
If My Goal Is Private Practice, Does Academic Training Still Make Sense?
What if you know you want private practice, but the strongest programs on your interview list are academic? Are you about to waste three–seven years training for a career you’re not going to have?
Here’s the blunt answer: yes, academic training can absolutely still make sense for a private practice career. But not always, and not at any cost. You need to be specific about what “private practice” you actually want—and what flavor of “academic” program you’re considering.
Let’s unpack this like adults, not brochure writers.
First: What Do You Actually Mean by “Private Practice”?
People use “private practice” to mean totally different things. Before you pick “academic vs community,” get clear on which bucket you’re in:
Common versions of “private practice”:
Traditional small-group or solo practice
You and a few partners, maybe independent, maybe part of a larger group.
You care about: efficiency, procedural skills (if procedural specialty), community reputation, financial literacy, autonomy.Large multispecialty group / employed practice
Think Optum, Kaiser, big health system clinics. You’re “private practice style” but employed.
You care about: being well-trained, not needing tons of hand-holding, being fast and safe on day one.Niche/high-end or procedural-heavy practice
Aesthetic derm, interventional pain, ortho sports, advanced GI, etc.
You care about: name recognition, fellowship access, technical skill, referrals.
Your ideal environment dictates whether an academic pedigree helps a lot, a little, or not at all.
Academic vs Community Programs: What Actually Differs?
Strip away the marketing. The key differences that matter for a private practice future are:
| Factor | Academic Program | Community Program |
|---|---|---|
| Case complexity | Higher on average | More bread-and-butter |
| Fellowships access | Usually stronger | Variable by program |
| Autonomy early | Often less early | Often more, earlier |
| Name recognition | Often higher | Mostly local/regional |
| Lifestyle in training | Often worse | Often better |
Academic programs usually give you:
- More complex, rare, “zebra” cases
- Bigger teams, more layers (student → intern → resident → fellow → attending)
- Easier access to competitive fellowships
- Some name-brand credibility on your CV
Community programs usually give you:
- Tons of bread-and-butter disease you’ll see daily in private practice
- More direct attending contact, often more hands-on early
- Often better lifestyle and call schedules
- Stronger exposure to real-world systems you’ll actually work in (billing, hospital politics, throughput)
Neither is “better for private practice” in a vacuum. It depends what you want to do after residency.
When Academic Training Is a Strong Yes for Private Practice
There are situations where academic training is not just “fine,” it’s arguably the smarter path—even if you’re never going to hold a faculty title.
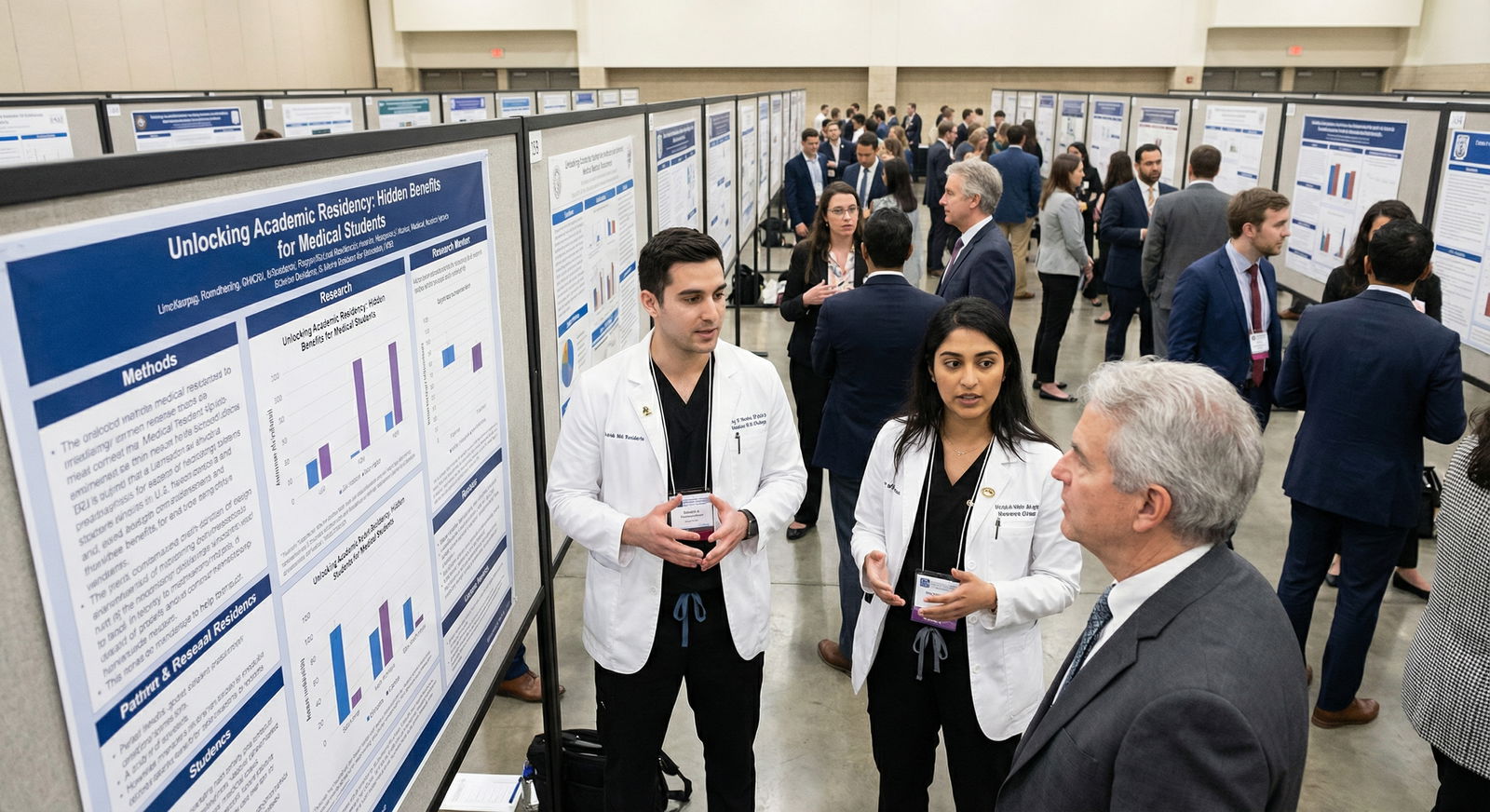
1. You’re Aiming for a Competitive Fellowship
If your route to private practice runs through a competitive fellowship, academic training often makes more sense.
Think:
- Dermatology (for later cosmetic focus)
- Ortho subspecialties (sports, spine, hand)
- GI with advanced endoscopy
- Cards with EP or interventional
- Interventional radiology
- Certain heme/onc niches
Academic residencies usually have:
- More in-house fellowships
- Stronger connections to fellowship directors
- Research infrastructure if your field still quietly cares about it
- More complex cases to talk about on interviews
Private practice groups love fellowship-trained specialists from recognizable places. The name on your badge does sometimes matter.
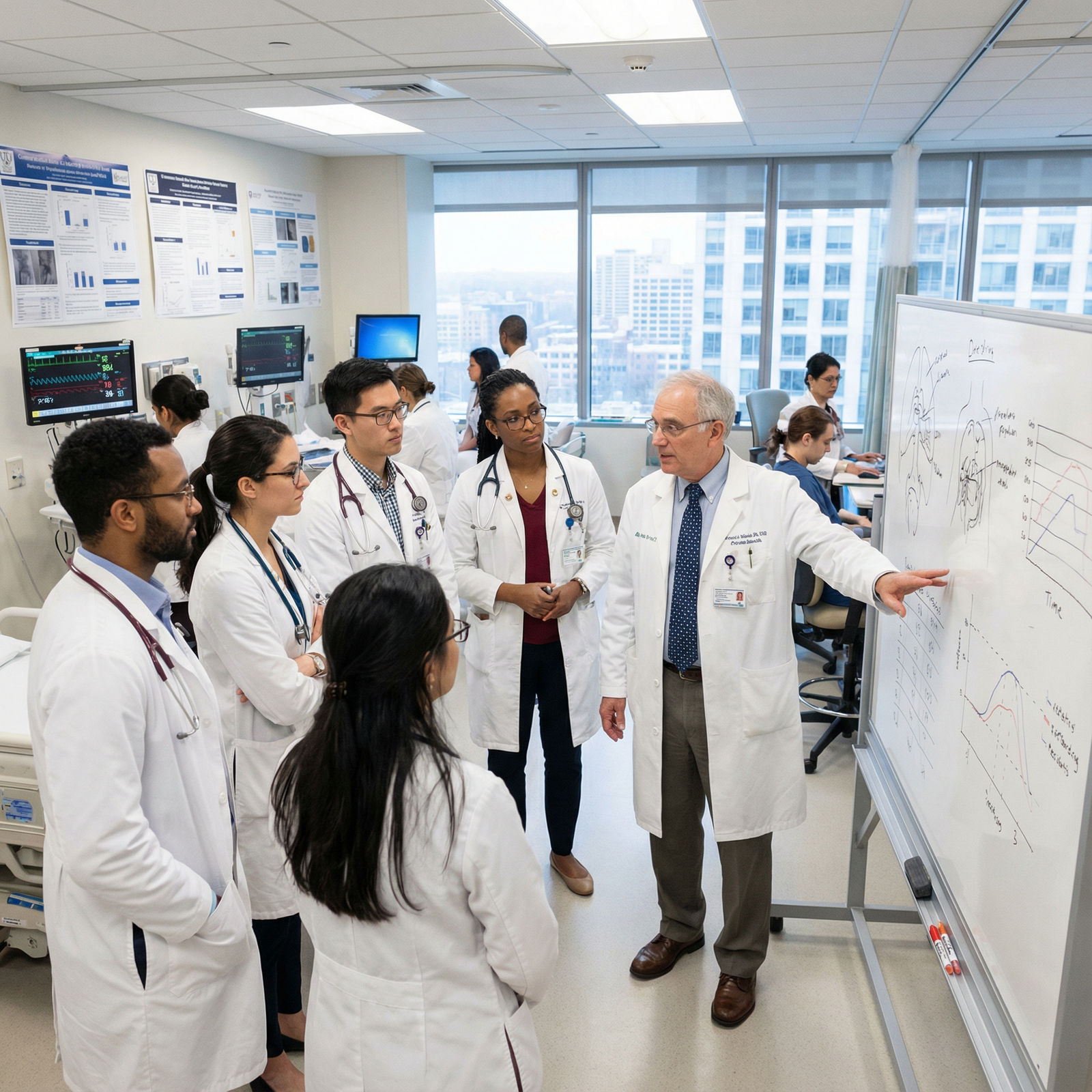
2. You Want to Be Technically Excellent in a Procedural Field
If you plan to live or die (financially) by your procedures, high-volume academic training can be a huge edge.
Example:
A busy academic GI program where you’re scoping all day, handling ERCPs/EUS, complicated bleeds, IBD, etc… That directly translates into:
- Confidence with tricky cases in private practice
- Comfort being “the expert” in your region
- Higher procedural volume and revenue potential later
Same story for ortho, ENT, IR, anesthesia, OB/GYN, etc. Deep exposure during residency often beats a lighter caseload at a sleepy community program.
3. You’re Considering a Niche/High-End Practice
If you want to do cosmetic derm in a major city, advanced heart failure in a large cardiology practice, or complex spine in a surgical group, then:
- Brand-name academic training can help attract referrals
- Your partners may care where you trained
- Patients may actually recognize the institution
You don’t need a big name. But when your future business model depends on being “the expert,” academic pedigree is a useful signal.
4. You Want Options (Even if You Think You Won’t Change Your Mind)
Here’s something I’ve watched over and over:
- MS4: “No way I’m doing academics.”
- PGY-2: “Huh, this research thing is kind of interesting.”
- PGY-3: “I kind of like teaching. Maybe 50/50 private–academic?”
Academic residency keeps doors open:
- Easier to go academic → private than the reverse in some specialties
- Easier to get hired in hybrid models (large groups with academic affiliations, teaching hospitals with private groups, etc.)
If you’re even 10–20% unsure, leaning academic can be insurance.
When a Community Program Is the Better Bet for Private Practice
Now, the other side. There are plenty of cases where chasing an academic badge just doesn’t make sense.
1. You’re Going Straight into General Private Practice
If you’re planning:
- General internal medicine or hospitalist
- Outpatient family med
- General peds
- General OB/GYN with no subspecialty push
- General anesthesia without a heavy academic niche
Then a strong community program can be ideal.
Why?
- You’ll see exactly the pathology mix you’ll see in practice
- Often more independence managing patients without five consultants
- Sometimes better exposure to billing, coding, and throughput
- You may train alongside or under the very group you’ll later join
I’ve seen plenty of residents slide straight from a community residency into a local private group—as a known, trusted quantity.
2. You Value Lifestyle and Sanity During Training
Academic powerhouses are not famous for chill schedules. If you know you:
- Care a lot about work–life balance
- Have a family or serious geographic constraints
- Are prone to burnout and don’t want a pressure-cooker –
Then a well-run community program might give you:
- More humane call schedules
- Less competition with fellows for procedures
- More continuity with attendings who’ve been there for years
Burning yourself to ash at a big-name program is not “worth it” just to land in regular outpatient IM.
3. Your Target Market Is Local/Regional, Not Prestige-Driven
If you know you’re going back to your hometown or a specific region:
- The local community program name may mean more to your future patients and employers than some faraway academic giant
- Local attendings often have deep ties to regional private groups and can open doors
Private practice hiring often looks like:
“Who do we know? Who did Dr. X train? Who rotated with us? Who seems easy to work with?”
That favors community programs integrated into local systems.
4. You Want Early Hands-On and Autonomy
Many community programs:
- Let you be primary operator earlier
- Have fewer fellows to compete with
- Force you to learn to work more independently (within reason)
If your main goal is to be comfortable running your own list, your own clinic, your own OR block—early autonomy matters more than a fancy logo on your diploma.
How to Decide: A Simple Framework
You’re choosing programs now, not signing a blood oath. Use this framework instead of getting lost in labels.

| Category | Value |
|---|---|
| Fellowship access | 80 |
| Procedural volume | 70 |
| Lifestyle | 60 |
| Local ties | 65 |
| Prestige | 40 |
Ask yourself three questions:
1. Do I need a competitive fellowship to do what I want in private practice?
- Yes → Strong preference for academic or very fellowship-connected hybrid programs
- Maybe → Mix of academic and strong community with in-house fellowships
- No → Community is totally valid, sometimes preferable
2. Where do I want to practice geographically?
- Very specific region → Weight local program reputation more than national prestige
- Open nationwide → Bigger academic names may travel better
3. What’s my tolerance for pain in residency?
Be honest.
- I’m fine grinding harder now for more options later → Academic (or high-powered hybrid) is reasonable
- I want solid training but not a martyrdom arc → Strong community or mid-tier academic
If you answer these cleanly, the choice tends to sort itself out.
Red Flags and Green Flags to Watch For
Forget “academic vs community” labels for a minute. Look at how each program actually trains you for real-world practice.
Green flags for private practice prep
- Graduates easily get the jobs you want (ask where last 5–10 ended up)
- Attendings are actively in or closely tied to private practice groups
- You get early and repeated exposure to outpatient settings (for clinic-focused fields)
- You’re doing the bread-and-butter procedures your future job will expect
- Residents say: “I feel ready to practice on my own”
Red flags
- Everything is ultra-tertiary/rare, with very little bread-and-butter
- Residents say they feel “book smart but not clinic/OR ready”
- Program leadership is openly dismissive of private practice (“sell-out” jokes, etc.)
- No one can tell you where grads went in terms of private practice vs academics
How to Talk About This on Your Application and Interviews
You don’t need to pretend you want a Nobel Prize to match an academic program. But you do need to sound coherent.
For academic-leaning programs, something like:
“Long term I see myself in a high-volume private practice with a strong clinical focus, possibly after a fellowship in X. I’m drawn to your program because of the case complexity, strong fellowship placement, and opportunities to teach and refine my skills so that I’m truly independent and capable when I join a group.”
For community-leaning programs:
“I’m aiming for a career in community-based private practice. I like that your program emphasizes direct patient care, continuity clinic, and working closely with attendings who practice in the same settings I hope to join after graduation.”
You’re not lying. You’re aligning your goals with what they actually offer.
Quick Reality Check: My Take
If I strip everything down:
- If you need a competitive fellowship or want a high-skill procedural niche → Academic or academic-leaning hybrid usually wins.
- If you want straightforward general private practice, in a specific region, with a reasonably good life during training → Strong community is often your best move.
- If you’re unsure and can tolerate some extra grind → Academic keeps more doors open.
The dumbest move is picking purely on label. The smartest is asking: “Will this place make me the kind of doctor a private group would happily hire and trust with their patients?”
Focus on that.
FAQ (Exactly 5 Questions)
1. Will an academic residency hurt my chances of going into private practice?
No. If anything, it often helps. Groups like residents who are well-trained, comfortable with complex cases, and come from programs with solid reputations. The key is that you still need enough exposure to bread-and-butter cases and outpatient/procedural volume, not just zebras and consults.
2. Can I get a competitive fellowship from a community program and still end up in private practice?
Yes, but it’s more variable. Some community programs have excellent fellowship match rates, especially if they have in-house fellowships or strong academic affiliations. Others send very few people to top fellowships. You have to look at each program’s actual fellowship match list, not the label on the website.
3. Do private practice groups really care where I trained?
Some do, some don’t. For routine outpatient IM or FM in a smaller town, they usually care more that you’re competent, pleasant to work with, and licensed in that state. For high-end subspecialty practices in competitive markets, training pedigree and fellowship (plus who knows you) start to matter more.
4. If I’m sure I don’t want research, should I avoid academic programs?
Not automatically. Many academic programs are perfectly fine with clinically focused residents who do minimal research. What you should avoid is a heavily research-obsessed program that expects multiple publications and grants from everyone. Ask residents how they balance clinical vs research time and whether clinically oriented people are supported or sidelined.
5. What’s the biggest mistake applicants make when choosing between academic and community programs for private practice goals?
They chase prestige or location blindly and ignore the day-to-day training reality. They don’t ask where graduates actually end up, how comfortable they feel to practice independently, or what the procedure/clinic volume is like. Your future private practice competence comes from what you do for 3–7 years, not just the logo on your white coat.
Key points:
- Academic training absolutely can make sense for private practice, especially if you want fellowship, complex skills, or optionality.
- Strong community programs are often better for straightforward general private practice, sane lifestyle, and local job connections.
- Ignore the label—pick the place that will make you the kind of physician a private group is excited to hire and trust.




















