicine details if you’re in a very inpatient-heavy or procedural specialty.
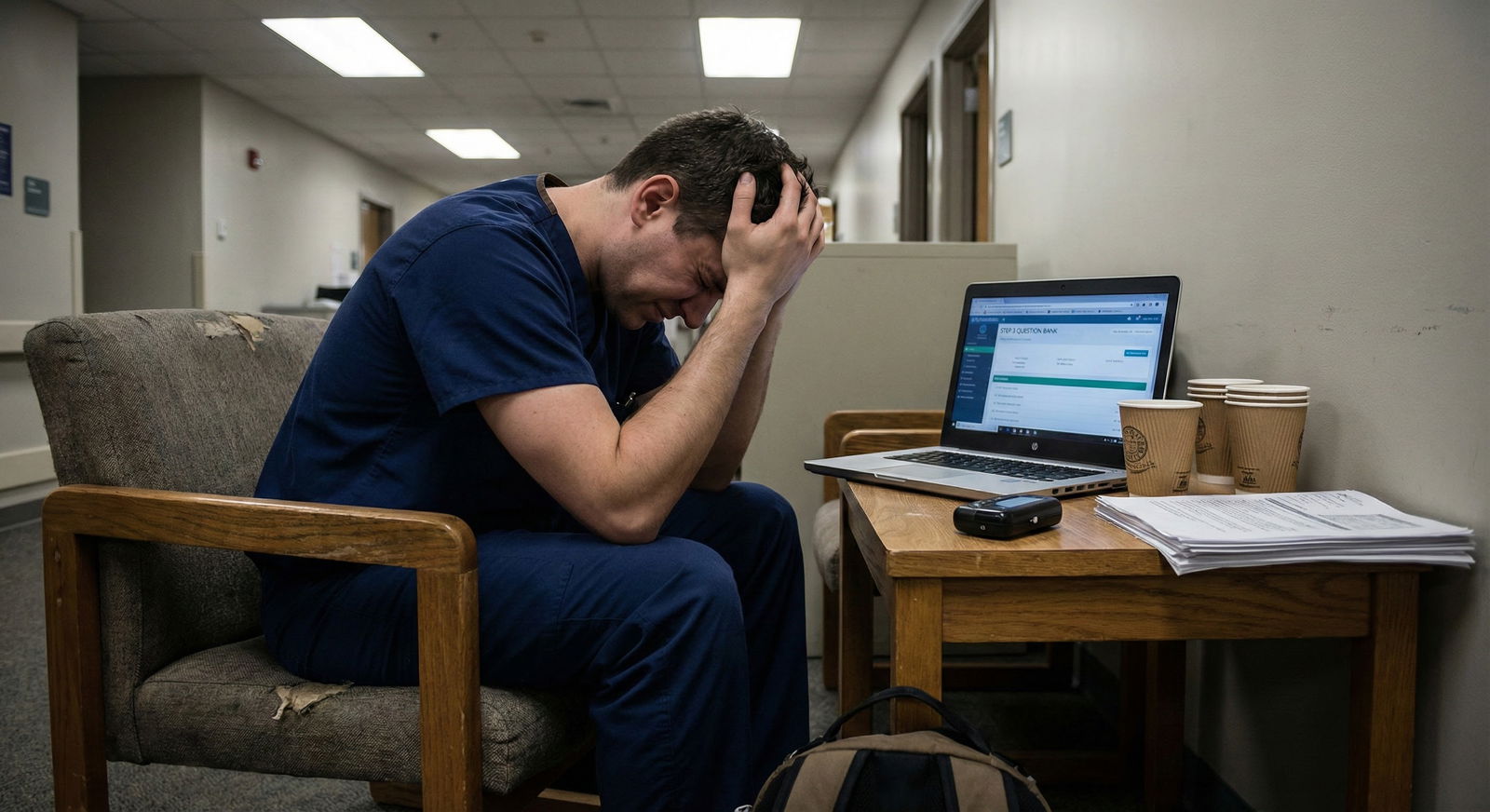
Also, late timing tends to collide with:
- Chief responsibilities
- Fellowship interviews
- Board prep for your specialty
Now you’re juggling multiple high-stakes tasks at once, and Step 3 becomes an annoying fire you’re constantly trying not to let spread.
Who sometimes needs to delay:
- Surgical residents with brutal PGY-1 and PGY-2 schedules and no true “light” blocks until research year
- Residents with early major life events: serious illness, childbirth, etc.
My opinion:
Don’t let Step 3 drag into late PGY-2 or PGY-3 unless you absolutely have to. The mental tax of “that exam I still haven’t taken” is real, and it doesn’t improve with time.
Program, State, and Visa Requirements: Non-Negotiables
Here’s the not-sexy but crucial part: some of your timing may be forced.
1. Your residency program rules
Every program has its own Step 3 expectations. Examples I’ve actually seen:
- “Must pass Step 3 by end of PGY-2 to be promoted to PGY-3.”
- “Must complete Step 3 before moonlighting privileges are granted.”
- “Completion of Step 3 is required before taking the in-service board exam seriously for promotion decisions.” (Yes, that was poorly worded. No, they didn’t care.)
Ask your program coordinator straight up:
- Is there a deadline for Step 3?
- Any months/rotations strongly recommended or reserved for exam prep?
- Any residents historically struggled because they took it too late?
2. State licensing timelines
Full medical license requirements vary a lot state-to-state. Some states:
- Require Step 3 to be eligible for full license
- Have time limits between Steps (e.g., all 3 Steps within 7 years)
- Need a full license by a certain PGY-year to continue training/more advanced duties
If you’re in a state with a strict clock, you can’t just “take it whenever.”
3. Visa considerations (for IMGs)
If you’re on a visa (J-1, H-1B), Step 3 timing can affect:
- Visa category eligibility (especially H-1B often needs Step 3)
- Timing of applications for future positions
This is one situation where earlier is often better — but that still doesn’t mean pre-residency is smart. It just means don’t push Step 3 into late PGY-2/3 if your immigration lawyer is telling you it’s needed earlier.
How to Pick Your Exact Timing: A Simple Framework
Let’s be specific. Here’s a straightforward decision process.

| Step | Description |
|---|---|
| Step 1 | Check Program & State Rules |
| Step 2 | Target Window: Late PGY-1 to Mid PGY-2 |
| Step 3 | More Flexibility |
| Step 4 | Identify 1-2 Light Rotations |
| Step 5 | Plan Earlier in Window |
| Step 6 | Allow Extra Study Time |
| Step 7 | Schedule 2-3 Months Ahead |
| Step 8 | Deadline <= PGY-2? |
| Step 9 | Recent Step 2 CK? |
Now translate that into a concrete plan.
Step 1: Map your actual schedule
Look at your full year:
- Mark all brutal blocks: ICU, heavy wards, trauma, nights, q4–q5 call.
- Mark all lighter blocks: electives, outpatient-heavy months, research, consults.
- Pick 1–2 target months where you could realistically study 1–2 hours most days.
Step 2: Anchor your exam within a 6–8 week study window
Backwards-plan from an ideal test date:

| Category | Value |
|---|---|
| Week 1-2 | 8 |
| Week 3-4 | 10 |
| Week 5-6 | 12 |
| Week 7-8 | 12 |
- Week 1–2: Light warm-up (a few blocks of questions, CCS orientation)
- Week 3–6: Main question bank push + serious CCS practice
- Week 7–8: Review weak areas, second practice test, fine-tune timing
If your rotation is moderate (not golden but not malignant), this is sustainable.
Step 3: Be realistic about your bandwidth
Ask yourself:
- On your worst day of that rotation, can you still do 10–20 questions?
- Can you carve out 1–2 longer weekend blocks for full practice sessions?
- If you had a 10–12 hour call or long day, will you still have mental energy for any studying at all?
If you’re honest and the answer is “no way,” that month is not your Step 3 month. Don’t lie to yourself here. Residents who do that end up rescheduling 3 times and paying fees.
Special Situations: By Specialty and Scenario
Surgical, OB/GYN, EM residents
You have:
- Higher physical fatigue
- More shift work/night work
- Often worse continuity with clinic
Strategy I’ve seen work:
- Aim for an elective, research block, or slightly lighter rotation during PGY-1 or early PGY-2.
- Accept that “perfect timing” doesn’t exist, and pick the least bad month.
- Schedule early in that rotation before fatigue piles up.
Residents aiming for competitive fellowships
Think cards, GI, heme/onc, some subspecialties in surgery, etc.
You want Step 3:
- Done and passed by the time ERAS opens for fellowship (mid-PGY-2).
- Ideally with no hint of marginal performance.
So for you, the window is realistically:
- Late PGY-1 → early-mid PGY-2
Not later.
Those who struggled with Step 1/Step 2 CK
If your prior scores were marginal or you barely passed, you can’t just wing Step 3 “whenever you feel like it.”
For you:
- Earlier isn’t automatically better.
- You need:
- A true light block
- A structured study plan
- Enough time to do a full pass of a Qbank (UWorld, etc.)
I’d still keep you before late PGY-2, but I’d prioritize a strong rotation choice and extra study time over rushing it.
Quick Reality Check: How Much Does the Exact Month Matter?
Short answer: far less than people pretend.
What matters more:
- Are you reasonably prepared?
- Are you not actively drowning clinically that month?
- Are you not at risk of missing a program/visa/state deadline?

Residents love to obsess about whether June vs July is better. Truth: both are fine if:
- You pick a lighter rotation
- You have 6–8 weeks of semi-consistent studying
- You protect at least a few evenings and weekend blocks
One Concrete Example: Internal Medicine Resident
Let’s say:
- You’re IM PGY-1
- You want cards fellowship
- Your schedule:
- July–Aug: Wards (brutal)
- Sept: Night float
- Oct: Outpatient clinic + half-day didactics
- Nov: ICU
- Dec: Wards
- Jan: Elective (renal consult)
- Feb: Wards
- Mar: Clinic-heavy month
- Apr: Cards consults
- May: ICU
- Jun: Wards
Your best targets:
- January elective
- March clinic-heavy month
You’d:
- Decide: “I’m taking Step 3 in late February or early March.”
- Start light Qbank work in December (even during wards — 10–15 questions on off days).
- Ramp up during January elective.
- Take the exam near the start of March clinic month while knowledge is fresh and rotation is still controllable.
That’s how you make this concrete instead of theoretical.
Key Takeaways
- Best general window: Late PGY-1 to mid PGY-2, during a lighter rotation, after you’ve built real clinical experience but before deadlines and burnout collide.
- Don’t wing the month: Look at your actual schedule, identify 1–2 genuinely lighter rotations, and anchor a 6–8 week study window there.
- Program/visa/state rules win: Whatever theoretical “ideal timing” you’ve heard means nothing if it conflicts with real deadlines. Start with those constraints, then optimize within them.
FAQ (Exactly 5 Questions)
1. Is it bad to take Step 3 during intern year?
Not automatically. If you have a genuinely light outpatient or elective month and your Step 2 CK knowledge is still strong, intern year can be a great time. It’s bad when people cram it into a brutal ICU/wards month and half-study out of guilt. The problem isn’t “intern year,” it’s stacking the exam on top of a miserable rotation.
2. Do fellowship programs care when I take Step 3 or just that I passed?
Most care mainly that you’ve passed before you start or sometimes before they rank you. Some competitive fellowships like seeing all boards done on time and cleanly, but they’re not usually nitpicking your exact month. What does look bad is failing Step 3 or scrambling to take it last minute right before fellowship starts.
3. How long should I study for Step 3 as a resident?
For most people: 6–8 weeks of consistent-but-modest studying is enough, assuming you’re coming in with reasonable Step 2 CK performance and active clinical work. That typically means most days doing 10–20 questions and one or two longer blocks on weekends, plus CCS practice. If you barely passed Step 2 or have been out of clinical work, budget more time.
4. Should I separate my Step 3 exam days or take them back-to-back?
If your schedule allows, I’d do back-to-back days. You’re already in test mode, you don’t have to ramp up twice, and you rip the bandage off faster. If you’re on a rough rotation or easily fatigued, separating by 1–3 days can help you rest and review CCS, but don’t stretch it more than that unless your schedule forces you to.
5. What if my program hasn’t said anything about Step 3 timing — can I just wait?
You can wait, but that doesn’t mean you should. A silent program doesn’t protect you from state licensing timelines, future job requirements, or the pain of studying while you’re a senior with much more responsibility. If no one’s giving you guidance, create your own rule: aim to have Step 3 done by mid-PGY-2 unless you have a very specific, defensible reason not to.






















